Signs of impending death Fear of impending death often stems from a lack of knowledge, so we encourage you to read this text. You may get answers to some of your questions and hope that you will seek more information and help. It's easier for loved ones to support each other during this difficult, responsible time when they know what to expect.
- How life can go on after prostate removal
- Sexual activity after prostate removal is possible
- Anatomy of the veins in the lower limbs of man
- What happens if the diseased vein is not removed?
- blood conversion
- muscle metamorphosis
- Rare, unexpected symptoms
- To better understand the loved one and their needs during this time, ask yourself questions:
- POSSIBLE COMPLICATIONS OF AMPUTATION
- Heart Surgery in Israel – Prof. Bitran
- How to get free care at home
- Free accommodation in a retirement home
- What documents must be submitted?
- Painkillers.
- Wound care after surgery
- Medical aftercare after surgery
- How do other organs work after a gallbladder removal?
- How to dispose of the different types of medical waste?
- Collection of medical waste
- Requirements for containers and bags for medical waste
- Other important points
How life can go on after prostate removal
Surgery on this organ will surely change a man's life. The most important changes are certainly for the better. The pain disappears, urination becomes possible again, and in the case of stage I-II prostate cancer, complete recovery is possible. But there will also be unpleasant consequences that you will have to wait and, in some cases, adapt to.
The removal of the prostate takes place under anesthesia. After removal, the following symptoms may appear:
- dizziness, general weakness, nausea;
- pain in the area of the surgical wound;
- initially, a small amount of blood is excreted in the urine.
These symptoms disappear completely after a few days. Doctors help to get through this period quickly by prescribing painkillers, diuretics and antibiotics to avoid infection.
Physiological consequences of prostatectomy in men
Free urination is not restored immediately. The tissue of the urethra is swollen after the operation.
- To remove the obstacle to the flow of urine, a catheter is inserted into the urethra, which must remain for some time.
- In 80% of cases, urinary incontinence occurs because the pelvic muscles weaken and a urine bag must be used.
In men under the age of 60, both the catheter and the urinary catheter are usually removed after 2-3 days. In complicated cases, if you are elderly or have had major surgery, they may stay in place for several weeks. Over time, muscles will regenerate and urination will return to normal.

Dangerous complications - bleeding, water intoxication - are very rare. Doctors treat you effectively, but discharge from hospital may be delayed.
Sexual activity after prostate removal is possible
Most men regain their potency after surgery. Exceptions are limited potency after a total prostatectomy and advanced age.
After a prostatectomy, abstinence for three months is recommended. In most cases, the nerves and blood flow completely return to normal during this period. Sometimes more time is required and doctors allow taking Viagra or Cialis.
Occasionally it happens that the semen does not leak out but is pushed into the bladder. This condition is harmless to health and can be quickly remedied with vibromassage.

Anatomy of the veins in the lower limbs of man
The venous system of our body comprises more than 75 % of all the blood circulating in the human body. There are 2 types of veins in our legs: The saphenous veins (in the upper layers of the skin) and the deep veins (near the arteries).
Arterial blood, saturated with oxygen and nutrients, begins its journey from the heart. From the respiratory organs it transports the nutrients to all organs and tissues. After delivering the nutrients, the blood absorbs the metabolic products and goes into the venous circulation.
The venous circulation in the legs runs in a downward direction. Blood flow is increased through the muscles. Venous blood flows through vessels (deep veins) to the heart and respiratory organs, where it is replenished with nutrients. The blood that flows through the subcutaneous veins does not carry nutrients or oxygen.
The deep veins in the legs carry 90% % of venous blood. 10 % of venous blood is passed through the great saphenous vein to keep the tissue viable. The superficial venous system of the feet arises from the venous network of the toes and forms a network of veins along the back of the foot. From these veins, the medial and lateral marginal veins branch off into the small and large saphenous veins.

Varicose veins occur mainly in the great saphenous vein and less commonly in the great saphenous vein. The great saphenous vein is the longest vein in our body. It can have five to 10 pairs of valves and is 3-5 mm in diameter.
What happens if the diseased vein is not removed?
A vein that has been affected by varicose veins for a long time may not recover on its own. How the varicose veins develop The vein expands several times, darkens and causes severe pain. The vessel wall becomes slack and thin. The blood collects on the walls of the dilated vessel and blood clots form. A blood clot blocks blood flow, preventing tissues, organs and the brain from getting the nutrients and oxygen they should.
The greatest threat to the human body is a blood clot that breaks off and travels through the circulatory system. A blood clot can block any vessel, vein, or valve on the way to the heart, brain, and other vital organs. It contributes to myocardial infarction, stroke and thrombophlebitis.

Thrombi detach only in large vessels in which the blood flow has a high flow rate. In small vessels, drainage is poor, the clot cannot dislodge, and blood backs up in its path.
blood conversion
The heart stops beating. As a result, blood circulation also stops. After death, the blood moves down through the blood vessels under the influence of gravity. Depending on the position of the corpse, the lower part of the body usually turns blue-purple. These are the spots of the corpse.
After a while the blood thickens. This happens gradually. The blood plasma appears to seep through the walls of the blood vessels into the surrounding tissues. And the red blood cells are completely destroyed. This process is called hemolysis.
muscle metamorphosis
An interesting fact is that muscles do not die immediately after the body dies. Our muscles function through a chain of biochemical processes of energy storage and use - adenosine triphosphate (ATP). During life, ATP is broken down - the muscle contracts, recovers, relaxes.
After death, all that remains is the process of ATP degradation. This leads to a gradual thickening and contraction of the muscle. This in turn causes the joints to lock in the position in which the corpse is laid out. Rigor mortis is the life of the muscle after death. Forever? No of course not. If the muscle dies over time, rigor mortis will pass.
Rare, unexpected symptoms
Worsening can be sudden, but it is still possible to talk to your loved one and their doctor in advance about what to do if they develop pneumonia, a seizure, pulmonary edema or brain swelling.

The grief associated with waiting is natural A translation of a Norwegian article about how grieving the imminent departure of a loved one who is alive but seriously ill is a normal condition. And a reason to be open and honest with yourself and others
- Ambulance and subsequent hospitalization/resuscitation (it's best to avoid unnecessary travel while dying);
- calling a doctor and/or nurse;
- cessation of activities and simply remaining with them;
- inviting relatives and loved ones to say goodbye;
- If you live in Moscow, you can contact the Coordinating Center for Palliative Care and get advice: 8 (499) 940-19-48.
As death approaches, fingernails may change color, hands and feet may become cooler, and facial features may become sharper. A pale, white nasolabial triangle may also appear on the face.
Sometimes the person does not die, as if waiting for permission from loved ones. It is important to let her go and allow her a peaceful death.
Say the most important thing: Forgive me. I forgive you. I love you. I thank you. take farewell.
To better understand the loved one and their needs during this time, ask yourself questions:
- What would be most important to you at the end of life? (e.g. good medical care, the opportunity to say goodbye to loved ones, to get your affairs in order).
- Are there any disagreements in your family that might worry your loved ones? It might be worth taking care of the will in advance.
- Is there someone (human, animal) that your loved one would like to see again before they die? What matters would she or he like to do? What thoughts bother him and keep him awake?
- Understand your loved one's last wishes (who they want to invite to the funeral, whether they want cremation or burial, whether they want religious rituals).
Don't forget to take care of yourself during this difficult time. If you need psychological help, you can contact the terminally ill helpline at 8 (800) 700-84-36 (toll-free, 24 hours a day).
POSSIBLE COMPLICATIONS OF AMPUTATION
One of the problems that can occur after amputation is residual limb swelling. It can arise from common causes such as circulatory and/or metabolic disorders, including heart failure, protein and/or electrolyte imbalances and renal dysfunction, as well as local lesions. Regarding the latter, it should be noted that it is often caused by an increase in local blood flow against the background of the healing process of the postoperative wound after amputation. Such swelling is limited and has certain limits. If these are exceeded, one or even several other causes must be sought.
Local swelling can occur, for example, in the area of foreign bodies: sutures or bandages, non-viable tissue of the limb, the shaft of a prosthesis, etc., which the body tries to enclose with connective tissue in order to isolate and reject it. The position of the residual limb is important - if no external pressure is applied, its low position contributes to the formation of edema, which is most pronounced in the distal area.
Local edema can also be caused by superficial or deep wound infections, skin diseases, and the presence of an obstruction to normal lymph and/or blood flow. It should be noted that venous outflow is passive and indirectly facilitated by muscle contraction. In the amputated residual limb, muscle contraction is not as active as in the intact residual limb, even with myoplastic coverage. In addition, varicose veins, postthrombotic thrombosis, fibrosis after radiation and postoperative scars in the groin and popliteal fossa can have a negative effect in this regard. External pressure (tight bandage, bandage or prosthetic cuff) has a similar effect. Here, even a lightly palpable ligature can lead to residual swelling of the extremity weeks or months later. It is important to distribute the pressure on the residual limb so that it decreases from the distal to the proximal residual limb. This not only prevents the development of chronic edema, but also improves the conditions for the free outflow of lymph and venous blood.
Heart Surgery in Israel – Prof. Bitran

Prof. Dr. Daniel Bitran is a leading cardiac surgeon in Israel. For the past 12 years, his name has been at the top of the list of the top 5 cardiac surgeons in Israel. He has performed more than 10,000 complex heart and vascular surgeries. The mortality and complication rates in the Department of Cardiac Surgery headed by Prof. Bitar are higher than those of the leading cardiac surgery centers in Western Europe.
How to get free care at home
People with Group 1 and 2 disabilities who are unable to take care of themselves and need help at home can receive assistance from the state free of charge. To obtain a disability card you must:

– visit the polyclinic to which the MHI policy is assigned;
– get a referral from your GP for an ITU (medical and social assessment);
– pass the MMSE test (assessment of the mental and physical health and living conditions of the patient);
– obtaining a disability card under the MMSE;
– Apply for a certificate from the local social security office.
The MSE office provides the disabled person with an individual program and technical means of rehabilitation: bedside toilet, wheelchair, etc. The program includes a disability pension, free travel on public transport, sanatorium treatment and other benefits.
You can also get support from a nurse or social worker as part of this program. This person comes to the home several times a week to provide medical treatment, buy groceries and medicine, and help around the house.
Free accommodation in a retirement home
The fact that a bedridden person lives at home - even with the help of a social worker - means that family members must be significantly involved in their care. A caregiver cannot visit you every day or stay by your bedside overnight. This is not covered by any government program. The family must either quit their jobs to care for the bedridden person themselves, or hire a paid caregiver to do so.
If both options are not suitable for the family, there is only one option left: placing the disabled person in a nursing home. Public geriatric facilities accept men from the age of 60, women from the age of 55 and people with disabilities of any age group 1-2 (over 18 years). The main condition for placement is that the person is unable to support themselves and that they have no relatives who can provide adequate care. The family member may be completely absent, live far from the disabled person, or be a migrant worker. In all of these cases, it is physically impossible for a non-disabled person to be with a bedridden person requiring care 24 hours a day.
Barriers to placing a disabled person in a state nursing home include:
– Infectious diseases: HIV, COVID-19, tuberculosis, scabies, venereal diseases, etc;
– Malignant addictions: alcoholism, drug addiction, smoking;
- Mental illness with acute psychotic episodes where the person poses a danger to self and/or others;
– If the disabled person has a healthy relative who can take care of them.
In order to place a bedridden person in a nursing home, you must contact the local welfare office, write an application explaining the circumstances and provide a number of documents.
What documents must be submitted?
In addition to the passport, the applicant and his/her legal representative (relative/guardian) must present the following documents to the social welfare office:
Painkillers.
An important part of rehabilitation after an amputation is the elimination of pain. Physical pain caused by the operation is often associated with the healing of the stitches. However, it is not uncommon for other types of pain to also occur – phantom limb pain. There may be burning and itching sensations in the residual limb area, which is uncomfortable for the patient. Phantom pain cannot be treated with conventional medicines, but requires special treatment such as massage, physical therapy, etc. The first step is to work psychologically with the patient.
Problems with phantom limb pain should be immediately reported to the attending physician, as well as people close to the patient; their support will help to overcome the difficulties. After fitting a lower leg, hip or hand prosthesis, the hygiene of the residual limb should be carefully monitored, otherwise phantom pains will also occur.
Wound care after surgery
In general, the residual limb requires the usual hygiene measures: daily alternating showers, use of hypoallergenic creams and avoidance of wound drainage. A massage that restores blood circulation and reduces the risk of psychomatic phantom pains is very helpful. Particular attention is paid to the healing process: the thinner the scar, the better for inserting the prosthesis.
Patients suffering from various cardiovascular diseases as well as diabetes require much more careful wound care. The pharmaceutical industry today offers a number of preparations that accelerate the process of tissue regeneration; an application is also possible.
Medical aftercare after surgery
After gallbladder surgery, the surgeon often does not make long-term recommendations. However, to avoid reoperation, complications, and the recurrence of gallstone symptoms, you should:
- 1-2 times a year a visit to the gastroenterologist to assess the condition of the hepatobiliary region
- 1-2 times a year an ultrasound examination of the abdominal cavity, especially the main bile duct.
- Regular or course of treatment with bile thinners (ursodeoxycholic acid - UDCA) and antispasmodics as recommended by your gastroenterologist.
After gallbladder removal, you should see your gastroenterologist regularly and agree on a list of approved digestive medications such as Allochol, Mesim, Creon, Festal, etc. Also discuss the possibility of taking antibiotics and vitamins for the future. It is not advisable to take medication on your own - talk to your doctor.
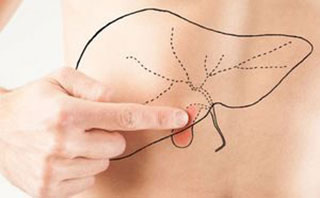
How do other organs work after a gallbladder removal?
Observation by a gastroenterologist is also required for another reason. With the new anatomical conditions in which the gallbladder is absent, the function of other organs of the digestive tract is often altered. The liver itself, the pancreas, the intestines, the stomach and the bile ducts function differently after the gallbladder has been removed.
After gallbladder removal:
- There is a relative deficiency in the enterohormonal system of certain hormones that regulate the tension of the muscular ring (sphincter of Oddi) surrounding the common bile duct and the pancreatic duct (virsunga). In this situation, persistent sphincter spasm may develop. Persistent spasm of the sphincter leading to pain in the right and left lower abdomen and umbilical pain mimicking pancreatitis.
- The bile can no longer accumulate in the 'bag' of the gallbladder, so that it flows out unconcentrated. This prevents the normal activation of pancreatic enzymes in the duodenum, disrupting the important intestinal phase of digestion. The consequences are diarrhea or constipation and a disturbance of the intestinal microflora occur.
- When the sphincter of Oddi is in a relaxed state, the microflora of the duodenum can invade the unprotected bile ducts. This leads to the formation of Inflammatory processes in the walls of the ducts - Inflammation of the bile ducts.
- The prevailing opinion in the medical community is that removal of the gallbladder is a an additional risk for developing hepatic obesity due to disturbed production of gastric hormones and improper nutrition, which could not be clearly confirmed in previous studies.
Some patients are concerned that the liver may need additional support after gallbladder removal. The answer depends on whether there is existing liver disease, damage to liver tissue (fibrosis or cirrhosis), changes in blood chemistry, etc. The gastroenterologist/hepatologist will give you an accurate answer based on an examination, analysis of your symptoms and your medical history. If necessary, the doctor will prescribe special liver treatment and hepatoprotectors. Prescribing medication for yourself is dangerous.
How to dispose of the different types of medical waste?
Since contact with medical waste entails toxicological, radiological and epidemiological risks, their handling is strictly regulated. However, it is not regulated by ordinances, but by SanPiN (Sanitary Rules and Regulations). All processes are carried out according to these regulations: the initial collection, the organization of interim storage, the subsequent transport and disposal.
For some types of waste, there are intermediate steps such as disinfection or decontamination. The following details the preparation for transportation, transportation, disinfection and disposal of medical waste.
Collection of medical waste
Medical waste is collected and disposed of by trained personnel who have been briefed and licensed for the job. Staff must be vaccinated against hepatitis B. The activity is carried out by the organization that generates the waste. The organization's medical waste disposal program applies.

The collection and further preparation for destruction includes:
- Loading of the medical waste on site into containers suitable for the respective type.
- Distribution of filled bins into reusable containers used for transfer to storage areas.
- Storage at the place of storage: for a maximum of 24 hours in separate rooms or in refrigerators (freezers) if the storage period exceeds 24 hours. Medical waste can be stored in a refrigerator for a maximum of one week prior to decontamination. When using a freezer, the maximum storage time is one month.
Requirements for containers and bags for medical waste
Class A medical waste does not have strict regulations for collection and disposal. More hazardous waste from the other categories is packed in reusable containers (which are regularly disinfected) or in hermetically sealed plastic bags or sealed containers. Items with sharp objects may only be placed in strong packaging that cannot be cut or otherwise damaged.
Other important points

- The collection, subsequent storage and disposal of 'B' and 'B' class medical waste should only take place in separate buildings or areas. This area should be divided into a 'dirty' zone and a 'clean' zone to which services are connected and ventilated without mixing potentially contaminated and uncontaminated airflows. The surfaces must be resistant to washing with concentrated disinfectant solutions. The optimal temperature is from +18 degrees Celsius to +25 degrees Celsius, and the humidity should not exceed 75 %.
- Handling medical waste requires mandatory documentation with process logs and contracts with companies that collect and dispose of the waste.
- If a Class B or C waste container is damaged, its contents must be collected by an employee wearing personal protective equipment using disposable cleaning tools or by hand with new gloves. The waste is then placed in new red or yellow bins/sacks that are sealed and labeled. Used PPE and cleaning equipment are also packed separately in containers marked by hazard class. Everything is then transported to an interim storage or disposal area.
- If a bag partially bursts without the contents falling out, it should be placed in a larger container.
In Russia, the problem of destroying medical waste is acute. On the one hand, they pose a real threat to the population, since they can contain toxic substances and are a source of contracting dangerous diseases. And not all organizations in the Russian Federation strictly follow the regulations for handling their residues, which poses a danger to the population, the environment and the atmosphere.
On the other hand, the disposal regulations can also be violated. Any company can transport, decontaminate and dispose of the waste produced by an organization, even without a license. The legal regulations apply only to substances of federal classification. And only 'G' and some other classes of waste fall into this category, but usually only after neutralization or destruction. Unauthorized activities often lead to errors in the handling of medical waste, which pose a high risk of dangerous situations.
Read more:- Where do the body parts go after the operation?.
- A tricky stump.
- What to do with amputated limbs?.
- The leg of a healthy person.
- Are human legs the same?.
- Ligament strain of the lower limbs.
- Leg Discomfort – Which Doctor Should I See?.
- Technique of tibia amputation.
