In the case of bilateral subluxations, the mandible is displaced towards the larynx and breathing is difficult, especially in the supine position.

- Hip dysplasia in children - advanced methods of diagnosis and treatment
- What is hip dysplasia?
- Definition of the disease. causes
- Symptoms of a spinal subluxation.
- Types of X-ray examination in trauma care
- preparation and execution
- Restrictions on taking x-rays
- How should I prepare for the examination?
- Endoprosthetics of the shoulder joint
- Fracture reduction with bone grafting
- Video about our orthopedic and trauma surgery clinic
- X-ray findings of the foot in two projections
- General information
- The most common mistakes radiologists make
- Diagnosis of Cervical Subluxation (Atlas)
- prognosis and treatment
- Surgery for temporomandibular joint subluxation
- Rehabilitation after surgery
Hip dysplasia in children - advanced methods of diagnosis and treatment
Advanced diagnostic and treatment methods are being developed at the Turner Science and Research Center for Pediatric Traumatology and Orthopedics. The Turner Scientific and Research Center for Traumatology and Pediatric Orthopedics develops and applies advanced methods of treating hip pathologies in children. The specialists deal with the most unusual and serious cases, treating children not only from all regions of the country, but also from abroad.
Surgical treatment is carried out within federal borders within the framework of specialized and state-of-the-art medical care, free of charge for patients up to the age of 18 from all regions of Russia.
Employees of the only special department for hip pathology at the GI Gorky Research Institute of Traumatology and Orthopedics. Modern techniques of conservative and surgical treatment of children with hip dysplasia of various degrees are successfully used in the Turner Center.
- According to international studies and statistics of our center, this congenital pathology affects 5-10 children per 1000 newborns.
- Girls are affected about 7 times more often than boys. Unilateral lesions are 1.5-2 times more common than bilateral lesions.
- In adults, in one out of three cases, the pathology causes coxarthrosis.
What is hip dysplasia?
Hip dysplasia is a serious pathology characterized by underdevelopment of all components of the hip joint (bones, ligaments, joint capsule, muscles, blood vessels and nerves).
The modern term for this pathology is developmental dysplasia of the hip joint, that is, developmental dysplasia of the hip joint that occurs during pre- and postnatal ontogeny and can include neonatal instability, isolated underdevelopment of the acetabulum, subluxation and hip dislocation - the most severe degree of hip dysplasia, which is characterized by complete separation of the articular surfaces of the femoral head and acetabulum.

Definition of the disease. causes
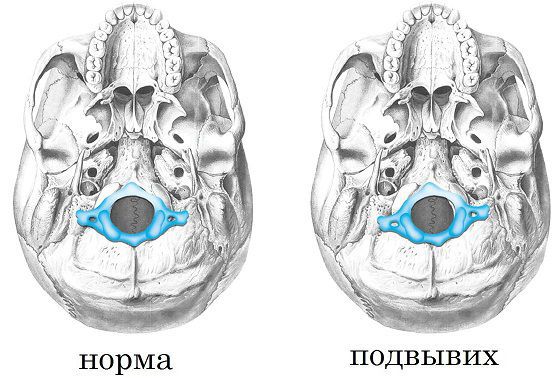
Vertebral subluxation (subluxation of the vertebrae) – is an abnormal displacement of one vertebra relative to the other, with the articular surfaces of the vertebrae remaining in contact. Subluxation is an incomplete displacement. Unlike subluxation, torsion involves a complete loss of contact between the joint surfaces, preventing movement.
Watch the video for a summary of the article:
Subluxations are most common in the cervical spine, less common in the lumbar and thoracic spine. There are no intervertebral discs between the vertebrae of the upper cervical spine. The occipital bone and the two upper vertebrae (atlas and axis) are connected only by ligaments that are less resistant to mechanical injury than the underlying vertebrae, which are tightly connected by cartilaginous pads - intervertebral discs. Due to these anatomical conditions, subluxations of the atlas occur and are more common than other subluxations.
Cervical subluxations can have the following causes, among others.:
- Damage to the ligament apparatus (shocks, falls from heights, sudden uncoordinated movements during strenuous physical work, sports games, headstands, somersaults, etc.).
- Birth-related injuries to the neck often lead to cervical subluxations in children;
- Neck muscle weakness in children contributing to subluxations from sudden, uncoordinated movements; [2].
- congenital connective tissue defects associated with hypermobility of the joints (Morcchio syndrome, Ehlers-Danlos syndrome, etc.);
- inflammatory processes in the spinal joints – rheumatoid arthritis, Grisell’s disease, etc. [1]
Causes of lumbar subluxations include:
Symptoms of a spinal subluxation.
Symptoms of acute cervical vertebral subluxation due to trauma:
- Acute pain in the neck;
- forced posture of the head by bending forward or to the side;
- Impaired movement of the cervical spine;
- swelling and acute pain on palpation;
- tinnitus, dizziness;
- feeling of goosebumps on the hands;
- Decreased strength and range of motion in the arms.
Long-term, previously undiagnosed vertebral subluxations are much more common.
- Neck pain of varying degrees of severity, arising from violent movements or a prolonged awkward position at work or when sleeping on a high pillow;
- Headaches that occur simultaneously with neck pain and are aggravated by pressure on the suboccipital muscles of the neck. The pain occurs mainly in the back of the head and forehead;
- Unilateral or bilateral restriction of movement of the neck;
- dizziness, ringing in the ears, deterioration in hearing and vision, impairment of autonomic function; [5].
- Traumatic thoracic subluxations are characterized by pain in the sternum, ribs, and abdomen. In traumatic lumbar subluxation, there are complaints of pain in the lower back, which increases with movement, sometimes inability to move, loss of sensation and strength in the lower limbs, abdominal and kidney pain, and dysfunction of the pelvic organs;
- Paresis and paralysis of the lower limbs can occur with spinal cord and root damage. [7]
When vertebral subluxation is accompanied by disc abnormalities, lower back pain gradually develops. They worsen with prolonged standing, bending, and heavy lifting. The pain radiates to the sacrum, coccyx, pelvis and lower limbs. On examination, there is a clear strain (contracture) of the lumbar muscles in the form of a limited forward tilt of the body. The contraction of the hamstrings causes the legs to bend at the hip and knee joints. There may be a change in the gait pattern.
Types of X-ray examination in trauma care
The type of X-ray examination of the bones and joints depends on the clinical symptoms and diagnostic needs and may include an isolated examination of a single joint or bone:
- X-rays of the elbow, wrist, knee and hip joint;
- X-rays of the hand and foot, fingers;
- X-rays of the sternum and collarbone;
- X-rays of the pelvic bones;
- X-ray of the sacroiliac joint;
- X-rays of long bones (thigh bones, humerus bones, etc.).
X-rays of bones and joints primarily enable the diagnosis of fractures, broken bones, joint dislocations and subluxations, and ligament injuries. And also joint and bone diseases, secondary bone and joint diseases, occupational changes and nutritional abnormalities.
X-rays of bones and joints do not always show pathological changes. There is a so-called 'radiographic period' when the lesion affects only the soft parts of the musculoskeletal system that cannot be seen on the x-ray. In this case, the usual radiological examination can be supported by more accurate methods: computed tomography (CT), magnetic resonance imaging (MRI).
Temporomandibular joint. X-rays of this joint are widely used in dental practice and oral surgery. They allow the diagnosis of diseases and injuries of the joint. The doctor also uses the data to identify bite problems. The image of the jaw allows conclusions to be drawn about the volume and structure of the bone tissue and is required for planning orthopedic treatments and dental implants.
shoulder joint. If there is a suspicion of periarticular inflammation of the shoulder, tumors, inflammatory and degenerative processes, fractures and dislocations, an X-ray may be required. It also allows for visualization of the clavicle and scapula.
preparation and execution
No special preparation is required. The patient is placed on a special table, and the groin area is protected with a lead apron. In children, additional protection is provided for the thyroid gland and eyes, and the infant is completely covered with an apron, leaving only the limb exposed.
An image of the joint or bone can be captured in one or more projections. In order to get accurate data, it is important that the child lies still. The examination only takes a few minutes. The doctor can immediately see the condition of the tissue and after the procedure receives a report with a protocol.
Excessive body weight can be an obstacle - fat cells distort X-rays. This results in the image not being clear enough. In this case, the doctor will suggest alternative examinations. Sometimes it is possible to solve the problem by capturing images from multiple projections. Some illnesses and injuries require only direct projection, while others require lateral projection to both sides. Sometimes a combination of several options is used. This gives the most accurate picture of the condition of the bone tissue.
Patients who need an X-ray of the joints often ask about the harm of the procedure. Radiation exposure in this type of diagnosis is minimal when modern equipment is used. The ViTerra Clinic uses modern X-ray machines with minimal radiation. X-rays are taken quickly, which reduces the stress on the body. An X-ray of the knee joint, for example, results in a radiation dose of 0.001 mSv - almost as much as a person absorbs every day in their everyday activities. Therefore, after 2-4 weeks, the X-ray can be repeated to assess the effectiveness of the prescribed treatment or the dynamics of tissue healing.
Restrictions on taking x-rays
With modern equipment and minimal radiation dose, X-ray examination of the foot is a safe procedure. There are no absolute contraindications to conducting the examination.
- The patient is in poor condition if they are unable to assume the correct position for a plain x-ray or stress test;
- if he has received a high dose of radiation within the past year;
- open wounds in the examined area with bleeding.
During pregnancy and lactation, X-rays are performed when there are strict indications. It is necessary to wear a protective apron covering the abdomen and mammary glands.
If an X-ray examination is not possible, an ultrasound or MRI examination of the foot is recommended.
How should I prepare for the examination?

No special preparations are required. The patient must appear at the clinic on the agreed date and bring their passport, insurance certificate, an extract from their medical records or a referral, and the results of previous tests.
The presence of pins and metal plates does not constitute a contraindication to X-ray examination of the foot.
Endoprosthetics of the shoulder joint
An endoprosthesis is indicated if the dislocation lasts longer than six months or if the impingement defect is more than 45 %. Replacement of the shoulder joint in chronic dislocations is judged to be more difficult than in normal osteoarthritis due to periarticular soft tissue destruction and damage to the articular surfaces. In these cases, total or reversible arthroplasty is performed.
In all cases, the patient is sedated for 4-6 weeks. We typically use an orthosis to keep the shoulder in neutral rotation during this time. Immobilization is followed by a rehabilitation phase that includes passive and active movement of the joint and strengthening exercises.
Fracture reduction with bone grafting
Consists of immobilization with an abduction splint for 6 weeks. The rest of the time, passive, careful flexion and extension of the shoulder is allowed. After immobilization, the patient is allowed to move the limb actively. In the first 12 months it is advisable to avoid heavy lifting.
The rehabilitation time after an endoprosthesis depends on the condition of the soft tissues. As a rule, movement of the shoulder joint is possible immediately after the operation.
If you have joint problems. When every movement causes you pain. We can help you. The clinic has state-of-the-art medical equipment that allows us to perform a wide range of surgical procedures on bones and joints.
Most joint operations in the clinic are performed endoscopically, ie through a small incision. The clinic is equipped with special recovery rooms where anesthesiologists monitor and treat patients after major surgeries.
However, the clinic not only performs highly technical surgical interventions, but also actively uses conservative methods to treat and rehabilitate patients without surgery.
The clinic offers patients the best possible conditions. Our doctors are professionals who put your health first. The doctors in our clinic are professionals who put your health first. Make an appointment today and come to our clinic for a consultation, we will definitely help you.
Video about our orthopedic and trauma surgery clinic
X-ray findings of the foot in two projections

The description includes the nature and severity of the findings. In private medical centers, the patient is given a plain x-ray and a digital x-ray, that is, an electronic storage medium, e.g. B. a floppy disk or a memory stick. The diagnosis is made by the attending physician.
General information
In the vast majority of cases, the initial diagnosis of a joint and spine disease is made after analyzing the patient's symptoms, medical history and examination data. However, later confirmation of the diagnosis is required by additional methods of examination: instrumental, laboratory and, less often, morphological. The gold standard for the diagnosis of joint pathologies is still the radiograph. X-ray is an important tool not only for diagnosing a specific joint inflammation or arthrosis, but also for assessing the course of the disease and the effectiveness of therapy.
A significant proportion of the patients referred to the provincial hospital had already been x-rayed at medical facilities in the region and needed evaluation at the provincial hospital. It should be noted that general practitioners are often guided by the descriptive elements of radiographs (protocols) provided to them by radiologists and do not assess some radiographic changes themselves.
And it's fine for these protocols to be created by a radiologist trained in arthrology and chiropractic, but based on their own clinical experience, radiologists often do not indicate on the X-rays the specific changes that allow the rheumatologist or therapist to make a differential diagnosis of joint injuries deliver. The phrase 'signs of arthritis' is quite common in the radiologist's report, but according to the literature, each type of arthritis may have its own specific signs to determine its nosological affiliation.
Therefore, in this article, we would like to focus on the most common errors in the radiological examination of rheumatic diseases and some of the most important and common radiological signs of joint involvement and their interpretation.
The most common mistakes radiologists make
Evaluating the experience of the rheumatology specialist at a provincial teaching hospital, we would like to point out the following of the most common errors in the use of X-ray diagnostics:
- Incorrectly selected scope of investigation
- Incorrect positioning of the patient during the X-ray examination
- Wrong interpretation of examination results.
The first step of the X-ray examination for the general practitioner should be the correct selection of the examination area, ie the area where the radiological changes are most revealing for the diagnosis of the disease in question.
For example, in recurrent attacks of gout, the clinical signs of pain and swelling may be most pronounced in the ankle joints while the metatarsophalangeal joints are unaffected, and it is a common mistake to give the patient an ankle x-ray, which is inconclusive in this situation is. The same applies if reactive spondyloarthritis or peripheral ankylosing spondylitis involving the ankles is suspected. Pathognomonic radiographic changes must be demonstrated in the sacroiliac joints and spine, while radiographic changes in the peripheral joints, particularly in the early stages of the disease, may not be present.
In general, x-rays of the ankle should be performed only rarely in isolated ankle disease and when specific (tuberculosis, gonococcal) arthritis is suspected due to their very low informative value and if there is a strict indication. This defect is associated with unjustified radiation exposure and additional patient costs for the repeat examinations required to clarify the diagnosis.
Diagnosis of Cervical Subluxation (Atlas)
The first vertebra of the cervical spine that supports the skull in an anatomically normal position is the C1 or atlantum. A subluxation of this vertebra is an abnormal displacement from the spine that can lead to neck injuries, poor blood flow to the brain, and dangerous symptoms.
When C1 is incompletely displaced, there is usually swelling in the neck, an inability to keep the head straight, and pain when the affected area is touched. When the atlas is displaced (subluxation) and the nerve roots or spinal cord are compressed, migraines, dizziness, trouble sleeping, and muscle spasms can occur. Loss of consciousness can occur.
Back and jaw pain, as well as tinnitus and an inability to move your arms and legs fully are common symptoms.

The clinical picture is more complicated when there is a congenital subluxation of the atlas. X-rays are not recommended because there are no markers that indicate a lesion. They appear after a few months when the child learns to stand up and walk. The gait of children with this pathology is unsteady and shaky. At the same time, they can develop attention deficit and be very gluttonous.
prognosis and treatment
The outcome of the injury depends on the cause and the general condition of the patient. Most cases have a favorable prognosis and do not require surgery.
To relieve symptoms, pharmacological treatment, physiotherapy, massage and physical therapy are prescribed. Treatment can be started as early as the first few days after injury to improve blood supply and muscle nutrition.
At the Doctor's Spine Center you can get advice on an incomplete dislocation and an x-ray of the neck in a cast, if any. The clinic's doctors conduct a comprehensive examination of the patient and draw up a treatment plan, which depends on the severity of the symptoms and the individual characteristics of the patient.
Surgery for temporomandibular joint subluxation
In most cases, the injury can be treated conservatively. A recurring subluxation of the temporomandibular joint is treated surgically. The interventions can be performed open or endoscopically. For example, the height of articular cartilage is increased by splitting it and placing a Teflon implant in the split. There is a method of deepening the acetabulum by changing the position of the disc from horizontal to vertical. In some techniques, part of the capsule is removed or reinforced with a strip of collagenous connective tissue. The exact type of operation is determined by the surgeon after a thorough examination of the patient and taking into account the specifics of each patient.
Take advantage of this unique opportunity and arrange a free consultation appointment for your planned intervention. Learn more.

Rehabilitation after surgery
Depending on the complexity of the operation, the patient must remain in the hospital under medical supervision for the first few days. Solid food should be eliminated from the diet after discharge from the hospital. Over time, the diet can be gradually expanded.
In the first few weeks after the operation, the mouth must not be opened wide and the lower jaw must be immobilized with special clamps and orthopedic splints. This is necessary to restore the function of the ligaments and joints.
Read more:- Inward subluxation of the foot.
- Anatomy of the heel bone x-ray.
- Subluxation of the ankle.
- Treated subluxation of the ankle.
- X-ray anatomy of the ankle.
- Legs of different lengths in a child.
- Anatomy of the foot x-ray.
- The child has a shorter leg than the other.
