The most common cause of pain in the back of the knee when bending is knee pain, but other illnesses can often be the cause. For an accurate diagnosis, you should visit a clinic that specializes in the treatment of the spine and joints. Do not hesitate to see your doctor because some diseases that cause leg pain below the knee require immediate surgical intervention.
- Tibia fracture
- Types of tibia fractures
- Symptoms of periostitis
- Causes of tibial periostitis
- What should you do if you have severe knee pain?
- How to treat knee and leg pain at home
- What to do if you have severe knee pain of a different kind?
- Knee pain after coronavirus and other viral diseases
- Severe pain under the knee
- How does Blount Erlacher's disease manifest itself in children?
- Treatment of Blount's disease
- Causes of Leg Bone Pain
- Bone pain in the legs when walking and at night
- Why do bones hurt so much after a fracture?
- How long does a bone hurt after a fracture?
- Symptoms of lower leg pain
- Rare causes of lower leg pain:
- Why does the front of the leg hurt below the knee?
- Causes of pain in the knee joint
- Causes of lateral knee pain
- Diagnosis of knee pain
- Treatment of knee pain
- Prevention of knee pain
Tibia fracture

A tibial fracture is a violation of the integrity of the tibia, sometimes occurring completely and sometimes partially when the load exceeds the strength of the bone. The injury is usually the result of a blow to the leg, e.g. B. from a clumsy jump, a fall from a height, a car accident, careless walking on the street in winter or extreme sports.
The shinbone is often injured due to its location and the lack of a layer of tissue. A fracture of the adjacent fibula is also not uncommon. The risk of such an injury increases in people over the age of sixty due to the structure of their bones. The bone becomes more brittle and porous, so even a small impact can cause a fracture. Young children are also susceptible to injuries due to their high level of physical activity. They are more likely to break this long bone without displacement or sharp fragments.
Types of tibia fractures
In traumatology, shin fractures are usually classified as follows:
- Fracture resulting in a small fragment that may be oriented vertically or horizontally;
- Fragmentary fracture, in which bone fragments are formed during the injury;
- Closed fracture in which the broken tibia does not penetrate the soft tissues;
- Open fracture, in which the integrity of the skin is compromised and the bone communicates with the external environment;
- The stress fracture is a characteristic injury to the shinbone. It occurs as a result of traumatic overexertion when the bone has already suffered minor fractures. Competitive athletes such as gymnasts and basketball players often injure themselves this way.
Symptoms of periostitis
The main symptom is localized pain in the area of the shinbone affected by the inflammation. As a rule, the area affected by the inflammation extends over 5-10 cm and the pain extends throughout the entire area, but can also be limited to certain areas.
At the beginning of the disease, the pain occurs with exertion and subsides with rest, but as the inflammation progresses, it becomes sharp and persistent, making movement difficult.
The inflamed area can cause the following. Redness, swelling and high sensitivity to touch. The pain worsens when bending and straightening the fingers.
Causes of tibial periostitis
As already mentioned, Shin periostitis (inflammation of the periosteum of the shin bone) is caused by inflammation of the connective tissue that lines the bone.
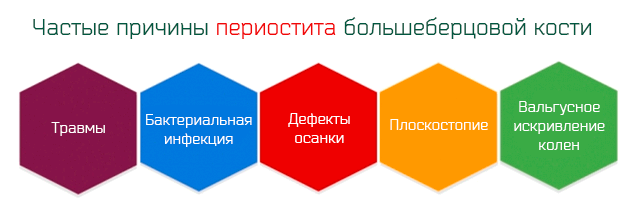
- A 'bacterial' infectionwhich normally reaches the periosteum via the blood. In this case, the inflammation of the periosteum is the result of a previous infection. However, this situation is very rare in our country.
- trauma. Much more often, periosteum inflammation is caused by trauma to the shinbone. Injuries result in microscopic tears that trigger an inflammatory process.
What should you do if you have severe knee pain?
Severe knee pain can come on suddenly or develop gradually. In both cases they often become unbearable. If severe pain occurs, you should take it easy and consult a doctor immediately. Everything is treatable and specialists can help even if the symptoms are neglected. If it is not possible to go to the doctor at the moment, you can relieve the pain yourself on an ad hoc basis.
However, it is important to remember that knee joint pain is a temporary measure that cannot be avoided when consulting a doctor. And it is better not to drag this matter out.
How to treat knee and leg pain at home
For severe knee pain, the following ad hoc measures can be used:
- Administer a painkiller in tablet form:
- Naise (Nimesulide) – if the pain is severe, take 1 tablet of 100 mg; this is an effective modern drug that belongs to the latest generation of non-steroidal anti-inflammatory drugs (NSAIDs) and has minimal side effects, including no adverse effects on the gastrointestinal tract (GIT); in acute inflammation, it not only relieves pain, but also reduces fever and reduces tissue swelling if the knee is swollen;
- Analgin – One 500mg tablet can be taken at once; it also reduces inflammation, swelling and pain. It is not advisable to use this medication excessively as it can cause serious blood disorders if taken too frequently.
- Pentalgine - A combination pain reliever containing two anti-inflammatory painkillers (paracetamol and naproxen), an anti-spasm reliever (drotaverine) and an antihistamine - helps if your knee is swollen. Take one tablet (no more than 3 to 4 tablets per day).
- Use external pain relievers (ointments, gels). The most effective of them are:
- Voltaren' emulsionActive ingredient: diclofenac; Properties of the drug: due to its structure, it is immediately absorbed into the skin, penetrates into the deeper layers of the skin, relieves inflammation, swelling and pain; the effect lasts for several hours; the ointment is applied to the skin in the knee area twice a day and rubbed in lightly;
- Menovazin – An alcoholic solution for external use with a combined formulation; Benzocaine and procaine have a local analgesic effect, menthol enhances this effect by dilating the skin vessels and causing a pleasant cooling sensation that reduces inflammation and fever; the solution is rubbed into the inflamed tissue and provides immediate relief;
- Dimethoxide gel – is an analgesic and anti-inflammatory agent that is applied to the skin 1-2 times a day; the gel has a quick healing effect; it also inhibits intra-articular hypertrophy of connective tissue, thus preventing the development of limb immobility; Contraindications: severe kidney, liver and circulatory diseases, pregnancy, breastfeeding.
What to do if you have severe knee pain of a different kind?
Knee pain can be of different types and durations. They can be constant and annoying or only occur during certain activities, at night, etc. For example, in some pathological processes the knee hurts when bending, in others when walking, etc. Only a specialist can understand what is going on, why it hurts and how to help the patient.
Knee pain after coronavirus and other viral diseases
Viral infections can cause arthritis. As a rule, these diseases develop on the background of an existing infection and resolve without sequelae. For example, influenza and other acute respiratory viral infections with acute fever can cause short-term joint and muscle pain or acute arthritis with inflammation and swelling of the knee joints. Its course is favorable.
Infection with coronaviruses is specific: it progresses differently from person to person. It is unknown why this happens. During the illness, annoying joint pain, swelling and redness sometimes occur - a sign of acute arthritis - but then subside again.
Arthritis, which sets in about a month after infection with the coronavirus, is even more dangerous. It has a significant impact on the immune system. Abnormalities in the immune system lead to the development of autoimmune processes. This is especially dangerous for people who have close relatives suffering from chronic arthritis. Experts say these patients are at high risk of developing rheumatoid arthritis (RA). The first symptom of RA is morning stiffness (difficulty bending the knee).
If arthritis occurs after recovery from a viral infection, you should immediately consult a rheumatologist.
Severe pain under the knee
This may be a symptom of a Baker's cyst. This is a stretched synovial sac with fluid in the tendon area. The cyst and the associated pain below the knee are due to it being connected to the knee joint cavity and filled with synovial fluid. The backflow of the liquid is hindered for various reasons. Most often, the cyst develops as a result of bruises, arthrosis of the knee joint.
How does Blount Erlacher's disease manifest itself in children?
Erlacher-Blount disease in children is manifested by a variety of symptoms that depend on the shape and degree of curvature of the limbs. The basic classification is based on the age at which the first clinical symptoms appear:
The infantile form begins between the ages of 3 and 5 and is characterized by symmetrical changes in the bone condyles of both legs;
The juvenile form is first diagnosed during puberty against the background of hormonal restructuring of the body and is characterized by the involvement of the tibia in one leg.
Blount's disease in children can cause varus or valgus curvature of the lower limbs to the following degrees:
- 15° curvature – potential;
- 16° to 30° curvature – moderate;
- 31° to 40° – progressive;
- Over 40° – progressing rapidly.
The general clinical signs are rapid fatigue of the calf and thigh muscles and compensatory claudication. The child tries not to put any strain on the affected limb while playing. When both limbs are bent, it spends most of its time sitting.
The duck gait is characterized by a significant degree of curvature of both limbs. The ligaments and tendons are weakened. Sprains, strains, dislocations, and torn ligaments and tendons are common even with minimal physical exertion.
After the age of 6, the child begins to lag behind the physiological norm. The arms and lower limbs appear disproportionately long and relatively short. Without proper treatment, muscle wasting, secondary flatfoot, or clubfoot occurs. The child may lose the ability to walk independently.
To diagnose the pathology, it is necessary to consult an orthopedic surgeon. After the doctor has examined you, x-rays are taken of the suspected deformed tibia and fibula. In the images, foci of bone and cartilage damage can be clearly seen.
Treatment of Blount's disease
Treatment for Blount's disease should be started as early as possible. In children with Blount's disease, the cortical growth plates close quickly. There is a risk that the development of the tibia and fibula will be significantly delayed. This will lead to external deformations in the future. That's why it's important to see an orthopedist as soon as possible at the first signs of a deformity.
The currently most effective method of bone reconstruction is the Elizarov apparatus. This means the osteosynthesis process can begin without surgery.
Manual therapy, osteopathy, massage, physiotherapy and remedial gymnastics are the primary and supportive treatment methods during the rehabilitation phase. Acupuncture helps initiate the regeneration process of bone and cartilage tissue. Gymnastics restores the tone of the damaged calf and thigh muscles. Massage and osteopathy improve tissue nutrition and accelerate the healing process.
Doctor of Medicine, Chief Physician
Causes of Leg Bone Pain
Only a doctor, after a physical examination and several tests, can explain exactly why your leg bones hurt. We will only look at the possible causes of these complaints. This can give you a rough idea of what might be going on with your health. This will help you make the right decision when choosing a specialist.
If you have suffered an injury (fall, bruise, sprain of the leg, involvement in an accident, fall from a height, etc.) on the eve of the appearance of this clinical symptom, you should immediately consult a trauma surgeon. This doctor will immediately take an x-ray and rule out the possibility of a broken bone or fracture.
Possible causes of constantly painful leg bones without traumatic impact can be the following diseases:
- osteochondrosis of the lumbosacral region, complicated by sciatica, radiculopathy and root syndrome;
- Protrusions, prolapses, extrusions and intervertebral fractures in the lumbosacral spine;
- Instability of the vertebral bodies and their periodic sliding relative to each other and to the central axis in the form of laterolisthesis, antelisthesis, retrolisthesis;
- Narrowing of the spinal canal, also as a result of a dorsal intervertebral fracture;
- Injury to the lumbosacral nerve plexus (plexitis, compression);
- Piriformis muscle syndrome (entrapment of the sciatic nerve when passing through a tunnel in it);
- Cauda equina syndrome (usually accompanied not only by pain in the lower limbs, but also by dysfunction of the pelvic organs);
- Circulatory disorders due to atherosclerosis, varicose veins, obliterative arteritis, vasculitis, diabetic angiopathy, etc;
- Entrapment of the sciatic nerve at its junction with the tibial and ankle branches;
- Deformed osteoarthritis of the hip, patellofemoral joint, knee, or ankle;
- Rheumatic cartilage damage to the large joints of the lower limbs (articular form of Bechterew's disease, systemic lupus erythematosus, rheumatic polyarthritis, etc.).
- Scarring deformations of the ligament and tendon tissue, which usually develop after traumatic sprains and strains;
- lesions of the menisci, joint capsules and joints;
- Osteoporosis, osteomalacia and osteopenia (these diseases are particularly dangerous in the elderly and menopausal women).
Bone pain in the legs when walking and at night
Women often complain of pain in the foot bones below the knee; An initial diagnosis provides insight into the problem causing the sensations. These include misalignment of the foot, wearing high-heeled shoes, deviation of the big toe, bones close to the joint, etc. All of these factors lead to serious damage to the musculoskeletal system. Cartilage degeneration occurs in large joints. As a result of compression, recurring inflammation occurs, which in turn causes pain syndrome.
If you have pain in your legs, you should first examine the foot, ankle and knee joints. Any abnormality in these structural parts of the lower limbs triggers the sensation. If you have to stand on your feet for a long time and your leg bones hurt at night, you should definitely check the condition of your circulatory system. This requires an ultrasound scan of the blood vessels in the lower limbs.
The leg bones hurt a lot when the foot is misaligned. Flat feet or clubfoot cause abnormal distribution of shock load. This can twist the tibial head in the knee capsule and put additional pressure on the meniscus. A plantogram can help identify the problem. This can be done by an orthopedist or chiropractor.
If your leg bone hurts when you walk, you should see an orthopedist or chiropractor as soon as possible. The doctor will examine you, take a medical history and order the necessary tests. X-rays, MRIs, CTs, ultrasounds, blood tests, etc. may be necessary.
Why do bones hurt so much after a fracture?
In reality, after a fracture, the bone only appears to hurt; In reality, the pain syndrome is caused by compression of the radial nerves in the periosteum and surrounding soft tissues.
The real reason why bones hurt after a fracture is the formation of a cavity where the integrity of the bone has been compromised. Capillary blood collects in the cavity, which is caused by ruptured blood vessels in the periosteum. Inflammatory factors are attracted to the area where the blood has pooled. These cause swelling of the soft tissues and increased local blood flow.
Other causes of pain syndrome:
- displacement of bone fragments;
- poor blood supply due to vascular diseases (varicose veins of the lower limbs, diabetic angiopathy, endocrine disorders, atherosclerosis, etc.).
- osteomalacia and bone structure disorders;
- Vitamin D deficiency;
- insufficient calcium and phosphorus salts in the body due to malabsorption or nutritional abnormalities;
- B vitamin deficiency.
Pain during rehabilitation can be associated with bone marrow degradation and deformities. An inappropriate course of rehabilitation can provoke re-damage to bone continuity. Therefore, the recommendations of the traumatologist and the chiropractor conducting rehabilitation should be strictly followed.
How long does a bone hurt after a fracture?
Why the bone hurts after a fracture was explained above. It is also important to know how long the bone hurts after a fracture and when this clinical symptom should completely disappear.
A broken bone heals within 40 to 60 days, depending on its complexity and location. Four phases can be distinguished in this process:
- First, fibrin, the main material that restores tissue integrity, collects blood and deposits proteins where bone integrity has been compromised;
- Second, the fibrin thickens and forms a soft scar, which then ossifies and turns into a bone callus;
- Third, osteoclasts and osteoblasts settle in large numbers in the fibrous scar, and the bone marrow hardens and fuses the fragments;
- Fourth, blood supply and innervation to the limb below the fracture site are restored.
The pain in the first stage is always associated with an inflammatory reaction. In the second, third and fourth stages, pain syndrome is a symptom of damage to nerve fibers or vessels.
Only an experienced doctor can determine the cause of pain in the long bones after a fracture. During the examination, diagnostic functional tests are carried out. These help to diagnose post-traumatic compression or tunnel syndrome, microvascular disorders with subsequent soft tissue necrosis.
For example, if a patient has suffered a broken tibia or fibula and is still in acute pain even after the cast has been removed, the doctor measures the pulsation wave on the inner crease of the foot. If the pulsation in the injured limb is reduced, it can be assumed that the large blood vessels have been interrupted during tissue fusion. The second examination concerns the tendon reflexes. If their intensity is reduced, the doctor may suspect a nerve fiber conduction disorder.
Symptoms of lower leg pain
Lower leg pain usually occurs below the knee on the outside of the leg (near the shinbone). The area affected by the pain is 10-15 centimeters long. The pain often occurs during physical exertion and subsides when you stop exercising. Typically, this pain is not serious, but if you experience pain while exercising, you should stop exercising.
- Decreased concentration of certain salts (calcium, sodium, magnesium, potassium) in the blood or dehydration.
- Taking medications: Statins can damage muscle tissue by lowering cholesterol levels, and diuretics can dramatically reduce salt concentrations in the body.
- Muscle cramps as a result of prolonged static stress or overexertion.
- Torn ligaments as a result of a muscle injury.
- Tibia fractures of the compressed type.
- Damage to the meniscus.
- Inflammatory processes in the tendons of the lower leg.
- Atherosclerosis of the blood vessels of the lower limbs (in this case, the pain usually occurs when walking and subsides after periods of rest).
- Deep vein thrombosis (blockage of blood vessels).
- Osteoarthritis, arthritis (inflammation of the joints).
- Infection of bone tissue (osteomyelitis).
- Inflammation of the tendon sheaths and tendons of the front and back thigh muscles (tendovaginitis/tendonitis).
- Damage to nerve fibers – polyneuropathy, which occurs in diabetics, alcohol abusers and smokers.
- Inflammation and damage to the Achilles tendon – partial macro and micro tears (retendinitis, tendinitis).
- 'Tethering' syndromes in the shinbone (pinch syndrome); posterior, anterior, lateral tibial muscle 'compartment' syndromes, anterior musculoskeletal fixator syndrome.
- Stress fractures within the tibia ('march', fatigue).
- Inflammatory processes in the periosteum of the shinbone – so-called periostopathy.
- Contractures ('congestions') of the lower leg muscles due to overloading.
- Macro and micro tears in the calf muscles.
- Dilatation of the lower leg and foot veins and lymphatic-venous insufficiency.
- Inflammation and microinjuries of the patellar ligament (perithedonitis, tendinitis, tendoperiopathy).
- Inflammatory processes of the tibial tuberosity: juvenile tenoperiostopathy of the growth zone (Osgood-Schlatter disease).
- Torn ligaments and sprains with ankle instability.
- Inflammatory processes at the tip of the kneecap ('jumper's knee', tendoperiostopathy).
Rare causes of lower leg pain:
- Newly appeared tumor in the lower leg or thigh – osteoma.
- Medications: corticosteroid and allapurinol.
- Osteosarcoma (malignant bone tumor).
- Paget's disease.
- Caused by herniated disc, compression of nerve roots.
- Tissue compression syndrome.
- Raynaud's syndrome.
Acute lower leg pain most often occurs in people who have not smoked for a long time. Rest helps to relieve the pain, but its occurrence indicates a health problem and signals the need for a change in lifestyle. In the presence of such a pain syndrome, it is also important to carry out the necessary examinations of the smoking patient to detect vascular and cardiac diseases.
Acute pain in the lower leg due to deep vein thrombosis is not dangerous, but there is a high risk of complications that can cause the thrombus to rupture and invade the lungs or brain. Sometimes thrombosis requires surgical treatment.
Atherosclerosis of the lower limbs causes symptoms very similar to those of tobacco users (Raynaud's syndrome). However, the two diseases are significantly different: atherosclerosis causes real narrowing of the blood vessels, in contrast to Raynaud's syndrome, which only causes spasms.
Tissue compression syndrome is a serious condition that occurs when the lower limbs are subjected to intense pressure. In some cases, bleeding occurs in the lower leg muscles, which compresses blood vessels and nerve fibers. As a result, the leg swells and becomes hot, and severe local pain occurs in the lower leg area. The most serious complication of the disease is damage to muscle and nerve fibers, which is usually irreversible. In this case, muscle loss and 'drop foot' (loss of foot function) can occur. As a result, the affected person loses the ability to flex the foot and therefore the ability to walk, cycle and swim.
Why does the front of the leg hurt below the knee?

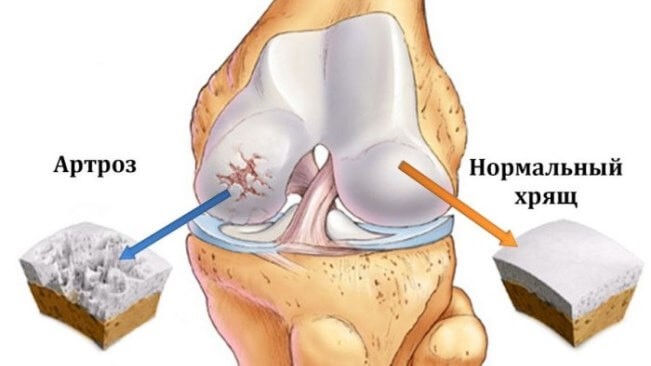
The knee joints are joints that are much more exposed to various mechanical factors than other joints. The reason for this is their location. Human legs are in motion every day, supporting not only the weight of the body, but also the loads carried by them. It is the knee joints that are the first to be affected by diseases such as osteoarthritis, arthritis, etc. In addition, problems can arise as a result of trauma caused by overuse or violent impacts. The disease is often diagnosed after a sprain or fracture.
'Therefore, it is important to see a doctor who will examine and identify the problem in order to treat it properly.

The conditions that cause pain below the knee can be different. Osteoarthritis in particular, which occurs more frequently in older people, sometimes also affects young people, usually after an injury. Athletes who frequently injure one part of their body are the most vulnerable. Overweight people and people with long lifespans also belong to this group, which is due to overwork.
In addition, this type of disease can occur in any person, especially if the problem is hereditary. Arthritis often occurs in the female family - researchers believe that it is a genetic predisposition, hormonal fluctuations at different times of life and, according to statistics and consequently, a large percentage of people suffering from joint pain and deformities - women.
One tip. A disease such as osteoporosis is characterized by a lack of calcium and vitamin D in the body and hypodynamics. It is therefore advisable to monitor the availability of these substances and supplement them if necessary. This is especially true for people who do not eat healthily, are prone to alcohol consumption and smoking, and have other bad habits.
Causes of pain in the knee joint
We often experience discomfort in one part of the body or another, but very often we attribute it to a recent bruise or simple fatigue. Pain is normal for humans, so all pain syndromes, especially mild and short-term ones, are simply ignored. Sometimes that's true - why bother the doctor unnecessarily? However, in some cases, it is very important to contact specialists in a timely manner in order to prevent the development of the disease and initiate treatment before the disease becomes chronic and worsens.
Why can the knee hurt?
- Injuries – simple bruises, sprains, fractures, sprains, strains, or other damage to the meniscus;
- overexertion after sporting activities;
- Inflammatory processes in or around the joint due to metabolic disorders (gout, fat and mineral disorders);
- Impaired immune responses of the body leading to arthritis, vasculitis, rheumatic diseases, psoriasis, etc.)
- Infectious processes in bone tissue, periarticular elements of the knee joint (brucellosis, irsinosis, etc.);
- Osteoarthritis or other degenerative diseases caused by increased, prolonged, irregular load changes;
- Diseases of the lumbar spine, motor deficits in neurological diseases - asymmetrical gait;
- Diseases of the hip, bone diseases of the foot and ankle.
So you have knee pain and can't decide whether to go to one of the following doctors Podiatristor whether you shouldn't worry too much about it. As you know, early detection prevents the problem from becoming chronic and allows for more gentle treatment.
There are several factors that should trigger a visit to the hospital:
- The pain may be mild but lasts for at least 5 days.
- There are other symptoms such as an increase in general and local temperature.
- The joint's mobility is restricted and severe swelling occurs.
- The joint becomes deformed.
- The pain increases when climbing or walking stairs.
Causes of lateral knee pain
There are many factors that can cause discomfort in a limb. The main causes of pain in the knee on the outside:
- Bruises. These injuries are more common in people who lead an active lifestyle. Depending on the severity of the impact and the object on which the person was hit, the pain may affect all or part of the knee joint.
- Injury to the external collateral ligament. It occurs when a person makes a violent inward movement of the shinbone.
- Damage to the patellar meniscus. A tear is possible with sudden bending caused by blows from the side.
- Gonarthrosis. Characterized by degenerative changes in cartilage tissue. When the shinbone and femur are affected, symptoms such as pain in the knee joint from the side often occur, especially when walking.
- Inflammation of the knee joint. If the knee joint is inflamed, the patient not only suffers from pain, but also from limited mobility of the lower limbs. Osteochondritis is caused by an infection that enters the joint through damaged skin.
- Osteochondrosis of the spine. With this disease, the pain often radiates to the hip or knee joint area.
- Broken bones.
Torn ligaments or sprains are a common cause of pain. Swelling and bruising are characteristic of these injuries. These injuries occur e.g. B. most often occurs when ice skating. Tendon ruptures are not uncommon in athletes over 40 who run or in young people who have received steroid injections in the knee joint area. One of the rare injuries that can cause this syndrome is a sprained knee. It is always preceded by a very strong impact. This triggers the injury:
When the kneecap is dislocated, pain sometimes occurs. This most often happens through a strong extension of the leg, e.g. B. during a jump. The risk of such an injury also exists in overweight people. Chronic knee pain on the inside and outside of the knee is often the cause:
Diagnosis of knee pain
If you experience discomfort when walking or bending your lower limbs, you should speak to your doctor. To find out the cause of your knee pain, you need to undergo a comprehensive diagnosis. After an initial examination, your specialist may recommend the following procedures:
Basic methods for diagnosing knee pain on the side outward:
diagnostic technique Time arthroscopy 60 minutes Ultrasound examination of the knee joint 30 minutes Radiological examination 10 mins Magnetic resonance imaging of the knee joint 30 minutes Treatment of knee pain
Once the diagnosis is established, your doctor will decide how to treat your knee pain. If the problem is caused by infectious or systemic inflammation (lymphadenitis, rheumatoid arthritis), the underlying disease is treated. In some cases, surgery is required. Operations are performed at:
- certain types of trauma;
- Thrombosis;
- abscesses;
- Gonarthrosis grade 3-4 (knee replacement);
- tumors.
In the postoperative period, the patient is prescribed anti-inflammatory and analgesic medications as well as an immobilizing bandage.
In case of inflammation, non-steroidal anti-inflammatory drugs are prescribed. If injuries occur, a cast or splint is placed on the injured area. Once the splint is removed, mobility of the knee joint is restored through therapeutic massage, exercises and physical therapy. Also, cartilage protectants are prescribed to slow down the degeneration of cartilage tissue, as well as in the non-triggered stages of gonarthrosis. The use of folk remedies can be used as complementary treatment only if approved by a doctor.
Prevention of knee pain
Risk factors include obesity, lack of exercise or excessive stress on the knee joints, frequent injuries and a hereditary predisposition to joint diseases. Maintaining the health of the knee joints can be supported by a healthy lifestyle. This includes:
- maintaining a healthy weight;
- an optimal level of physical activity, including strength and endurance training;
- a balanced diet;
- an adequate amount of sleep;
- hardening;
- avoiding injuries and overexertion;
- increasing stress tolerance;
- regular monitoring of blood composition and measures to correct deficiencies in important vitamins and minerals.
To prevent disability and life-threatening complications, it is important to seek medical attention at the first sign of discomfort or pain in the hamstring area.
- tibia and fibula.
- Why does the femur hurt?.
- Why do feet hurt after running?.
- Why does the galley muscle hurt?.
- The outer arch of the foot hurts, why.
- Why the legs hurt below the knees after running.
- ankle-shin.
- What is the connection between the femur and tibia?.
