The therapy usually achieves the best results when the child is still very young, because at this age the bones are not yet fully 'mature' and mineralized.

- osteoarthritis in the hands
- Causes of osteoarthritis in the hand
- What is Dupuytren's disease?
- Causes: trauma, heredity, etc.
- Signs and symptoms of clinodactyly
- Causes of crooked fingers in children
- Causes of joint deformations in fingers and toes
- Treatment of toe deformities
- Changes in the nails in isolated malformations
- Nail changes in ectodermal dysplasia
- classification
- differential diagnosis
- causes
- Types of anomalies of the fingers in children
- What is clinodactyly? Causes, diagnosis and treatment of clinodactyly in children
- diagnosis
- What is syndactyly?
- Why children are born with fused fingers: the main causes
- treatment of the disease
- Prevention of ectrodactyly
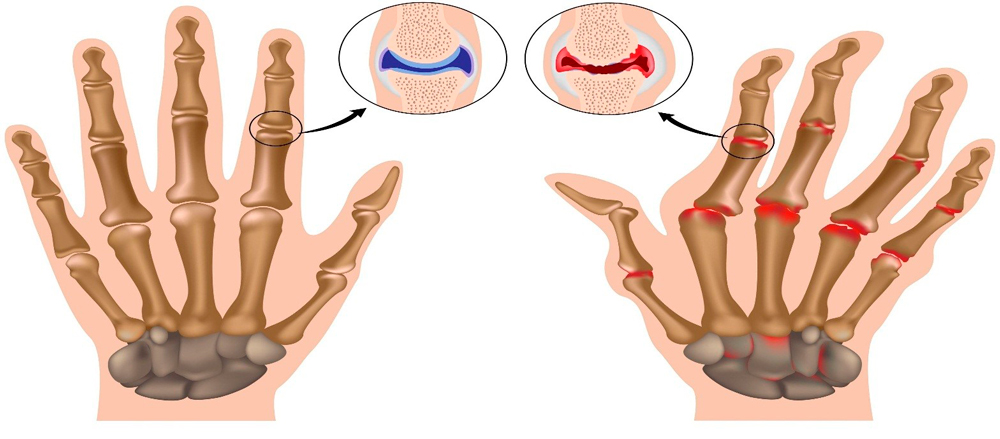
osteoarthritis in the hands
Statistics from industrialized countries show an increasing trend in the incidence of osteoarthritis. The pathological process develops in a certain group of joints, and arthrosis of the hands is one of the most common localizations. In this article you will learn why the disease develops, how it develops and what special features must be observed during treatment.
Arthrosis of the hands is a degenerative-dystrophic disease of the small joints, which is accompanied by progressive destruction of the cartilage tissue, intermittent aseptic (non-infectious) inflammatory processes, deformation of the hand with permanent impairment of its function and an increasing pain syndrome . This leads to reduced quality of life, loss of ability to work and ability to support yourself.
- Small, differently shaped carpal bones (8 in total) arranged in two rows (proximal and distal); the proximal row forms the carpal joint with the radius of the forearm;
- the tubular metacarpals - their proximal parts form the metacarpals I through V with the distal row of the carpals; their distal ends form the metacarpal joints I to V
- the small long bones of the fingers, 3 on the second to fifth fingers and 2 on the first finger; they form the metacarpophalangeal joints I to V, the proximal and distal interphalangeal joints.
Most women who are older than 50 years develop hand osteoarthritis. The frequency of the disease increases with age. If treatment is started early, the destruction of the joint surfaces can be stopped. ICD-10 code:
- M18 – Osteoarthritis of the first wrist (rhizarthrosis);
- M19 – Other osteoarthritis of the hand and fingers – M19 (Other osteoarthritis).
Causes of osteoarthritis in the hand
Various external and internal factors can cause osteoarthritis:
- Hereditary structure of the cartilage – it can quickly deteriorate under the influence of various factors;
- advanced age and old age - the destruction of articular cartilage is favored by age-related changes in blood circulation and reduced metabolism;
- Hormonal pathology – especially common in women with reduced hormonal balance, including age-related menopause;
- physical exertion – constant, long-lasting fine work with hands, which is accompanied by micro-injuries; Women are particularly vulnerable to heavy household chores;
- Consequences of hand injuries – fractures, dislocations, bruises;
- Consequences of acute and chronic arthritis (inflammatory processes) of different origins.
The body changes due to various external and internal causes: The amount of synovial fluid that nourishes the cartilage decreases. The cartilage covering the heads of the articular surfaces gradually thins, loses elasticity, cracks and deteriorates. This leads to the proliferation of bone and connective tissue, changes in shape and functional impairment of the small joints. This process is accompanied by a gradually increasing pain syndrome.
- people who work with heavy loads on their hands or play sports - plumbers, wood turners, pianists, tennis players, housewives;
- people suffering from osteoarthritis;
- have close relatives with osteoarthritis in their hands.
What is Dupuytren's disease?
Dupuytren's contracture (fibromatosis of the hand) is a non-inflammatory degeneration of the tendons of the hand that causes the fingers to lose mobility and be unable to bend fully. Statistically, men are affected more often, while the disease is 6-10 times less common in women and usually has a benign form.
The tendon degenerates into scarred connective tissue on the ring finger (40 % of cases), but the contracture can affect other fingers as well. Loss of mobility of the little finger occurs in 35 % of the patients, the middle finger is affected in 16 % and contractures of the thumb and index finger occur in only 3 % of the cases. The disease is characterized by inheritance of the fingers, beginning with the ring finger. Since Dupuytren's disease progresses very slowly, the index finger and thumb are less susceptible to pathological tendon changes.
The contracture usually develops after the age of 40 and affects both hands. However, if the disease is diagnosed at a younger age, there is a risk that it will progress rapidly.
Causes: trauma, heredity, etc.

The exact causes of the disease are not known to this day. Dupuytren himself, in his description of the contracture, suggested that it is caused by chronic or acute trauma to the hand. A fracture or a severe bruise, but also persistent pressure on the hand, for example from constant leaning, can trigger pathological tissue changes.
In modern orthopedics, the role of trauma in causing hand contractures is controversial. In most cases, both hands are affected, which means that the condition cannot be caused by external factors. In some cases, however, trauma to the hand, particularly chronic trauma, aggravates the disease and contributes to its rapid progression.
A connection between Dupuytren's contracture and disorders of the peripheral nervous system or the protein or salt metabolism could not be proven. A controversial theory is the neoplastic nature of the disease. Many orthopedic surgeons strongly disagree with this. However, there are studies that link connective tissue hypertrophy in the tendon to tumor cell activity. Oncogenes that play a key role in the development of fibrosarcoma have been found in the cells of patients with contractures.
It has been found that Dupuytren's disease often occurs in relatives; moreover, it occurs specifically in the male line. For this reason, doctors assume that it is a hereditary disease, the cause of which should be sought in the genes.
Signs and symptoms of clinodactyly

The affected finger may be oddly curved in the middle or overlap with other fingers, most commonly the pinky, although the ring finger can also be affected.
In general, clinodactyly, as an anomaly, does not in itself cause pain or inflammation, although it can cause discomfort when using the affected hand. If the finger curve is more than 30 degrees, hand function and fine motor skills may be affected.
If the clinodactyly is minor, you can skip treatment at this point and just watch your child use their hand. However, when clinodactyly is more severe, it is helpful to know that there are several treatment options.
Causes of crooked fingers in children
In some cases, clinodactyly can be inherited, but it can also be part of a broader pathology such as Down syndrome. According to the Philadelphia Clinic, one in four people with Down syndrome has clinodactyly.
Crooked fingers as part of a larger pathology are also common in Klinefelter syndrome, Turner syndrome, and many other diseases.
It's not just the hands: Researchers at the GI Gorky Research Institute for Children's Orthopedics and Orthopedics have found that the finger is also part of a thumb disorder. Turner syndrome indicates that children with fibrodysplasia often have a curvature of the big toe.
Causes of joint deformations in fingers and toes
The first and most important cause of the disease is a genetic predisposition. It is not the disease itself that is inherited, but metabolic characteristics, bone and cartilage structure and density. Diabetes, endocrine disorders, trauma and increased pressure on the toe joints, excess body weight, unbalanced diet, alcohol abuse and intoxication, hypothermia, viral infections, etc. can also be causes.
Treating toe deformities requires long-term treatment. The first step is to relieve the affected joints: hands should be relaxed as much as possible, lifting heavy objects and jerky movements with your hands are prohibited. Pain relievers and nonsteroidal anti-inflammatory drugs are used to reduce pain and inflammation. Chondroprotectors - drugs that 'act' directly on the reconstruction of bone and cartilage parts - are also used. In order to achieve the desired effect, the drugs of this group must be taken for a long period of time - at least three months.
Physiotherapeutic methods These treatments relieve stiffness, inflammation, and pain, and help maintain wrist function. These include heating (including ultraviolet, laser and infrared radiation), ultrasound, electrophoresis, magnetic therapy and phonophoresis.
If drug therapy is ineffective, surgical treatment – partial or total prosthesis of the affected joints – is recommended.
Treatment of toe deformities
The treatment of toe deformities also requires long-term treatment. Painkillers and non-steroidal anti-inflammatory drugs are prescribed to relieve pain. With severe inflammation and pain in the toe joints, corticosteroid injections are prescribed. Treatment also includes physical therapy and physiotherapy.
In addition to conservative treatment, it is important to take steps to prevent blisters and sores. The footwear should be changed to larger shoes. Special orthopedic shoes or special insoles are required. Shoes should be heelless and have a wide toe box.
When conservative treatment is ineffective, surgical treatment is recommended, which includes surgery of the soft tissues and bone structures.
The family clinic offers effective and gentle methods for treating toe joint deformities. Our specialists use modern technology and special designs for surgical interventions that achieve good results and restore mobility to your joints.
Make an appointment with an orthopedist and trauma surgeon
Make an appointment for a consultation with a qualified specialist in orthopedics at the Clinic for Family Medicine.
Changes in the nails in isolated malformations
anomalies nailsCrooked, drum-shaped, and spoon-shaped nails can be an autosomal dominant inherited abnormality that is not associated with other abnormalities. Although congenital ingrown toenails can result from a congenital dislocation of the thumb that can only be corrected by surgery, in most cases these abnormalities resolve independently and are not associated with an anatomical defect.
Spontaneous regressive ingrown toenail can result from transient hypoplasia of the toenails (particularly the thumbs) that usually resolves within 12-18 months. Nail lesions can be exacerbated by external trauma and recurrent/chronic paronychia.

Congenital ingrown nails:
a – A congenital deformity of the big toe led to recurring ingrown toenails that eventually required surgical correction. There were already similar problems in the family.
b - the child had ingrown toenails on the big toe of both feet, which improved without treatment by 12 months of age.
Nail changes in ectodermal dysplasia
Many of the ectodermal dysplasia are associated with nail abnormalities; in some these are characteristic and diagnostically significant. In congenital pachonychia, an autosomal dominant pathology with variable penetrance, hyperkeratosis of the nail bed develops in the first months of life.
The nail plate is then thickened and lengthened. The nail plate thickens and lengthens.The nail plate thickens and turns yellowish-brown. Minor trauma can cause painful detachment of the plate from the nail bed and bleeding. Typical are hyperhidrosis on the palms and soles, as well as blisters and vesicles. Other manifestations include leukokeratosis of the oral mucosa (not associated with malignant degeneration), thickening of the eardrums leading to deafness, corneal leukokeratosis, and cataracts. Hyperkeratotic papules on the volar surfaces of the limbs, dermoid cysts, and multiple steatocytomas have also been described.
Yadasson-Levandowski type congenital pachonychianot associated with ocular manifestations is caused by mutations in the keratin 16 (KRT16) gene or keratin 6A (KRT6A) gene located at loci 17q 12-21, 12q13. Defects in the keratin 17 (KRT17) and keratin 6B (KRT6B) genes are associated with Jackson-Lawler pachonychia, which is retinal dystrophy without mucosal leukoplakia.
Congenital dyskeratosis can be confused with congenital pachonychia. However, in congenital dyskeratosis, which can be X-linked, autosomal dominant, or autosomal recessive, the nail plate is thin and longitudinal sulci and pterygium are present. In congenital dyskeratosis of the neck and trunk, poikiloderma with reticular pigmentation, telangiectasia, and atrophy are the main features.
Leukoplakia of the oral mucosa may be associated with the development of squamous cell carcinoma and other gastrointestinal malignancies. Pancytopenia, resembling Fanconi anemia, occurs in 50% of % patients in their second and third decades of life. In most cases, the mode of inheritance is recessive, X-linked and associated with mutations at the Xq28 locus in the gene encoding dyskerin (DKC1). Nail hypoplasia can also be a feature of hydrotic ectodermal dysplasia and Coffin-Siris syndrome.
classification
II. DIAGNOSTIC AND THERAPEUTIC METHODS, APPROACHES AND PROCEDURES
Minimum list of tests to be performed at the time of referral for a planned hospital stay:
- coagulation picture (bleeding and clotting time, prothrombin, fibrinogen, platelet adhesion and aggregation reaction, antithrombin);
- blood chemistry (total protein, alanine aminotransferase, total cholesterol, bilirubin, direct bilirubin, creatinine, urea, glucose, potassium, sodium, phosphorus, calcium, chlorine);
- coagulation values (bleeding and clotting time, prothrombin, fibrinogen, platelet adhesion and aggregation, antithrombin);
- blood chemistry (total protein, alanine aminotransferase, total cholesterol, bilirubin, direct bilirubin, creatinine, urea, glucose, potassium, sodium, phosphorus, calcium, chlorine);
Emergency diagnosis: not performed.
Complaints.Deformation of the limbs causing functional and cosmetic impairment and burdening the patient's psyche.
Medical historyHistory: Toe and/or foot injuries, with increasing deformity of the limb segment with age.
– Hammer-shaped deformation of the middle fingers, accompanied by pronounced tension under the skin of the extensor tendons and the formation of painful ossicles along the backs of the deformed fingers;
– Abnormal anatomical bone structure.
differential diagnosis
The diagnosis of acquired finger and toe deformities is not difficult due to the visually detectable deformities and impaired limb function.
• First-generation cephalosporins.Cefazolin, 50-100 mg/kg, intravenously, once 30-60 minutes before surgery.
Intravenous drip doses of 10-20 mg/kg/day, in one or more injections, for severe infections and in children 1 month and older;
Vancomycin: 15 mg/kg/day, to a maximum of 2 g/day, every 8 hours, intravenously; each dose should be administered over at least 60 minutes.
• Paracetamol, 200 mgParacetamol, 200 mg, tablets – 60 mg per kg of the child's body weight, 3-4 times a day. The interval between doses should be at least 4 hours. The maximum daily dose is 1.5 g - 2.0 g;
Paracetamol rectal suppositories 125, 250 mg – a single dose of 10-15 mg/kg of the child's body weight, 2-3 times a day, after 4-6 hours;
Paracetamol suspension 120 mg/5 ml, for oral administration - a single dose of the drug is 10-15 mg/kg body weight, 4 times a day, the interval between consecutive doses is at least 4 hours (the dose for children aged 1 up to 3 months is determined individually).
Paracetamol Oral Syrup 2,4% 50ml – Children from 3 to 12 months – ½-1 teaspoon (60-120 mg); from 1 to 6 years – 1-2 teaspoons (120-240 mg); from 6 to 14 years – 2-3 teaspoons (240-360 mg), 2 to 3 times a day.
The maximum duration of treatment with paracetamol as a pain reliever is no more than 3 days.
• Ibuprofen Suspension 100 mg/5ml - 200 ml, for oral administration, 7-10 mg/kg body weight, maximum daily dose - 30 mg/kg. The interval between doses of the drug should not be less than 6 hours. Duration of treatment no longer than 5 days, as an analgesic.
In children aged 1 to 14 years: 1 mg/kg to 2 mg/kg body weight intravenously, intramuscularly or subcutaneously. Intravenous injections should be given very slowly or diluted in an infusion solution and given as an infusion. The dose may be repeated at 4-6 hour intervals.
causes
Abnormal hand development in children is often caused by a hereditary factor. There may be a gene in the family with a 'fault' that is passed from generation to generation. Sometimes the faulty gene 'sleeps', ie it does not show up for several generations and then becomes active. If a family member has an abnormality, a geneticist should be consulted when planning a pregnancy.
Hand deformities in children can also be caused by abnormalities in the formation of the limbs in the womb. These malformations can be caused by external factors affecting the mother's body during the 3rd to 7th week of pregnancy:
- consumption of alcohol, drugs or smoking during pregnancy;
- Ionizing radiation;
- taking certain medications;
- infectious diseases;
- an unfavorable environment etc.
Often the cause of the anomaly in the child remains unknown. However, special treatment is required.
Types of anomalies of the fingers in children
The following hand development abnormalities are most common in children
- syndactyly. This malformation is considered one of the most common. In this anomaly, the fingers are fused together. There are several forms of this deformity. The fingers are partially or fully fused, and the anomaly may involve only the skin or the bones may be fused.
- polydactyly. It is characterized by the presence of an additional sixth finger. It can be present on one or both hands, more rarely on the feet. In most cases, the sixth finger is underdeveloped and therefore looks more like an extra fang. In rare cases, the finger has bones, ligaments, and tendons and is fully functional.
- Brachydactyly, ectrodactyly. These defects are characterized by the absence of phalanges, underdevelopment and shortening of the fingers. Brachydactyly has nail plates. Often this anomaly is accompanied by a fusion of the fingers.
- camptodactyly. This is the term for a malformation in which a flexion deformity can be observed. The fingers cannot fully stretch either in the passive state or during active activities. Due to the lack of a hand crease, the skin is greatly stretched. The anomaly most commonly affects the little finger.
- hypoplasia. This is a specific malformation of the thumb. Depending on the development, it can manifest itself in different ways. The thumb is often shortened or emaciated. Sometimes it is attached to the body through the skin or it may be absent altogether.
- Concretion. This anomaly is also known as a fusion defect. The main feature of this pathology is that two fingers sit on one metacarpal bone, so the functioning of the hand is disturbed. The space between the fingers is very narrow. The hand may be shorter than normal.
- split hand. Also called 'crab claw' because the hand is split in two. Can occur on one or both hands. Often occurs on the legs as well.
- brachymetacarpy. In this deformity, the metacarpal is very short. Because of the 'collapsed' metacarpal, the fingers are also short. This is particularly noticeable when the child clenches their fists.
- gigantism. Enlarged fingers or single phalanges. More rarely, there is an enlargement of all parts of the hand.
- Congenital amputation of fingers or phalanges. Very rare. The limb ends in a stump, which can worsen as the child grows. Deformation of the residual limb is often observed. This phenomenon is caused by uneven growth of bones and soft tissues.
- macrodactyly and megalodactyly. It is characteristic that one or more fingers are longer and thicker. In most cases, the finger remains functional but has a pronounced cosmetic defect.
What is clinodactyly? Causes, diagnosis and treatment of clinodactyly in children

Clinodactyly is an abnormally curved or bent finger, usually caused by abnormal development of the finger's little bones. It can also be caused by the hand's growth plate being abnormally shaped or the bones growing in an unusual direction. Diagnosis involves visual examination, and treatment in severe cases may require surgery.
According to Boston Children's Hospital, the condition affects approximately 10 %s in the general population, with varying degrees of severity.
diagnosis
A physical examination of the affected hand helps determine the degree of curvature of the finger and how it affects function. The doctor may recommend imaging tests, such as x-rays, to better see the bones of the finger and hand. Range of motion tests can also be done to understand how the curvature affects function and how best to help your child.
Sometimes clinodactyly does not require immediate treatment, particularly when the finger is only slightly curved or there are no functional difficulties. Doctors may recommend constant monitoring of the hand and finger to make sure the situation isn't getting worse.
If the curvature of the finger is more than 30 degrees, treatment may be strongly recommended. Treatment is usually most effective when the child is very young because the bones are not fully developed.
If surgery is deemed necessary, part of the curved part of the bone is removed to straighten the finger. The tendons and soft tissues can be loosened or operated on to relieve the finger and joint and ensure future stability. The finger is then attached with pins or screws to keep the bones straight.
Once everything is stabilized, the finger is immobilized with a cast or splint. Depending on the severity of the curvature and the extent of the surgery, recovery will proceed accordingly.
Once any bandages or casts are removed, the doctor may suggest working with a physical therapist who specializes in hand mobility. He or she will help your child regain full range of motion or learn to adjust to a new range of motion or function.
What is syndactyly?
Syndactyly is a congenital malformation of the musculoskeletal tissue. The main feature of this pathology is that the fingers or toes are fused together.
The disease can affect one or more limbs. In addition, syndactyly of the hand or leg may be accompanied by other limb malformations related to abnormal development of the joints, related apparatus, etc.
In syndactyly of the legs, as in the arms, there are two forms depending on the type of fusion:
- soft tissue shape. Only soft tissue fusion occurs, but the bones can still develop fully.
- bony shape. In the bony form, the fusion of the fingers is made more difficult because the finger bones are partially or completely fused together.
Depending on the degree of fusion, it is a simple or complex fusion. In the first case, healthy fingers fuse together, while in the second case the disease is accompanied by other abnormalities and malformations.
Why children are born with fused fingers: the main causes
Parents whose son or daughter is born with anomalies wonder why their children are born with crossed fingers. Doctors have now discovered that the causes of crossed fingers are often hereditary. If a parent had this abnormality, there is a 50 percent chance that the child will be born with a developmental disability. The mutated gene is particularly common in the male line.
Sometimes, when syndactyly is diagnosed, the causes are not hereditary. The abnormality occurs between weeks 4 and 8 of pregnancy, when the embryo is developing and forming a hand.
The following factors can cause abnormal limb development:
- taking certain medications during pregnancy;
- toxic exposure (inhalation or ingestion of toxic substances);
- exposure to radiation;
- unfavorable environment or unhealthy working conditions;
- consumption of alcohol or intoxicating substances;
- infectious, inflammatory processes in the mother's body.
Sometimes syndactyly of the fingers or toes is caused by trauma to the uterus or low fertility during pregnancy. The abnormality is caused by the pressure of the walls of the uterus on the fetus.
treatment of the disease
Treatment for ectrodactyly involves surgery. Surgery is often performed during puberty for a condition such as ectrodactyly. Cosmetic defects are corrected and the function of the foot or hand is restored.
Before the operation, the necessary examinations are carried out: ultrasound, X-ray, CT, MRI, Doppler ultrasound and electromyography of the hands and feet.
There are several surgical methods for ectrodactyly:
- splitting fingers with donor skin;
- Transplantation of fingers from foot to hand;
- Correction of joint flexion and extension.
After correcting the hand or foot dysfunction, a surgical intervention is recommended to correct the cosmetic defect: arthroplasty.
Prevention of ectrodactyly
Specific preventive measures have not been developed, since the causes of ectrodactyly are not known - the causes of the pathology are not scientifically proven. A list of general recommendations is as follows:
- Giving up bad habits (smoking, drinking alcohol);
- Eat a sensible diet;
- Distribute work and rest times evenly;
- Avoid physical and psycho-emotional stress;
- Avoid cold weather;
- Get regular medical check-ups;
- Predictive planning of pregnancy.
The main method of preventing the development of pathology in the fetus is to follow all the recommendations of the obstetrician-gynecologist, conduct regular visits to the doctor and check-ups.
Read more:- name of the fingers.
- ectrodactyly.
- Why are the big toes crooked?.
- Gum disease on feet.
- straightening of the fingers.
- structure of the toes.
- structure of the toes.
- Tendonitis on the 1st toe.
