There are a number of symptoms that make it urgent to see an orthopedist, as they can indicate a serious condition. If these symptoms are observed, specialist medical help is essential:
- Diagnostics in trauma orthopedics
- Article
- What the recording looks like
- Diagnostics in traumatology and orthopedics
- What diseases require regular monitoring by an orthopedist?
- When should you take your child to an orthopedist?
- Diagnostics in orthopedic traumatology
- Conservative treatment of diseases of the musculoskeletal system
- (2) Is it very serious if a child has not started to sit/walk by the date specified in the norms?
- 4: Are strollers harmful?
- When to See an Orthopedic Dentist
- Preparation for the visit and the course of the visit to the orthopedic dentist
- methods
- diagnosis
- When should you see an orthopedist?
- What does an orthopedic surgeon treat?
- What does a pediatric orthopedist do?
- What does the pediatric orthopedist treat?
- spine and thorax
- hip joints and feet
Diagnostics in trauma orthopedics
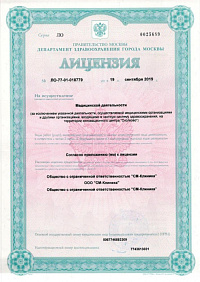
Orthopedic diagnostics at SM Clinic is characterized by a comprehensive approach, precision and efficiency. The methods used provide essential information about the condition of the bone structures, the cartilage tissue, the capsule and ligament apparatus of the joints. In connection with the clinical symptoms, the location of the injury can be clearly localized and the correct diagnosis can be made.
The excellent diagnostic possibilities, multiplied by the high professionalism of our doctors, allow us to choose the appropriate treatment tactics and ensure high-quality treatment of diseases of the musculoskeletal system in SM Clinic.
Article













What the recording looks like
First of all, the orthopedist listens to your complaints carefully. It is important to tell the doctor as much as possible, as the conversation will provide basic information for a preliminary diagnosis. It is advisable to prepare the answers to the following questions in advance:
- the nature of the symptoms;
- the time of their occurrence;
- possible reasons for the development of pathological symptoms;
- medications taken to alleviate the condition and the results obtained;
- heredity;
- whether there have been previous hospitalizations or surgeries for the condition;
- whether there has been trauma;
- for working patients: the nature of their work.
After assessing the complaints, the orthopedic surgeon carries out a physical examination. The specialist assesses the patient's gait, limb alignment, and the presence of joint deformities and tremors. To determine the range of movement and active mobility of individual joints, the doctor can ask the patient to perform various activities - bending, squatting, etc. When checking passive mobility, the orthopedist moves the patient's limbs. In this way, any pathological resistance is also detected.
Diagnostics in traumatology and orthopedics
To clarify the diagnosis in traumatology and orthopedics, the following laboratory and instrument-based diagnostic methods are used:
- General blood test;
- urine test;
- biochemical analysis of blood;
- rheumatic examinations;
- X-rays;
- computed tomography or magnetic resonance imaging;
- arthroscopy;
- arthrography.

The scope of the examination is selected individually, depending on the nature of the complaints, the general condition of the patient and other factors. At AlterMedica, the diagnosis of diseases of the musculoskeletal system is carried out with modern equipment at an expert level. Thanks to the state-of-the-art equipment, examinations are quick and effective. Orthopedists and trauma surgeons are able to detect various diseases at an early stage.
An individual treatment plan is drawn up based on the examination results. Conservative and surgical treatment methods are used in traumatology and orthopedics. The scope of treatment depends on the detected disease, its severity, the presence of concomitant diseases and the patient's age.
AlterMedica's orthopedic traumatologists are bound by international standards when treating diseases of the musculoskeletal system. The drugs prescribed are proven to be effective. Operations are only recommended if there is a corresponding indication.
A consultation and any questions can be arranged by telephone. A recall form is available on the website. Leave your contact details, our receptionist will call you back shortly to make an appointment.
*Promotions and discounts are possible, please ask the operator or the reception for the exact price.

What diseases require regular monitoring by an orthopedist?
Chronic diseases of the musculoskeletal system often lead to exacerbations and require regular medical monitoring by an orthopedist. Patients should see a doctor regularly if they have been diagnosed with any of the following
- osteochondrosis;
- Rheumatoid arthritis;
- osteoarthritis in various joints;
- femoral neck fracture;
- spinal injuries;
- Knee or shoulder dislocations.
Preventive visits to an orthopedist/traumatologist are advisable for those who play sports or engage in extreme outdoor activities in order to timely eliminate micro-injuries and prevent possible problems.
When should you take your child to an orthopedist?
It is important for parents to know when to visit an orthopedist, because a timely visit to the orthopedist allows to correct anomalies, even congenital. It is important to take the baby to the orthopedist:
- if the newborn's hip is crooked (congenital dislocation);
- if the baby's head is constantly tilted towards one shoulder (torticollis);
- when the child walks with a 'raking' foot (clubfoot);
- If the child tires easily when walking and their gait seems sluggish (flat feet);
- If the child walks visibly stooped;
- If the child complains of pain in the legs, arms, back or neck.
This article is for educational purposes only and does not constitute scientific material or professional medical advice.
Diagnostics in orthopedic traumatology
When diagnosing diseases of the musculoskeletal system, the following examinations are mainly carried out:
- Clinical examination;
- X-ray (digital quality with tomosynthesis, for patients up to 300 kg);
- CT (Siemens CT scanner with up to 128 slices);
- MRI (full body diagnosis in 1.5 hours);
- ultrasound diagnostics;
- diagnostic arthroscopy;
- Laboratory diagnostics: clinical and biochemical blood tests and other tests.
Receipt of the analyzes from 07:30 a.m. The results are sent to the practice personally and by e-mail.
Conservative treatment of diseases of the musculoskeletal system
- Pharmacological treatment (including intra-articular injections of pharmacological agents, blockades);
- Physiotherapeutic treatments (including laser therapy, ultrasound, magnetic therapy, myostimulation, etc.).
- massages;
- Manual therapy;
- reflexology;
- orthoses.
- joint arthroplasty;
- arthroscopic treatment of joint injuries;
- corrective surgery for foot pathology;
- osteosynthesis of bone fractures;
- corrective osteotomy;
- resection of flank bones;
- surgical treatment of muscle and tendon injuries;
- Treatment of consequences of injuries;
- Treatment of spinal injuries and deformities.
(2) Is it very serious if a child has not started to sit/walk by the date specified in the norms?
Every child is different. If it's checked regularly by the family's orthopedist, who doesn't find anything abnormal, there's no need to panic about the deadline. Let's set a time frame: A child can sit up at 10 months at the latest and learn to walk independently at the latest at 18 months. However, routine check-ups with the family's orthopedist should not be neglected. The doctor should continue to monitor the child's musculoskeletal system in the future. It is all the more important to clear up unnecessary doubts and worries again and again.
It is good for the child to walk barefoot on uneven surfaces (pebbles, grass, sand, orthopedic mats), when the ligaments and muscles of the feet work, preparing to support the arches of the feet. On a smooth, level surface, the child should walk with arch support – in orthopedic preventive shoes. So, it is worth buying home orthopedic shoes to avoid flat feet and other anomalies. Remember that children love their parents and imitate them in everything. If you wear orthopedic shoes, your child will surely follow your example.
4: Are strollers harmful?
While your child crawls on all fours, it trains its musculoskeletal system so that it can learn to walk independently. It is not advisable to use a baby walker when your child is on their feet. A child in a stroller has limited mobility, and unprepared will put a lot of strain on the child's spine, especially the lumbar spine, and your child will not learn to balance. Let your child crawl more - this is an excellent preparation of the musculoskeletal system for learning to walk.
Only your general orthopedist can determine with absolute certainty whether you have flat feet. In the orthopedic office, the doctor scans your feet with a special computer device (a plantograph) that accurately shows if there are any abnormalities in your feet. By determining the exact foot parameters, the podiatrist can prescribe custom orthotics to prevent or treat foot problems.

When to See an Orthopedic Dentist

The reasons for visiting an orthopedic dentist vary. If severe caries occurs, this is a serious reason to visit the dentist - in addition to the aesthetics, the function of the teeth can also be affected. Every tooth plays an important role in a person's life, and tooth decay affects the functioning of the entire body. An orthopedic dentist is also necessary to timely protect a tooth from tooth decay. It is important to remember that not every type of denture can permanently restore a tooth. Many dentures are only responsible for restoring part of the tooth. If the tooth has become brittle and tends to decay, timely treatment by the dentist can prevent further damage. Correcting small caries in the tooth crown also requires professional help. Unfortunately, not all people can boast of having perfect teeth. In some cases, veneers can be a good solution to the problem. High-quality veneers can help hide dental imperfections.
The orthodontist deals with microprosthetic, removable, fixed and conventional fixed methods of tooth restoration. Microprosthetics are procedures in which a decayed tooth must be brought into a presentable condition. The orthodontist uses inlays and trays to replace part of the tooth. The front teeth in particular require this type of care. Veneers are particularly popular today. They have a lifespan of about 10 years. Fixed dentures are more extensive and durable than microprostheses. With crowns and bridges, the prosthetist restores the chewing function of the teeth. Orthopedic practice shows that when a single tooth is missing, a crown is an excellent solution, while when there are several missing teeth, a bridge is much more effective. Not only older people can need removable dentures. Teenagers can use them too. The orthodontist places a prosthesis in place of the lost tooth, avoiding distortion of the healthy teeth. Depending on the patient's individual dental situation, the specialist can make a full or partial denture.
Preparation for the visit and the course of the visit to the orthopedic dentist
During the visit, the orthopedist examines the patient's mouth and listens to their complaints. The examination can be visual or instrumental. The dentist then takes impressions and photos of your teeth. If necessary, a consultation with an oral surgeon is arranged. Based on the information received, the dentist draws up a treatment plan for the patient.

Depending on the individual characteristics of the patient's teeth, the dentist selects appropriate methods of examination. A panoramic photograph of the teeth, an orthopantomogram or an X-ray of one or more teeth may be proposed. A few months after the prosthetic work, the patient can have a follow-up examination to assess the work done.
After the instrumental diagnosis, the orthopedic dentist may consider consulting other specialists, e.g. B. an orthodontist recommend. After collecting all the data needed for the treatment, the dentist develops a treatment plan for the patient. The orthopedist is responsible for ensuring that the prosthesis is correctly fitted and made.
methods
In practice, the dentist most often uses the techniques of removable and fixed dentures, rarely combining both techniques. The decision is made individually in each case and depends on the clinical situation and the needs of the patient.
Fixed or permanent dentures are fixed dentures. This includes:
- Crown.
Crowns are made of different materials (ceramic, gold, composite, etc.) and are cemented in place of the original crown, which is the visible part of the tooth and is made of dentin and enamel. - Bridges.
They are inserted between adjacent teeth, called 'anchor' or 'abutment teeth', to fill a gap in a row of teeth.
Fixed dentures can be attached to a natural tooth or to an implant. In this case one speaks of a conditional prosthesis.
Removable dentures are used when several teeth are missing and/or implants cannot be placed.
- Removable full dentures.
They are used when most teeth are missing in one or both jaws at the same time. - Partly removable prostheses.
They are useful when one or more teeth are missing in a row to correct aesthetic defects.
In the case of prostheses, a distinction is made between:- Inplanar dentures. Reconstructs sections of a row of teeth, the cheapest. The downside is that the main chewing force is on the gums;
- Immediate dentures. A temporary prosthesis placed after tooth extraction and before the final restoration;
- Corrugated dentures (from 'bust' - bow) are the most comfortable and durable of all dentures and can be used for full or partial dentures. One benefit is that chewing pressure is evenly distributed over the gums and remaining teeth.
A separate group is the so-called microprosthetics - the reconstruction of a damaged tooth with a small prosthesis. The most popular treatments are veneers - ceramic or porcelain fillings that hide imperfections and correct the shape of the tooth and the color of the enamel.
diagnosis
The orthopedic dentist does not treat teeth in the usual sense: he does not do fillings, he does not treat nerves and he does not clean root canals. However, a diagnosis is also required as part of his visit.
At the first consultation, the doctor will outline the treatment picture and inquire about the patient's options, preferences and lifestyle. This helps in choosing the best option (or multiple options) for prosthetic treatment.
In some cases, the orthopedist may refer the patient for further consultation with other specialists (general practitioner, orthodontist, etc.).
When should you see an orthopedist?
Depending on the purpose of the visit, a consultation with an orthopedist can be therapeutic or preventive, and depending on the number of visits, it can be an initial or follow-up consultation. An appointment can be made alone or with a referral from another doctor (traumatologist, rheumatologist, neurologist, etc.) to clarify the diagnosis, confirm or rule out an orthopedic pathology and decide on an operation or prescribe therapeutic agents. As a rule, the first visit to the orthopedist is a planned visit, rarely an emergency examination is required:
- Scheduled Consultation. It is indicated when symptoms of diseases of the musculoskeletal system appear for the first time or when an already diagnosed orthopedic disease has progressed. Reasons can be: shortening or deformation of a limb, curvature of the spine, occurrence or worsening of pain, functional impairment, swelling of the joint area.
- emergency advice. Required if symptoms appear suddenly or worsen. Usually required for severe pain, support and movement difficulties or fluid accumulation in the joints as a result of arthritis of various origins.
A follow-up visit is scheduled to review laboratory and instrumental findings, make a definitive diagnosis, establish a list of treatment regimens, monitor disease progression over time, adjust the treatment plan, and decide whether hospitalization and surgical intervention are necessary.
What does an orthopedic surgeon treat?
Orthopedists treat developmental anomalies, acquired diseases of non-traumatic etiology and long-term consequences of injuries to bones, joints, muscles, tendons and ligaments. Sometimes their area of expertise overlaps with that of other specialists. For example, post-traumatic deformities are treated by both traumatologists and orthopedists, spinal disorders are treated by neurologists and neurosurgeons, and patients with certain joint disorders may be treated by orthopedists or rheumatologists. There are the following groups of diseases that require consultation with an orthopedist:
- Congenital anomalies of the limbs. Various malformations (absence or underdevelopment of a limb segment), congenital contractures, hip dysplasia, congenital hip dislocation, etc.
- foot deformities. A large and diverse group of pathologies of congenital and acquired origin, including clubfoot, various forms of flat feet (including valgus deformity of the first toe), deformities caused by previous foot trauma, paresis and paralysis.
- spinal curvatures. Poor posture, scoliosis, pathological kyphosis and lordosis, mixed forms of spinal deformities (kyphoscoliosis).
- degenerative diseases.Arthrosis of various etiologies (post-traumatic, congenital and acquired diseases), osteochondrosis, spondylosis, spondylarthrosis, spinal instability.
- Pathologies of soft tissue structures. Lesions of tendons, tendon insertions and tendon sheaths (tendinitis, enthesopathies, bursitis) that are occupational or caused by other orthopedic diseases.
Due to the non-specific nature of symptoms and the availability of orthopedic care in the capital, orthopedists are often the first to diagnose rheumatic diseases (rheumatoid arthritis, ankylosing spondylitis), benign and malignant bone and soft tissue tumors, which are then treated by rheumatologists and oncologists. Sports medicine is an important branch of orthopedics.
What does a pediatric orthopedist do?
The pediatric orthopaedist diagnoses and treats diseases of the musculoskeletal system of various origins and their prevention. This doctor treats children from birth to 18 years of age.
A pediatric orthopedic dentist may also be needed to care for a child with misaligned baby teeth, as the baby teeth affect later development of the permanent dentition. The orthopedist corrects the teeth visually and can detect tooth misalignments at an early stage of tooth formation.
The newborn undergoes an initial orthopedic examination in the maternity hospital, and then it is advisable to visit the orthopedist for the following examinations:
Subsequently, it is advisable to take the child to the orthopedic department at the age of 3, 6 and 9 years. Regular examinations allow the pediatric orthopedist to monitor the development of the child's skeleton and muscular corset, which reduces the risk of developing acquired disorders: scoliosis, flat feet, osteochondrosis and others. It is particularly important to consult a specialist during periods of active growth and increased physical activity: e.g. B. before the start of the first grade (6-7 years) and during puberty (11-13 years).
An unscheduled visit to the pediatric orthopedist should be made if the following symptoms are observed
- Asymmetric skin folds on the shoulders and hips in children under 1 year;
- Delayed physical development: the child has difficulty turning, sits up late and cannot walk
- Restricted hip movements: When changing or getting dressed, it is easy to observe that the child's legs 'do not open';
- Unequal length of upper or lower limbs.
In children 3 years and older, symptoms of musculoskeletal disorders include:
- Difficult, unsteady gait: the child has difficulty standing and is constantly reaching for a support (walls, chairs);
- Clubfoot: abnormal position of the feet when moving;
- noticeable stooping or 'hunching', both when walking and when sitting;
- visible changes in the joints: swelling, puffiness, redness of the skin, rash, blueness of the skin;
- child's complaints of muscle or joint pain;
- Physical weakness: may manifest as poor coordination in motor play or 'everything falls out of hands';
- head posture;
- Numbness of the extremities or unusual sensations in the hands and feet (tingling, 'goosebumps')
- Local increase in body temperature;
- Injuries: severe bruises, dislocations, fractures and torn ligaments.
What does the pediatric orthopedist treat?
The pediatric orthopedist treats a wide range of congenital and acquired anomalies of the musculoskeletal system.
Doctors treat the following congenital deformities of the upper limbs:
- Syndactyly - complete or partial fusion of the fingers caused by a genetic abnormality. It is diagnosed at birth, cannot be treated with drugs, and requires surgery;
- Polydactyly - an inherited abnormality with an increased number of fingers on the hands;
- Sprengel disease, or abnormal (high) shoulder position – characterized by the irregular shape of one of the shoulder blades: it becomes shorter and wider, resulting in a constant forced elevation of the shoulder;
- Obliquity – the hand is tilted away from the ulna at an irregular angle, which can be due to pathology of the bones themselves as well as abnormal tendon structure.
The pediatric orthopedist also treats congenital malformations of the lower limbs. One of the most common is hip dysplasia. This is a total or partial dislocation of the hip caused by an abnormal shape in the uterus.
Congenital orthopedic anomalies are the result of abnormal fetal development influenced by poor genetics or a serious illness in the mother during pregnancy. Birth injuries can lead to musculoskeletal problems in the infant.
Other common conditions that a pediatric orthopedist deals with include:
- Clubfoot - a deformity of the foot that causes it to deviate from the direction of the shinbone and stand at an irregular angle to it. The heel is turned inwards or outwards. This anomaly is congenital and can be well treated;
- Scoliosis is a curvature of the spine caused by structural bone defects, trauma, or other causes. It manifests itself in a hunched, asymmetrical position of the shoulder blades and ribs and limited movement of the trunk;
- Osteochondrosis is a structural disorder of the intervertebral discs, leading to their deformation and reduced function. The disease affects different parts of the spine and the symptoms vary accordingly. The patient complains of pain in the back, chest or neck and suffers from limited mobility;
- Arthritis is an inflammation of the joints that is usually infectious in children. The affected area becomes inflamed and painful, and the joint loses mobility;
- Torticollis is a condition characterized by forced supination of the head. It is caused by a shortening of the neck muscles or a skeletal deformity;
- Flatfoot is a foot deformity with a reduced arch. The condition is both congenital and acquired and is classified into different grades depending on the severity of the pathology.
spine and thorax
All these curvatures form in the first few months of life. If the curves of the spine are correctly formed, a spring effect is created and the spine can later absorb axial loads due to the good cushioning of the vertebrae. However, if only one of the curves is flattened, this effect disappears and the spine has to endure irrational loads, which leads to many diseases, e.g scoliosis (lateral curvature of the spine), osteochondrosis (limited mobility of the spine), etc.
So let's go back to the investigation. Let's place the child on their stomach with their legs bent ('frog position') and make sure the spine is in the midline. Sometimes a baby can have something called 'infantile scoliosis'.infant scoliosis'It is usually accompanied by neurological symptoms (muscle dystonia, hypertonia) and when corrected, the spine returns to its normal position.
Sometimes examining the child in this position reveals a posterior deviation of the spinal axis, referred to as 'lumbar kyphosis'. Lumbar kyphosis of the spinea; it is most common in babies who are born large and passes fairly quickly if the baby is held properly for the first three months of life, not attempting to sit up or stand on their feet (many parents love it to make the baby 'jump up' - but this is not possible).
Parents should know that the curvature of the spine develops gradually: First, the baby begins to hold its head - this contributes to the development of cervical lordosis. In this context, it is important to remember that the use of pillows in children interferes with the correct development of this curvature. As the child begins to sit up (which it gradually does if not disturbed by adults), thoracic kyphosis and lumbar lordosis develop. If a child is placed in a chair too soon, instead of the desired slouch, they may have a thoracolumbar kyphosis (known as 'hunched back').
hip joints and feet
Let's get back to the orthopedic examination of our child. The next stage, which is no less important, is the hip joints.
To assess the function of the hips, lay the child on his back, bend his legs at the knees and try to spread them.
This should not be sudden and violent. The child may not like this, tensing the muscles and not allowing the legs to straighten. If done correctly, it is usually possible to spread the legs so that the knee joints touch the table on which the child is lying.
The restriction of abduction can have various causes. The most common (and easily treated) cause is. disc spasm. (inner thigh) muscles. In this case, wide swings (that is, when the baby's hips are not pressed together but are a certain distance apart), warm water baths, and physical therapy can help. If the mother finds that hip abduction is more restricted on one side, this should be reported to the doctor.
The next stage of the examination is to check the symmetry of the buttock folds and the length of the legs; to do this, the baby should be placed on his stomach. You should see a specialist if you notice any of the following, among other things Asymmetry of the gluteal folds or different leg lengths.
Similar symptoms can occur with different diseases, and only a correct diagnosis will help you to initiate the right treatment in time and keep your baby healthy.
When you are sure the hips are properly formed and their function is unaffected, take a look at the feet. Pay attention to the placement of the foot, which should be in a central position. If you notice that the foot is not pointing straight ahead, but is rotated slightly in or out in the horizontal plane (ie there is what is known as 'foot twist'), you should check the position of the foot. foot rotation), it is important to start massaging the foot as soon as possible. A special massage can correct the deformity of the foot in the first month of life. If the foot deformity is more severe, the foot can be corrected with bandages before the child begins to walk. Remember, any minor foot deformity can be easily corrected in early childhood, but once your child can walk, much more effort needs to be put into treating it.
Read more:- Who is the orthopedist?.
- What an orthopedist treats and what symptoms to report.
- What is another name for an orthopedist?.
- What is an orthopedist?.
- What is the name of the orthopedist in the health center?.
- How much does a prosthetic foot cost?.
- What the surgeon examines in teenagers.
- What the orthopedist pays attention to.
