These simple and widely used methods will help you get back to normal walking as quickly as possible.

- Foot: causes, prevention and treatment
- Bunion: Causes
- Anatomy of the heel area
- Causes of Haglund's deformity
- Displaced fractures of the ankle joint
- Example 1.
- Why do transverse flat feet occur?
- Stages of flat foot formation
- Pharmacological treatment of ankle arthritis
- Anti-inflammatory drugs for ankle arthritis
- Cartilage protectant for ankle arthritis
- Antispasmodics and muscle relaxants for osteoarthritis of the ankle
- Warming agents in the treatment of ankle arthrosis
- diagnosis
- treatment of fibroids
- Conservative treatment
- surgical treatment
- prognosis and prevention
- Causes of pain and swelling in the ankle joint
- Sprained ankle, swollen ankle: what to do?
- Symptoms of Achilles tendon disease
- Diagnosis of Achilles tendon disease
- Gout (Tophus goutis)
- Treatment tactics:
- What should I do? Self-treatment or help from an orthopedist?
- video overview
Foot: causes, prevention and treatment
A bunion on the foot is a problem that worries many people. It also worries medical science, which coined the term 'bunion'. According to official statistics, almost 50 % of adults and elderly people are affected by a bunion. The cause of the appearance of bunions is not, as many believe, due to wearing tight, high-heeled shoes. Both men and women are at risk of developing this disease and there are many causes. Now let's find out how to prevent bunions or at least minimize the severity of their effects.
When you touch a tumor, it feels very dense and vaguely resembles a callus. Externally, it looks like a severe bone deformation, an appendage. To a certain extent this impression is true.
To understand the causes of bunions, you must first know the anatomy of the foot in general and the big toe in particular. The toe is formed by two joints. The largest joint is the metatarsophalangeal joint, which connects the largest bones of the toe. When healthy, the joint is straight. An illness occurs under stress, triggered by weight gain, uncomfortable shoes or standing work. The joint has to adapt to this load and deforms to help the body maintain balance.
X-rays of the affected joint show that the metatarsal moves outward while the phalanx moves in the opposite direction, toward the index finger. The changed shape of the joint causes constant pressure on the soft tissues, the layer of fatty tissue under the skin becomes thin, and the skin becomes rough, thick and calloused. This eventually leads to deformation of the foot and the formation of a characteristic club foot.
Bunion: Causes
Doctors refer to the degenerative process as the formation of a 'valgus foot'. As mentioned, weight gain and wearing uncomfortable, wobbly shoes are among the causes, but these causes are not at the top of the list. Both an overweight man and a woman wearing high heels can have completely healthy feet.
Medicine has not yet given a clear answer to the question of what causes corns. However, an analysis of statistics shows that the most common causes are:
- Genetic predisposition. The structure of bone tissue and therefore the tendency to form corns is hereditary;
- Traumatic impacts on the foot;
- Congenital deformities;
- Certain types of arthritis, particularly rheumatoid arthritis, which involve severe and deep inflammation;
- Poliomyelitis and other diseases affecting the nervous system and muscles.
Anatomy of the heel area
The heel bone is the largest bone in the foot. The Achilles tendon, the largest and strongest tendon in the human body, is attached to its bulb. The Achilles tendon pulls on the heel bone by contracting the posterior tibial muscles (calf muscles and flexors), allowing the sole of the foot to flex. This function allows us to walk, run, stand on our toes and jump. Between the heel bone and the Achilles tendon is the joint capsule of the hindfoot, which ensures that the tendon can move easily as the foot moves. Almost all joints have such a capsule, e.g. B. the elbow, the shoulder, etc.
The constant friction of the Achilles tendon causes the mucous membrane sac to become inflamed. This chronic stress over many months shifts to the posterior tubercle of the wrist and gradually pathological cartilage begins to form, which changes shape and often has sharp spikes. This can even be seen on an x-ray. The formation of this cartilage is due to the body's defense mechanism. The desire to strengthen the site of constant irritation and improve the gliding of the tendon. Unfortunately, the pathological cartilage is unable to do this. This creates a vicious circle.
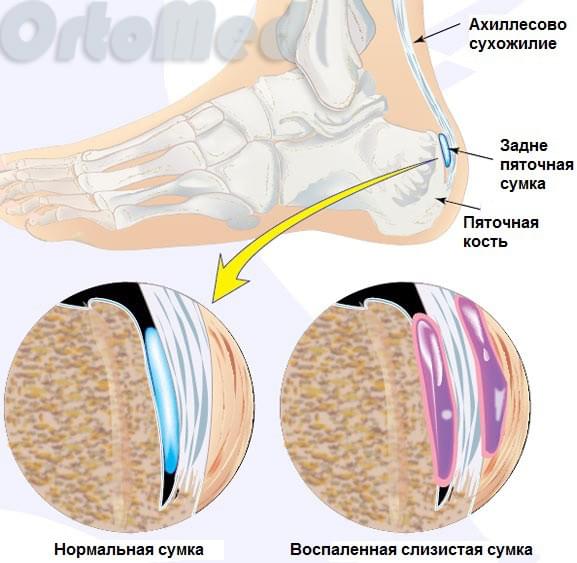
Pressure on the Achilles tendon capsule and tendon continues to increase, leading to increased inflammation, pain and swelling. Inflammation of the Achilles tendon capsule and tendon without bony deformation is called Achilles tendon bursitis (hindfoot bursitis). Bursitis usually precedes Haglund's deformity.
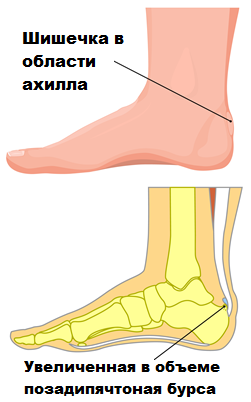
Patients pay no attention to the 'bump' and mistake it for a callus until it starts to hurt. This disease is usually difficult to treat conservatively. That's why it's important to see an orthopedist in the early stages of Haglund's disease.
Causes of Haglund's deformity
- A high arch can contribute to Haglund deformity because a person with a high arch causes the heel bone to tip backwards and the Achilles tendon to rub more against the normal heel bone, causing it to enlarge. This constant irritation eventually leads to inflammation of the capsule and tendon.
- Stiffness (reduced elasticity) of the Achilles tendon can also increase the risk of Haglund deformity because it rubs more against the heel bone. In contrast, a more elastic tendon puts less pressure on the pastern of the hind foot.
- A flat foot deformity or varus deviation of the heel bone alters the biomechanics of foot movement and increases the pressure of the Achilles tendon on the heel bone, triggering this pathological mechanism.
Haglund's deformity itself can occur without pain or symptoms of inflammation. There is only a pathological exostosis (heel nodule) on the back of the heel. This deformation usually does not cause problems with the function of the foot. In most cases, however, the deformity is accompanied by capsular and tendonitis and swelling. Patients then experience pain when walking and sometimes even when resting.
The syndrome can occur on one or both feet.
Signs and symptoms of Haglund's deformity include:
It is the pain that causes the patient to seek medical attention.
Displaced fractures of the ankle joint
Restoring the damaged structures in displaced fractures is the most important task of the orthopedist and traumatologist. These fractures require surgical intervention. Only with an internal fixator (plate or screw) can the bone fragments be securely fixed in the correct position.
After surgery and metal resection of the ankle fracture, a plaster cast is not required. The patient can perform active movements in the ankle joint. The patient is then taught to walk on crutches. Immediately after the operation it will not be possible to fully walk on the leg. The patient walks on crutches and puts only moderate strain on the extremity. The plates and screws remain in the patient's body until the fractures heal and the bone is completely remodeled.
Open fractures in the ankle area are a problem. These patients, particularly diabetics, are at high risk of wound necrosis and infection.
All open fractures of the ankle require surgery. When internal fixation poses a risk due to large wounds and soft tissue areas, the ankle can be temporarily immobilized with an external immobilization device. Once the soft tissues have healed, surgery is usually performed to join the bone fragments together in an anatomically correct position with plates and screws.
Improper application and adjustment of a plaster cast in the case of ankle fractures can often lead to skin problems including skin necrosis. Putting on a cast must be supervised by medical personnel to avoid such complications.
If the surgical technique is not correct, complications such as lack of fracture healing, joint stiffening and ankle osteoarthritis can occur.
Ankle osteoarthritis usually occurs when the fracture has not healed properly because the bone fragments were not positioned correctly during surgery.
Example 1.
A 54-year-old patient twisted her left leg while getting off a bus. The ambulance was called and she was taken to the trauma department, where she was given first aid and put in a cast. On the third day she presented to our clinic with increasing pain. She was examined by a traumatologist, and the X-rays taken in our clinic showed complete dislocation of the ankle fragments with outward subluxation of the foot.

After a detailed interview with the patient, it emerged that she had been discharged without medical advice as she was 'recovering' from the broken limb.
Due to the age of the injury and complications, the operation was performed on the seventh day. The fibula was immobilized with a pre-modeled plate, the medial malleolus with a hammertoe screw and a spoke.

Why do transverse flat feet occur?
In 8 out of 10 people, the arch of the foot drops due to overloading of the foot and reduced muscle tone. There is increased pressure on the inside of the foot, the toes and the foot becomes flattened. Main causes of foot deformity:
- Weakness of the connective tissue, genetic defects.
- Weakening of muscles and ligaments due to insufficient physical activity.
- Heavy lifting and carrying, weight training, overweight.
- Standing for long periods of time (tourist guides, salespeople, welders, waiters, hairdressers).
- High heels, tight and small shoes.
- Injuries to the ankle joint, torn tendons and ligaments in the arch of the foot.

Stages of flat foot formation
The orthopedist determines the severity of the foot deformity by examining the condition of the arch of the foot, the extent of movement, the impression of the sole and x-rays. Computer-assisted podometry (diagnostic foot loading) is prescribed for an objective assessment.
A total of four grades are distinguished, which are characterized by the following features:
- Slight foot fatigue, swelling, the big toe is not dislocated and there is significant redness on the side joint.
- Significant pain at the end of the day, the big toe deviates up to 20 degrees.
- The angle of deviation increases to 30 degrees, limited range of motion, no side arch. The pain spreads to the knees.
- The thumb deviates by more than 40° and can bend. Swelling, pain in the legs, lower back and head persist. Walking in normal shoes is difficult.
Pharmacological treatment of ankle arthritis
Drug treatment of ankylosing spondylitis has several directions:
- elimination of inflammation;
- elimination of pain;
- restoration of the cartilage that lines the joint;
- Elimination of degradation products from the joint and periarticular tissues;
- Improving tissue nutrition (stimulating blood circulation).
Secondary arthritis of the ankle also requires treatment of the underlying pathology, e.g. B. Antibiotics, cytostatics, antihistamines and primary medications for rheumatoid arthritis. The drugs are taken orally, topically or by intra-articular injection for ankle osteoarthritis.

Drug treatment for osteoarthritis can quickly relieve the pain and partially rebuild the cartilage in the joint.
Caution: Conventional painkillers for the treatment of ankle osteoarthritis should not be taken for more than 3 days before seeing a doctor, as they mask complications!
Anti-inflammatory drugs for ankle arthritis
Anti-inflammatory drugs for ankle arthritis can be steroidal (hormonal) or non-steroidal. Nonsteroidal medications (NSAIDs) are primarily used to relieve the symptoms of arthritis in the ankle but do not affect the cartilage. These include Artradol, Ibuprofen, Diclofenac, Ketoprofen, Meloxicam, Nimesulide, Indomethacin, Celecoxib and Lornoxicam.
If NSAIDs do not relieve pain, the doctor will prescribe SC (glucocorticoids) for a short time, usually in the form of injections for ankle arthritis. Treatment should be carried out no more than twice a year, strictly according to the doctor's instructions, since uncontrolled intake of HGs has a negative impact on the immune system and hormonal balance and can worsen the condition of the joints.
The most common agents used to treat ankle arthritis are hydrocortisone, prednisolone, methylprednisolone, and dipropane.
Cartilage protectant for ankle arthritis
Treatment of ankle arthritis with NSAIDs and HGs is symptomatic. However, the nutrients glucosamine and chondroitin, which are part of the joint cartilage and synovial fluid, are required for the regeneration of the joint. They ensure the correct viscosity of the synovial fluid and improve the elasticity and cushioning properties of the cartilage.
The most effective remedies for the treatment of arthrosis in the ankle are: artracam, artravir, chondroitin complex, dona, structam, protecon, artra, alflutop, movex active, teraflex.
Antispasmodics and muscle relaxants for osteoarthritis of the ankle
With arthrosis of the ankle joint, muscle tension and spasms often occur, which impair metabolism and cause exacerbation of pain syndrome.
To eliminate this, the following preparations are used: Drotaverin, Tolperisone, Tizanidine, Mydocalm, Baclosan.
Warming agents in the treatment of ankle arthrosis
Warming agents in the treatment of ankylosing spondylitis include ointments, creams, gels, compresses and lotions for external use. They have a locally irritating, pain-relieving, anti-inflammatory effect and improve tissue trophism.
diagnosis
The diagnosis of a hirgroma is usually made based on the history and characteristic clinical signs. X-rays may be recommended to rule out bone and joint pathology. In doubtful cases, an ultrasound examination, an MRI or a puncture of the hirgroma can be carried out. Ultrasound examination can be used to identify not only the cyst, but also its structure (homogeneous or fluid-filled), whether there are blood vessels in the wall of the hirgroma, etc. If a tumor mass is suspected, the patient can be referred for an MRI scan. This examination allows an accurate determination of the structure of the tumor wall and its contents.
The differential diagnosis of a hygroma is made with other benign and soft tumors (lipomas, atheromas, epithelial traumatic cysts, etc.) based on the location, tumor consistency and patient complaints. A hygroma in the hand area sometimes has to be differentiated from bone and cartilage tumors.

treatment of fibroids
Conservative treatment
Surgeons and orthopedic traumatologists treat the pathology. In the past, hygroma was treated by crushing or kneading. Some doctors practiced punctures, sometimes with simultaneous injection of enzymes or sclerosing agents into the hygroma cavity. Physiotherapy, mud, ointment dressings, etc. were also used. Some clinics still use these methods today, but the effectiveness of the treatment is not satisfactory.
surgical treatment
After conservative treatment, the recurrence rate is 80-90 %, after surgical removal the risk of recurrence is only 8-20 %. Based on available statistics, the only effective treatment method today is surgery. Indications for surgical treatment:
- Pain when moving or at rest.
- Limitation of the range of motion in the joint.
- Unsightly appearance.
- Rapid weight gain.
Surgical intervention is particularly recommended if the hirgroma is growing rapidly, as removing a large mass is difficult. Hirgromas are often located near nerves, vessels and ligaments. As the tumor grows, these masses begin to move and become more difficult to remove. Sometimes the operation is performed on an outpatient basis. However, during the operation, the tendon sheath or joint may be opened, so it is better to hospitalize patients.
The operation is usually performed under local anesthesia. The limb is bled by placing a rubber band over the incision. By exsanguinating and injecting anesthetics into the soft tissues around the hirgmans, the boundary between tumor and healthy tissue can be clearly delineated. For complex or large lesions, anesthesia or regional anesthesia may be performed. During surgery, it is very important to extract and excise the hematoma so that not even small areas of altered tissue remain at the incision site. Otherwise, hematoma recurrence may occur.
prognosis and prevention
Fractures of the ankle joint without dislocation usually heal well and do not cause any further discomfort to the patient. Mild pain associated with changes in the weather or significant stress on the joint is occasionally reported. Post-traumatic dystrophic pain syndrome - severe pain in the foot and ankle that makes standing on the foot impossible - can occasionally occur in properly treated displaced fractures. It is caused by vascular and neurotrophic abnormalities. Treatment is conservative – electroresection with novocaine, paraffin, novocaine blocks, physiotherapy and vitamin therapy. Recovery usually occurs within a year.
Unrepaired displaced ankle fractures result in persistent pain, deformity and swelling of the joint, limitation of movement, instability and unsteadiness when walking and limping. A deforming inflammation of the joint quickly occurs, making it even more difficult to support and move the ankle. In such cases, reconstructive surgery is required, which may include removal of scar tissue, osteosynthesis with various metal structures, bone grafting, and ligament reconstruction. Prevention consists of injury-reducing measures.
Causes of pain and swelling in the ankle joint
A fast lifestyle, heavy physical activity, overexertion and excess weight are factors that make the joint vulnerable to injury. In the case of the ankle, this risk is increased by uncomfortable women's shoes.
If the foot is sprained, there is a high risk of many unpleasant consequences in the form of ankle swelling:
If a person has twisted their ankle and the ankle is swollen, it is important to determine what type of injury affected the limb.
- A sprain is a closed injury in which the fibers that make up the ligament are torn and the patient experiences pain and discomfort but can barely walk. Ligaments take at least two weeks to heal.
- Torn and torn ligaments are a more serious and painful injury. You can't walk, your ankle is swollen. A touch, let alone a kick on the limb, is not acceptable. When a tear occurs, a popping sound is heard, followed by an acute pain syndrome. These injuries cannot be treated alone, therapeutic and surgical measures are required, and an immobilizing bandage should be applied for up to one and a half months.
- An ankle bruise is the easiest to treat. It is also swollen, but everyone knows what to do from childhood. Elevate the leg and apply a cold compress. If you suspect a more serious injury, you should consult a doctor.
- During a subluxation, the ankle joint is slightly displaced and the ligaments are damaged. It is very likely that conservative measures will not be enough and surgery will be necessary.
- A joint dislocation is characterized by a severe displacement (up to 40 degrees) of the bone and damage to the joint capsule. The pain is unbearable, the swelling is severe and the limb is disabled to the point of being dislocated. This can only be done under anesthesia and not at home. If the capsule is severely damaged, a surgeon will be called in.
- An ankle fracture can occur with or without bone displacement and can be open or closed. Treatment may last a month or longer.
Sprained ankle, swollen ankle: what to do?
Regardless of how serious the injury is, first aid may be as follows
- Immobilization of the foot with a splint - real or self-made
- Avoid stepping on the foot to avoid further damage.
- Apply ice to relieve the pain. This also reduces swelling. Such a compress can be applied for up to 20 minutes without harming your health. Do not put the ice pack back on for an hour.
- If possible, it is advisable to use a tight bandage.
- It is better to keep your leg elevated.
After first aid, a doctor should always be consulted and the condition of the ankle and the entire foot assessed.
Symptoms of Achilles tendon disease
Swelling and pain in the affected area, thickening of the tendon, stiffness of the foot and ankle, limping, etc. are typical symptoms of Achilles tendon disease.

In Haglund's disease, the specialist can feel the posterior bursa and the protrusion of the heel bone.
Diagnosis of Achilles tendon disease
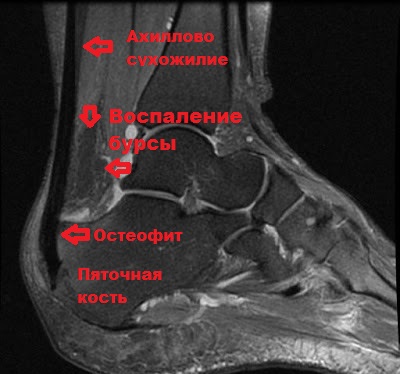
The orthopedist/traumatologist is responsible for the treatment of injuries and diseases of the Achilles tendon, who takes the anamnesis, carries out clinical examinations and assesses the general condition of the ankle and foot.
The resulting X-ray (MRI) can be used to identify a number of problems in the Achilles tendon area, if any. These include excessive calcification in this area, various types of degeneration and inflammation, deforming changes (spurs), etc.
Gout (Tophus goutis)
Gout is a disease associated with a disorder of purine metabolism. In gout tophus, deposits of uric acid salts occur in the tissues.
- Gout most often affects men, and tophus is the main reason for consulting an orthopedist;
- The location of the tophus varies greatly and extends from the toes to the ulna.
- Their size varies from a few millimeters to gigantic proportions;
- Tofu tumors are compact and painless;
- With chronic trauma to the footwear, they can become inflamed, infected and infectious;
- When tofus open, a white mass (urate crystals) is released from them;
- 15-20 % of gout patients carry urate stones.
 |  |
| The appearance of a foot with gout tofu | |
|---|---|
Treatment tactics:
- After conservative treatment and stabilization of the ureteral level, removal of the tophus is indicated.
- The operation is best performed when the tophus is small, without waiting for growth or purulent complications.
- The operation is localized and individualized depending on the size and location of the tophi.
What should I do? Self-treatment or help from an orthopedist?
If you know how different the thickenings on the feet can be, you also know that the treatment is different!
In some cases, physiotherapy, ointments and the selection of comfortable footwear are enough, in others, treatment of the underlying disease that manifests itself in the bunion is necessary, and in still others, surgical correction of the deformity and removal of the bony protrusion is required.
However, instead of visiting a qualified podiatrist for an accurate diagnosis and appropriate treatment of the disorder (tumor), many people look for easy ways to remove the 'bone'. But there are so many suggestions for treating a 'tumor', from magical remedies and ointments to insects and urine.
Modern medicine, of course, does not deny the effectiveness of folk remedies in certain cases, but in order to use them correctly, you need to know what you are treating. It is also important to know that two or more diseases can be combined.
Unfortunately, we often confuse wishful thinking with reality. Self-medication is not an option to understand the causes of the disease and implement effective treatments.
A qualified podiatrist can help you get rid of the condition (lump) quickly and without wasting time, without endangering your health.
video overview
Read more:- What is the name of the orthopedist in the health center?.
- What is the heel of a shoe called?.
- Heel bone tendon sac in Latin.
- Root nodules in children.
- The ankle bruise is where the picture is taken.
- dislocation of the ankle.
- Structure of the human ankle.
- Heel bone human anatomy photo and description.
