Patients with syphilitic periostitis complain of severe pain that increases at night. Palpation reveals a round or spindle-shaped, limited swelling with a dense, elastic consistency. The overlying skin is unchanged and palpation is painful. Spontaneous resorption of the infiltrate, bone growth or suppression and spread to the surrounding soft tissues can lead to fistula formation.

- The knee joint: how it works and why it hurts
- Cartilage, joint capsule, synovial fluid….
- Bones and their connections
- Characteristics of osteoblasts and osteoclasts in developing bone.
- Modes of bone development (ossification).
- Posterior osteosynthesis with plates
- Periosteal osteosynthesis with external fixation devices
- diagnosis
- Diagnosis of hip fractures
- Treatment
- Submerged osteosynthesis: use of pins
- Immersion osteosynthesis: plates
- Fibrous periostitis
- Serous albuminous periostitis
- causes
- Symptoms of subluxation and tilting of the kneecap
- Clinical Significance
- Treatment
The knee joint: how it works and why it hurts
Knee pain is the most common reason for visiting a rheumatologist. This joint is the most commonly affected joint because it is subjected to enormous stress on a daily basis. It is one of the most complex joints in the human body. How is the knee joint structured and what causes pain?
The knee joint is composed of two bones – the femur and the tibia. There are two ligaments between the bones ribbonsThese are arranged transversely to each other. They are called anterior and posterior. There are two on the outer and inner sides collateral ligaments (technically medial inner ligament i outer lateral). Ligaments are strong elastic fibers whose job is to direct the movement of the joint and inhibit it in certain positions. They have nothing to do with the tendons.
Ligaments are elastic fibers between bones, while tendons connect bones to muscles. So they are two completely different substances. Muscles gradually develop into tendons that attach to bones. When a person bends or straightens their leg, they control the muscles that pull the bones through the tendons.
Ligaments and tendons are different substances: they should not be confused!
Cartilage, joint capsule, synovial fluid….
Where the bones come together are their heads cartilagewhich protects you from friction and shock. Inside the joint are two menisciwhich are shaped like crescents. They are needed to protect the cartilage and bone from mechanical stress.
The cartilage and meniscus are located in what is known as the 'joint capsule'. joint capsuleInside the joint capsule is the synovial fluid (synovia). synovial fluid. Like oil, it lubricates all joint surfaces and prevents friction. This is the case when the amount of synovial fluid is sufficient and its viscosity is correct.
On the front of the joint are the kneecapor kneecap. It is held together by ligaments and tendons and is covered with cartilage on the inside. The kneecap is a kind of protective shield that protects the internal components of the knee joint from damage.
How is the knee joint structured? Clear demonstration with detailed explanations:
Bones and their connections
We are just beginning a new chapter in anatomy that deals with the musculoskeletal system. It supports the body, keeps the body parts in position, protects the internal organs and ensures the musculoskeletal system - movement.
The bones are the basis of the musculoskeletal system, which we are now dealing with. Osteology (from Greek osteon - bone) is the branch of anatomy that deals with the study of bone tissue, individual bones and the skeleton as a whole.
In addition to what you learned about bone structure in the connective tissue section, there are a few other important points that I will discuss in this article.
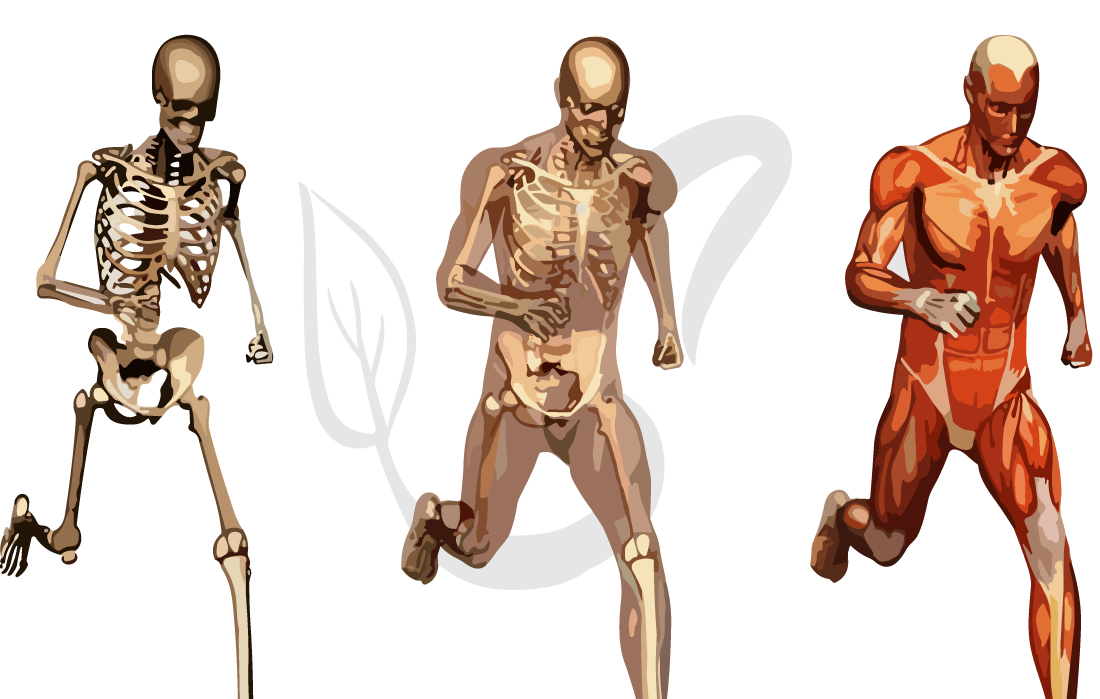
The skeleton and joints are the passive part of the musculoskeletal system, the muscles are the active part. The muscles contract to change the position of the bones - different movements occur.
Structure of the bone
The bones consist of organic and inorganic matter. The organic substance is represented by ossein (from Latin. os – bone), the inorganic substance is calcium phosphate. The elasticity of the bone is due to the ossein and the hardness to the calcium salt. Under normal conditions this ratio is balanced.
In children, the bones are more elastic and resilient than in adults: organic matter predominates. In the bones of older people, both the organic content and the inorganic calcium salt decrease, making the bones of older people brittle and prone to fracture.
The compact bone substance is formed by bone lamellae that lie closely together and form osteons (structural units of compact bone tissue). The compact substance gives the bone its strength.
The spongy substance also contains bone lamellae, but these do not form osteons, so the spongy substance is less solid than the compact substance. The molar mass contains red bone marrow between the bone ligaments (bone balls).
Characteristics of osteoblasts and osteoclasts in developing bone.

Two cell populations are required for bone development in bone (Figure 4):
Osteoblasts are cube-shaped cells (20-30 µm in diameter) with a single large cell nucleus that sit close together on the bone matrix (intercellular substance). The fibroblasts produce all components of the bone matrix. They have two different embryonic origins:
- Neural squamous cells (which are released from the edges of the embryo's neural groove as it closes into a neural tube). The fibrous bone tissue of the skull bone arises from them.
- Trabecular bone mesenchymal cells. From them the lamellar bone tissue arises.
Osteoclasts are multinucleated (2 to 100 nuclei per cell), large (20 to 100 µm), hematopoietic cells. They penetrate the connective tissue and cartilaginous layers of the bone via blood vessels. The function of osteoclasts is bone resorption.
The interaction of two cell types, osteoblasts and osteoclasts, is required for the formation of the bone organ.
Modes of bone development (ossification).

There are four types of ossification (Figure 5), depending on where bone formation (including ossicles) begins in the bone:
In intramedullary ossification (Figure 5), the primary ossification point is in the center of the connective tissue filling of the bone. The newly formed bone tissue then spreads from the center of the organ to its periphery. In this way the primary bone ossifies. Thickening usually occurs at the site of the primary ossification point (e.g. parietal tuberosity, external occipital protuberance, etc.).
Periosteal ossification is characteristic of secondary bones. Osteoblasts attach to the surface of the cartilage skeleton and begin synthesizing the bone matrix. This leads to compression and trophic disruption of the underlying cartilage tissue, the changes in which activate osteoclasts. As a result, bone tissue is formed on the surface of the cartilaginous skeleton, which gradually grows (Fig. 5). Periosteal ossification leads to the formation of a compact bone substance. In long bones, the diaphysis is formed in this way during the intramembranous period.
In endochondral ossification, the ossification point (primary focus) appears in the center of the cartilaginous bone formation. The bone tissue then grows from the center to the periphery (Figure 6). This leads to the formation of cancellous bone substance. In this way, the secondary bones are formed: the epiphyses and apophyses of the long bones, the cheekbones and the long bones (with the exception of the cranial arch).
Periosteal ossification is caused by the periosteumPeriosteumLatin. – periosteum). In children, the periosteum is responsible for bone thickness (remember, metaphyseal cartilage is responsible for bone length) (Figure 6). In adults, ossification of the periosteum ensures physiological bone regeneration.
Posterior osteosynthesis with plates
Nacolumbar osteosynthesis is performed using plates perforated in different lengths, widths, shapes and thicknesses. The plates are screwed through the hole in the bone. Wires (wrapped wire sutures) and other fixation devices are also used for osteosynthesis for bone compression.



The most recent development in osteosynthesis is the angled stabilization plate (LCP). In addition to the threads on the screw that screw it into the bone and hold it in place, there are also threads in the holes in the plate and in the screw head so that the head of each screw is held securely in the plate. This type of fastening of the screws in the plate significantly increases the stability of the osteosynthesis.


For each segment of all long bones, angle-stable plates are made that are adapted to the shape and surface of the segment.


Plates for the proximal and distal humerus
Cap osteosynthesis allows open repositioning and excellent anastomosis (directly under visual control during surgery). It is therefore the osteosynthesis of choice for intra-articular and periarticular fractures, as the anatomy of the articular surfaces must be corrected to avoid mechanical hindrances to joint movement.
Periosteal osteosynthesis with external fixation devices
External periosteal osteosynthesis, which is carried out with the help of distraction-compression devices, occupies a special position. In most cases, this osteosynthesis method is used without exposing the fracture zone and enables repositioning and stable immobilization of the fractures. In this method, pins or rods are inserted through the bone and secured above the surface of the skin in an external fixation device. There are different types of brackets (unilateral, bilateral, sectoral, semicircular, circular and combined).

In Russia, the Ilizarov apparatus is traditionally used as the most functional, convenient and reliable external fixation device. GA Ilizarov was the first to invent an apparatus in which crossed spokes, passed through bone splints, are attached under tension to ring supports. The device is then placed outside the patient's body.
diagnosis
The diagnosis of acute periosteal inflammation is made based on the medical history and clinical signs, as the periosteal changes only become visible two weeks after the onset of the disease. Radiographs are the main instrumental method for diagnosing chronic periostitis and allow assessment of the shape, structure, outline, size and extent of the periosteal layers as well as the condition of the underlying bone and, to some extent, the surrounding tissues. Depending on the type, cause and stage of periosteal inflammation, needle-like, lacy, pectin-like, fringed, linear and other periosteal layers can be observed.
During long-lasting processes, the periosteum thickens significantly and fuses with the bone, so the cortical layer thickens and the volume of the bone increases. In purulent and serous periostitis, the periosteum detaches and a cavity forms. If the periosteum is torn due to a purulent fusion, a 'fringe tear' will be visible on x-rays. In malignant tumors, the periosteal growth takes the form of an overhang.
The X-ray examination provides information about the type, but not the cause, of the periosteum inflammation. An initial diagnosis of the underlying disease is made based on clinical symptoms, but depending on the symptoms, various tests may be used to make a final diagnosis. For example, if varicose veins are suspected, an ultrasound duplex examination is recommended, if rheumatic diseases are suspected, rheumatoid factor, C-reactive protein and immunoglobulin levels are determined, if gonorrhea and syphilis are suspected, PCR tests are carried out, etc.
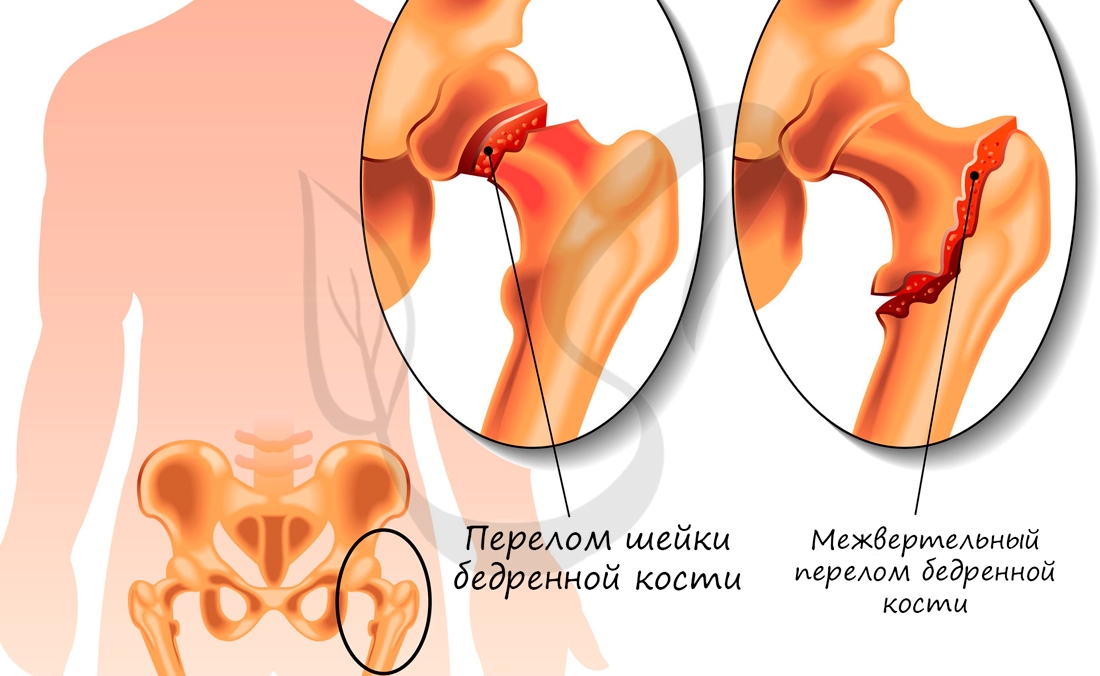
Diagnosis of hip fractures
If there is damage to the femoral diaphysis or another type of bone destruction of the femur, a diagnosis is required in order to develop appropriate treatment tactics. Which methods are used?

- X-RAY IMAGE. This method provides information about the type of injury, its location, and the presence and location of fractures. Multiple projection x-rays are recommended to provide more information about the hip fracture.
- MRI. An examination used for hip fractures that allows detailed visualization of the damaged area. It provides information about the condition of the bone and the adjacent soft tissues. The method is based on sound waves that travel through the body.
- Computed Tomography. A method that provides information about the type of fracture in the thigh, the condition of the arteries, veins, nerves and muscle tissue.
If a femoral fracture is due to an infectious component or a chronic disease, laboratory tests may be recommended. These provide information about the severity of the inflammatory process and the condition of the entire body.
Treatment
Immediately after the injury, anesthesia and immobilization of the injured limb are required. In most cases, a patient with a hip fracture requires surgical treatment. The severity and type of injury determine the further course of treatment:
- For traumatic neck injuries. The difficulty in treating such a femur fracture is the slow healing time. Often the patient does not fully recover, even after a long period of time. Osteosynthesis increases the chances of healing without consequences. Screw fixation is usually used. If necessary, replacement of the damaged area with titanium may be recommended. Hip arthroplasty is also used.
- Vertical injury. Therapy consists of fixing the bony area with a dynamic screw or a movable plate. Healing takes an average of three to six months. After this time, the screw is usually no longer removed. This type of hip fracture is typical for older people and carries a high risk of complications, making re-operation dangerous.
- If there is a diaphyseal injury to the thigh. Surgical nails or plates are used for immobilization. Traction may be recommended to restore function. Traction is indicated when there is a risk of dislocation and to fix the fragments.
In addition, conservative treatment is recommended. Anti-inflammatory drugs, analgesics and chondroprotective agents are prescribed.
Submerged osteosynthesis: use of pins
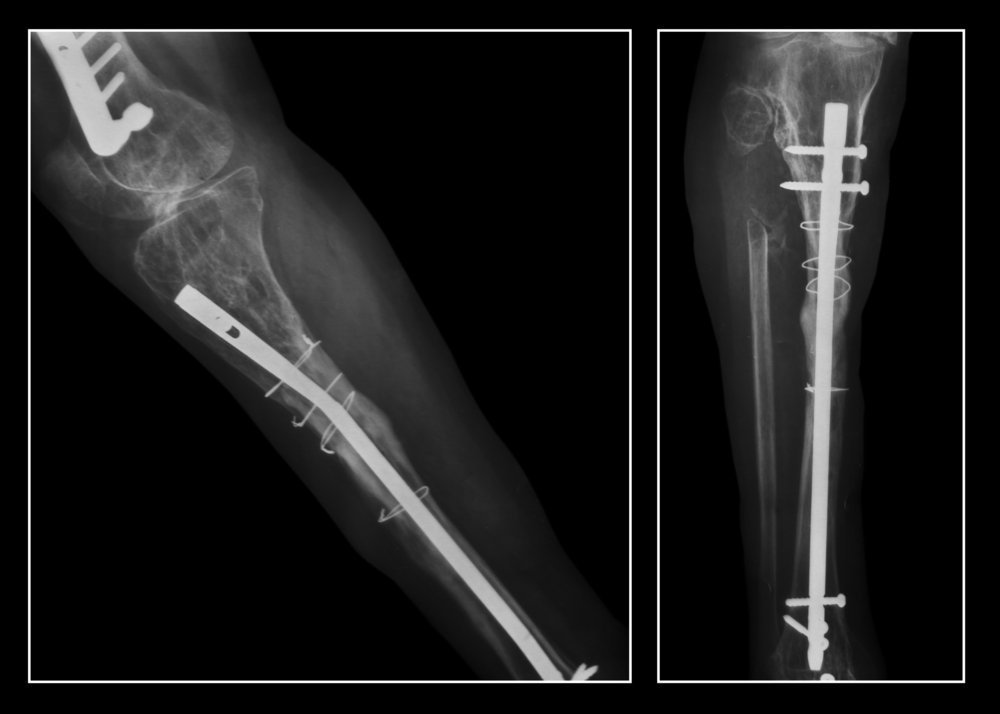
Submerged osteosynthesis is a technique in which fixation elements are inserted into the bone. For example, interlocking intramedullary osteosynthesis (IMS) is the gold standard for treating long bone fractures in the diaphyseal zone (the middle part of the bone). The shaft is inserted directly into the medullary cavity through a maximum 5 cm long incision and secured with transverse abutments. This method has several advantages over a plaster cast:
- Secure fixation that prevents movement of the fragment as the bone is essentially firmly attached to the rod.
- Minimal damage to the skin. In the fracture zone itself, the soft tissues are not affected at all, which means that the vessels that supply the injured bone are preserved and healing is accelerated.
- Already a day or two after the operation, the patient can put weight on the limb. In addition, traumatologists note that activity stimulates bone growth and fractures heal faster.
Longitudinal needles can be used for more than just fractures. You can e.g. B. can also be used to create a framework for a curved spine. The main problem with such operations is the use of curved rods, which previously had to be bent individually for each patient in the operating room. In 2013, the French company Medicrea solved this problem by developing the UNiD device, which, based on X-ray images, helps to create a rod with the desired bend for the patient. This shortens the operation time and at the same time avoids possible errors.
Immersion osteosynthesis: plates

Splinting – placing a plate on the bone – is another commonly used method to fix various damaged bones. This type of osteosynthesis can be successfully used to treat complex fractures, including joint fractures. The disadvantage is that a large piece of bone must be exposed. The operation is quite traumatic and can cause a number of complications. This includes an inflammatory process up to osteomyelitis.
However, in modern traumatology, angle-stable plates are used that are raised above the bone and enable a minimally invasive procedure with minimal incisions. The latest technology is the use of multi-axis screws (LCP), which can be inserted diagonally rather than vertically if necessary. This makes it possible not only to lift the plate, but also to fix it as accurately as possible. Even people with osteoporosis can undergo surgery, making the system suitable for treating joint fractures and other complex fractures in the elderly, such as: B. in injuries to the femoral neck or the proximal part of the shoulder.
The operation to insert the modern plates takes an average of 30 minutes, meaning the patient requires less anesthesia. After the procedure, the injured area can be put under strain and mobility returns, so that the affected person does not need a long rehabilitation phase with joint expansion after bone stiffening.
A special application of the plate is to immobilize ribs in the event of multiple injuries. This is one of the most serious types of fractures that are difficult to heal and often result in false joints, bone displacement, etc. In such cases, the insertion of a plate not only allows a return to normal life after just a day, but also avoids later complications. In rib osteosynthesis, the implants are often used for life and are not removed once the bone has fused. Nowadays, such operations are also carried out in Russia; in particular, a successful reconstruction of a rib fracture was carried out in Tomsk.
Fibrous periostitis
Develops gradually and takes a chronic course. It occurs as a result of years of irritation and manifests itself as a callus-like, fibrous thickening of the periosteum, which is closely attached to the bone. Observed at Periostitis on the shinbone in chronic shin ulcers, bone necrosis, chronic arthritis, etc. Significant development of fibrous tissue can lead to superficial bone destruction. In some cases, new bone formation is noted if the process continues for a long time. After the irritant is eliminated, a reversal of the process is usually observed.
It usually develops as a result of infection due to periosteal injury, through infection of neighboring organs (e.g. jaw periostitis due to dental caries) or through a hematogenous route. In metastatic periostitis, the periosteum of a long bone (usually femur, tibia, humerus) or several bones are affected at the same time. Purulent periostitis is an essential component of acute purulent osteitis. There are cases where the source of the infection cannot be identified.
Purulent periostitis begins with hyperemia of the periosteum and the appearance of serous or fibrinous exudate. The periosteum then infiltrates abscesses and easily separates from the bone. The fragile internal periosteum becomes saturated with pus, which then accumulates between the periosteum and the bone, forming a subperiosteal abscess. In an extensive process, the periosteum detaches over a large area, which can lead to malnutrition of the bone and superficial necrosis. Necrosis, which affects entire sections of bone or the entire bone, occurs only when pus infiltrates the intraperiosteal cavities. The inflammatory process can subside (especially if the pus is removed in a timely manner or spontaneously breaks through the skin) or spread to the surrounding soft tissues and bone substance (see osteitis).
Serous albuminous periostitis
An inflammatory process in the periosteum with the formation of an exudate that accumulates under the periosteum as a serous, slippery, albumin-rich fluid. The exudate is surrounded by brownish-red granulation tissue. The exudate and granulation tissue are covered by a thick membrane and resemble a cyst, which can mimic a cerebral hernia when located on the skull. The amount of exudate sometimes reaches 2 liters. It is usually located under the periosteum or as a cystic sac in the periosteum itself, or may even accumulate on the outer surface of the periosteum; in the latter case there is extensive swelling of the surrounding soft tissues. If the exudate is beneath the periosteum, the periosteum exfoliates, exposing the bone, and necrosis may occur, resulting in cavities filled with granulation tissue, sometimes with small sequestra.
The process usually occurs at the diaphyseal ends of long bones, most commonly the femur, less commonly the tibia, humerus, and ribs, and usually affects young men. P. often develops after trauma. Painful swelling occurs and the body temperature is initially elevated, but soon returns to normal. If the process is limited to the joint, joint dysfunction may occur. The swelling is initially hard, but may subside over time and fluctuate more or less visibly. The course is subacute or chronic.
causes
The formation and development of patellar tilt and subluxation can be caused by many factors, in most cases by several factors at the same time.
The main causes of this disorder are:
- Abnormal development of the lower limbs;
- Weakness of the medial ligament or excessive tension of the medial ligament that supports the kneecap;
- Weakness of the inner thigh muscle;
- Abnormal leg shape:
- X-shaped or valgus curvature of the tibia;
- High protrusion of the kneecap
- Internal rotation of the lower limbs and many others.
Anatomically, the kneecap has two ligaments on each side that hold it in place and prevent it from moving inward or outward. However, excessive tension in the outer ligament or weakness in the inner ligament can cause significant outward movement of the kneecap.
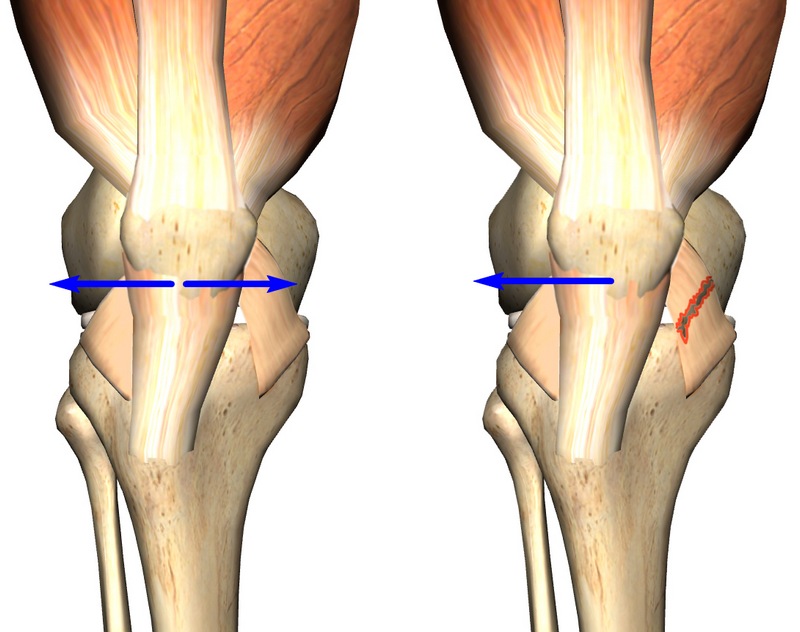
When the patella is normally centered in the condyle, the adhesion of the medial and lateral ligaments is strictly balanced. If there is an imbalance (e.g. severe ligament injuries and tears), the kneecap moves outwards due to the lack of tension compensation in the outer ligament.
In addition to the ligaments, the muscles also ensure the stability of the kneecap, including the medial ligament. As part of the quadriceps femoris, this muscle formation is also responsible for the stability of the kneecap and prevents it from moving outwards.
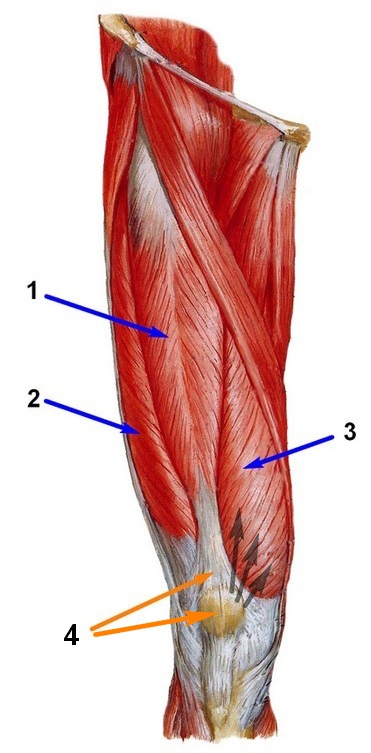
Figure 5 shows the muscles of the thigh (front view): 1 - straight, 2 - lateral, 3 - medial, 4 - intermediate. The black arrows indicate the insertion of the medial muscle.
Symptoms of subluxation and tilting of the kneecap
Pathologically abnormal sliding of the kneecap in the sulcus often leads to instability of the kneecap and more or less severe pain in the knee joint.
Although the feeling of instability is common, it is not the main indicator of patellar subluxation or tilting.
In addition to pain, it is not uncommon for a clicking sound to be heard during extension and flexion movements of the knee, which is caused by abnormal movement of the kneecap in the condylar sulcus.
It should also be noted that subluxation/deflexion of the kneecap is often preceded by damage to certain parts of the joint, e.g. B. due to complications during operations, previous dislocations, etc.
In the event of a pathological subluxation and/or tilting, the kneecap slides abnormally into the condylar sulcus. This causes significant damage to the cartilage that covers the kneecap and can lead to various types of injuries, including osteoarthritis.
In addition, if the patellar tilt and/or subluxation is prolonged, fluid can accumulate in the joint area and cause swelling.
Clinical Significance
External cracked hip syndrome can cause chronic pain in the lateral area of the hip joint above the trochanter of the femur. The pathophysiology of this disease involves thickening of the posterior aspect of the PST or anterior tendon fibers of the gluteus maximus muscle near its insertion site. This part of the insertion remains in the posterior part of the greater trochanter when the hip joint is upright and moves forward during flexion, adduction or internal rotation, triggering a 'cracking' mechanism. The clicking occurs because tense fascial structures adhere to the greater trochanter as it moves into the positions described above (3).
The clinical examination of PBT dysfunction is best done using the Ober test.
To perform the Ober test, the patient is asked to lie on the side opposite the side on which the test is to be performed. The side on which the symptoms occur must be facing upwards (towards the ceiling). The doctor then passively bends the knee to about 90 degrees. He then passively brings the hip joint into a flexed and extended position. The doctor then assesses passive range of motion via the FFT, keeping the hip in an extreme extension and extension position. The test is positive if pain, tension or a cracking occurs over the hip joint socket.
Treatment
Treatment typically begins with UBT traction, physical therapy, and physical therapy. The use of NSAIDs may be helpful in reducing inflammation. Surgery is a last resort and is used in cases that do not respond to the treatment described above.
Some corrective exercises are described below:
1 – Pelvic floor elevation with rubber band
An effective and simple exercise to start with is raising the pelvis from the supinated position with an elastic band. Researchers Choi and colleagues found that EMG activity of the gluteus maximus muscle was significantly increased during this isometric hip extension exercise compared to the same exercise without an elastic band when the angle of forward pelvic tilt was significantly reduced. They concluded that performing this isometric hip extension exercise with the resistance of an isometric rubber band could increase the EMG activity of the gluteus maximus muscle and reduce the angle of forward tilt of the pelvis during the exercise.
2 – Hip adduction
Hip abduction while lying on your side is an excellent exercise for isolating the gluteus medius muscle. Distefano and colleagues studied glute activation during regular exercise and found this exercise to be one of the best.
3 – Side step with an elastic band
Once you have isolated the gluteus medius muscle, you can incorporate it into a more functional exercise, the side step with an elastic band. Increasing hip abduction strength has been shown to improve female athletes' ability to control the relative position of the lower limbs. (14) In this exercise, the steps should be performed in a half squat and with the knees bent, which increases the activity of the gluteus maximus and medius muscles [4].
4 – Side elbow position
Read more:- Pain in the periosteum of the tibia.
- function of the fibula.
- Why the shin hurts.
- Which muscle extends the lower leg and flexes the thigh.
- Bones of the tarsal bone of the hand.
- Why does the femur hurt?.
- Corset for broken fibula.
- tibia and fibula.
