It is better to seek the help of an orthopedist at an early stage in order to prevent further development of the disease and protect yourself from serious problems.

- flat feet
- Description of the types of flat feet
- Longitudinal-transverse flatfoot: who is suitable for surgical treatment?
- What happens before the operation?
- Diagnosing flat feet
- Transverse flatfoot surgery
- Combined treatment
- Treatment and prevention of flat feet in children
- Doctors on the causes of transverse flatfoot
- Pain is a major symptom of transverse flatfoot
- Removal of the bunion
- Why shouldn't you forget to make an appointment with your orthopedist for a check-up?
- Prevention of flat feet in children
- Treatment
- prevention
flat feet
Flatfoot is a disorder of part of the musculoskeletal system characterized by deformity of the arch of the foot.
It is characterized by an impairment in gait biomechanics that can lead to complications in other important parts of the system (knee joints, spine).

A healthy foot has a longitudinal arch (at the inner edge of the foot) and a transverse arch (between the bases of the toes). Medicine knows the longitudinal and transverse flatfoot.
The former is a deformation of the longitudinal arch, the latter is a deformation (flattening) of the forefoot. There is a combined form of the ailment, in which the patient has both types of flat feet at the same time.
Thanks to the correct formation and function of the arch of the foot, a person maintains balance, which protects the body from impact when walking.
Healthy feet are able to perform many important functions that are compromised by flat feet:
- Human adaptation to the unevenness of the ground, the pavement
- the distribution of the total body load when walking;
- the ability to cushion (reduce) the impact with the ground during movement.
In some cases, flat feet are combined with heel pronation, supination, and forefoot retraction. This is a flat valgus deformity. Many patients confuse this pathology with flat feet.

Description of the types of flat feet
There are different types of flat feet:
- Congenital form (rarely occurs, since it is considered an intrauterine pathology);
- Acquired flat feet can be divided into several groups and can occur in all age groups, they can be traumatic (the disease develops after a foot injury, impact, damage to joints, tendons), rickets flatfoot (it develops after rickets, the disrupts the normal formation of the skeletal system of the feet; bone tissue loses its former strength, under the influence of daily stress soft tissues and muscles are deformed), paralytic flatfoot (the disease develops after poliomyelitis, partial atrophy of the foot muscles, joints);
- Static flat feet (caused by hereditary predisposition, long periods of sitting at the computer, leading to muscle and ligament weakness, unsuitable footwear, obesity, high leg loads, pregnancy, constant wearing of high heels, platforms).
Longitudinal-transverse flatfoot: who is suitable for surgical treatment?
The surgical treatment of longitudinal-transverse flatfoot depends on the stage of the disease. The indication for surgical treatment should be made very discreetly, since the disease can also be treated conservatively. Due to the dynamic situation of the arch of the foot, a good result can be achieved with regular training and special exercises to build muscle.
Surgical treatment of longitudinal-transverse flatfoot is recommended only if the patient experiences severe pain in the foot for a long time, and the pathology negatively affects the patient's quality of life. Chronic tendinitis or a rupture of the tendon of the posterior tibialis muscle make an operation unavoidable. Surgery is also required for spastic hindfoot deformities associated with ankle arthritis.
What happens before the operation?
Before the operation, the doctors Doctors at the joint clinic The doctors in the joint clinic carry out a comprehensive clinical examination. One of the most important diagnostic signs of longitudinal-transverse flatfoot is a lateral deviation of the forefoot caused by a change in the longitudinal arch of the foot, with almost all toes becoming visible when viewing the foot from behind. Doctors call this phenomenon Too many toes sign. In patients without foot pathology, all toes point forward. A standing X-ray clearly shows the bone deformity and can confirm the doctor's concerns.
Another indicator of a compound flatfoot is a test called the single heel rise sign, which gives an indication of the condition of the posterior tibial muscles. To do this, the doctor observes the alignment of the foot from behind while the patient is standing. Injuries to the tibialis muscle are likely when the ankle axis is tilted inward. Another method for diagnosing the tibialis posterior is magnetic resonance imaging (MRI). A podometric study is recommended to analyze the degree of loading on the foot when standing and walking.
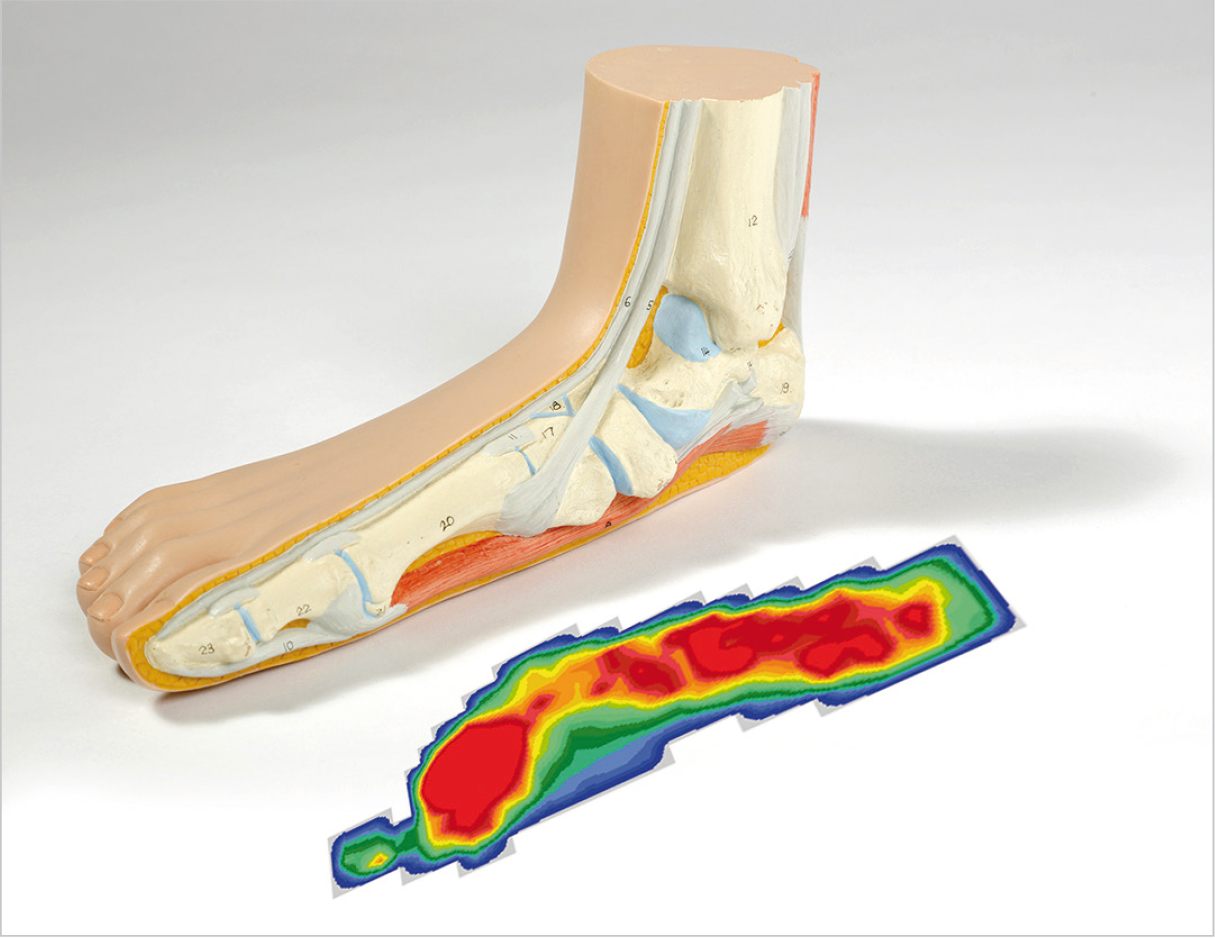
Longitudinal-Transverse Flatfoot: Measurement of the size and condition of the foot (podometry). The deformation of the longitudinal arch of the foot is determined by podometry: the pressure (area marked in red) is more evenly distributed than in a healthy person. With a normal longitudinal arch of the foot, only the area around the heel and fingertips is loaded. The longitudinal-transverse flatfoot causes a flattening of the arch of the foot.
Diagnosing flat feet
The orthopedist performs a visual inspection of the foot and orders x-rays. X-rays are used to make a definitive diagnosis by determining the extent of the disease and the type of flatfoot. Depending on the diagnosis, the specialist chooses a treatment method (conservative or surgical) and draws up a treatment program.
It is quite difficult to get rid of flat feet with conservative treatment methods. It is possible only at a very early stage of development, when flat feet are discovered at a young age (3-5 years). If it is possible to teach the child at this time certain exercises that need to be done for a long time, then the likelihood of flat feet in the future will decrease. In addition to exercises, flat feet in children can also be corrected with orthoses, orthopedic aids and special footwear. Unfortunately, in most cases this does not happen and flat feet continue to develop.
Basically, there are no conservative therapies that can cure flat feet in adults. We can use customized orthopedic insoles, various physiotherapy treatments, massages, physiotherapy and acupuncture, but all of this only serves to stop an already existing deformity and thus slow down the development of flat feet. However, when we already have flat feet, and especially when they have reached an advanced stage, only surgery can cure them.
Of course, the term 'surgery for flat feet' raises fears, but today there are surgical procedures that, through small incisions, can eliminate flat feet quickly and with little trauma. The bony structures are brought into the anatomically correct position with the help of a special implant. The patient walks for several years, during which the ligaments and muscles get used to this condition, and then the implant is removed.
Transverse flatfoot surgery
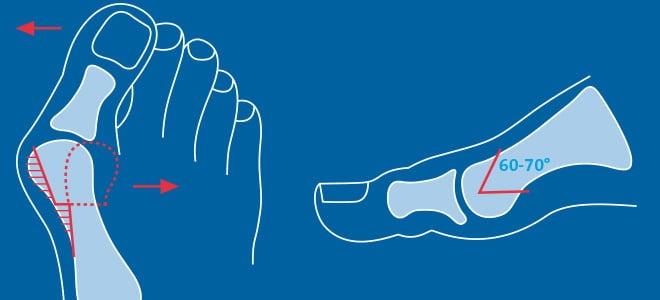
In the case of transverse flatfoot, doctors perform the following surgical procedures On the forefoot. Generally, they perform an osteotomy (chevron or scarf) of the first metatarsal. If necessary, they supplement this with plastic surgery of the muscles, ligaments and tendons. Surgical interventions can correct not only transverse, but also valgus deformities of the foot.
Doctors often find patients with exostoses (bony prominences) and hammer toe deformities of toes II-V. The former are removed using the Schede method, while the latter are corrected by resection or osteotomy. In patients with transverse flatfoot, several interventions can be carried out at the same time. This approach allows qualitative correction of the existing defects.
Combined treatment
The transverse-longitudinal flatfoot is the most severe form of the disease. Both arches of the foot are deformed at the same time and the foot becomes completely flat. This pathology is difficult to treat.
The goals of combined flatfoot surgery are.
- restoration of the arch of the foot;
- fixation of the bone in a stable position;
- Correction of deformity of the first toe;
- removal of exostoses;
- Correction of the hammer toe misalignment.

Surgery of longitudinal-transverse deformities.
In the case of a transverse-longitudinal deformity, several interventions are performed at the same time. For example, the patient undergoes a Schede operation, a Scarf osteotomy, and arthrodesis of some metatarsal joints at the same time. Doctors usually try to do everything in a single surgical procedure.
The recovery time after these surgeries is longer than in other cases. Fortunately, the patients do not need a cast or crutches. In the worst case, they have to go with fixation spokes, which are removed along with the threads after 2 weeks.
Severe longitudinal flatfoot requires posterior tibial tendonoplasty and marginal subcutaneous tenotomy of the Achilles tendon. After this procedure, the patient is placed in a plaster cast and can only walk on crutches.
Treatment and prevention of flat feet in children

How to treat flat feet in children? Adequate physical activity alone is an excellent prevention against various orthopedic problems in children. What makes sense? Walking barefoot is very useful, especially on uneven ground (sand, gravel, just dirt). Special orthopedic mats are a good addition to the home. It makes no sense to wear shoes at home if there are no orthopedic problems, but this will only make the child uncomfortable. It is better to buy your child sensible (preventive) shoes. The most important criteria that will help you choose the right shoes for your child. Tight, form-fitting back, flexible, pliable and corrugated sole, small heel 0.5-1.0 cm, preferably the shoes should be leather, acceptable in height, but not too high, they should not be too tight (the big Toe should not be pressed too much against the rest), they should not 'pinch' (margin 0.5-1.0 cm), they should not be worn over others.
Asymptomatic locomotor flatfoot alone does not require treatment. Children with symptomatic movement flatfoot can be treated with special individual orthoses (rational footwear) and especially with exercises for children with flatfoot to train their body balance.
Conservative treatment of children with rigid flat feet is ineffective and is aimed at reducing pain before surgery. Choosing comfortable footwear, limiting physical activity, and weight control are necessary. There are numerous surgical treatment options for rigid flat feet. The choice of surgical treatment in children is always individual.
If you have any doubts about the correct shape of your child's feet, it is always best to see an orthopedist.
Doctors on the causes of transverse flatfoot

Doctors assume that in most cases, transverse flatfoot is caused by weakness in the lower leg and foot muscles. Slightly less often it is caused by injuries (fractures) of the bones of the foot or their weakening due to various pathologies (rickets, etc.). When the muscles or ligaments are underdeveloped, the patient's weight is not properly distributed on the foot, overloading the bones and phalanges of the foot. As a result, the foot splays and becomes flattened.
There are a number of factors that contribute to the development of a transverse flat foot:
- Individual predisposition to muscle and ligament weakness (hereditary);
- Severe nervous system abnormalities (including cerebral palsy);
- Inadequate metabolism leading to nutrient deficiencies in the musculoskeletal system;
- Early onset of rickets;
- History of severe lower limb injuries (particularly below the knees) resulting in forced stepping and abnormal weight distribution;
- habit of wearing fashionable footwear, especially high heels;
- Systematic stress on the lower limbs (obesity, frequent weight lifting, frequent pregnancy).
Transverse flatfoot can also be congenital. In this case, a malformation of the feet during fetal development is assumed to be the cause.
Pain is a major symptom of transverse flatfoot

At the initial stage of development, transverse flatfoot does not affect the patient's life. However, in the absence of adequate treatment, the pathological processes cause a number of unpleasant symptoms. Initially, the patient feels a feeling of heaviness in the foot, which occurs after standing or walking for a long time and stimulates physical activity. Over time, these symptoms become more and more noticeable. Sometimes patients can pinpoint the location of the pain - it is the area where the first and second toe meet.
As the disease progresses, the symptoms begin to appear constantly, regardless of exertion or time of day. There is marked swelling of the fingers and toes, sometimes extending to the knuckles. The severity of this symptom can vary, sometimes the swelling is barely noticeable. The thickening of the arch of the foot causes severe pain in the calf muscles, which become rock hard. Corns, hard and dry calluses form on the foot. These corns are in the areas that are most stressed. Corns most commonly appear on the heels, the outside of the foot, and the toes and the balls of them. As flatfoot progresses, the foot becomes wider and wider, so that the patient can no longer wear conventional shoes because they become uncomfortable and too tight. Trying to walk in fashionable shoes causes severe discomfort and pain.
The classic symptom of a transverse flat foot is a valgus deformity of the big toe. This condition is also known as 'valgus' or 'bunions' of the foot.
Removal of the bunion
In transverse flatfoot, the metatarsals separate and the joints gradually become crooked, resulting in a valgus foot deformity, or 'bunions'. The joint can protrude either from the inside (change of the first toe) or from the outside (Taylor deformity, change of the fifth toe).
Since the constant bending of the joint leads to the accumulation of excess bone tissue, it is not possible to fix the 'ball' by simply correcting the foot. The overgrowth must be removed separately. In modern orthopedics, open surgery is only used for advanced flat feet. Minor deformities are treated with minimally invasive methods. Hypertrophy is removed through punctures no larger than 4 mm in size, which heal fairly quickly.
Why shouldn't you forget to make an appointment with your orthopedist for a check-up?

Although the diagnosis is not made until the age of 5, the doctor can already determine whether the child has a predisposition to the development of any pathology. Based on regular observations, he can determine what needs to be done to prevent flat feet from developing. The doctor will tell the parents what needs to be done individually and to what extent so that the child's feet develop properly.
Three visits to the orthopedist in the first year of life and every six months thereafter, even if everything is normal.
Don't trust the advice of shop assistants in children's shoe stores. They are more interested in sales than in the health of their little customers. Some stores have special devices that are said to be used to check children's feet for flat feet. Don't rely on readings from these simple devices. They usually indicate some degree of flat feet in everyone as they are not intended to diagnose but to increase sales of children's orthopedic shoes. A diagnosis can only be made by a doctor and only after a comprehensive examination. Advice on choosing shoes is also best provided by an orthopedic doctor.
Prevention of flat feet in children
Our ancestors rarely had flat feet. This is because they mainly walked a lot and went barefoot. Flat feet are rarely seen in country children and barefoot Africans. But in sedentary city dwellers, this pathology is - everything and more.
- Sedentary lifestyle, lack of physical activity;
- excess weight, which increases the load on the foot;
- Wearing the wrong shoes or another child's shoes;
- rickets in childhood;
- injuries;
- Trauma; hereditary predisposition.
Reducing the risk of developing this disease:
- Foot and toe massage. This should first be done by a professional, then the parents themselves will learn the proper techniques.
- Warm foot baths with sea salt.
- Walking barefoot on grass, pebbles, seabed or special massage mats. You can make a special path at home using stones, chestnuts, round sticks or logs.
- Special exercises that children like to do in the form of games. These include rolling different sized balls or massage rollers, walking on your toes, on your heels, on different sides of the foot. The doctor selects the exercises, their order and number of repetitions, and this should be done individually.
- Application of paraffin and ozokerite, electrophoresis.
- Avoid obesity, eat a healthy diet and get plenty of exercise. However, avoid putting too much strain on the foot and lifting heavy weights.
- Swimming, skating and in-line skating.
- Wear suitable footwear and, if necessary, special orthopedic insoles.
We will deal with the last point separately.
Treatment
The best results of conservative treatment are achieved with mild deformities. To correct a mild deformity:
- wearing orthopedic shoes or insoles – these are selected by the doctor after a thorough examination of the feet;
- taking multivitamin complexes;
- exercises at home on orthopedic mats or relaxation balls;
- General strengthening body massage with emphasis on the lower limbs;
- Pine and salt baths once a week.
Moderate deformities are corrected in the same way. Therapy includes magnesium and B and D vitamins. Parents are advised to let their child do daily exercise and massage at home.
Stage III and IV valgus requires long-term correction. Therapy includes:
- wearing orthotics, braces and bandages;
- Pharmacotherapy: analgesics, antihistamines, anti-inflammatory drugs, anti-infectives, venotone and phleboprotective agents, hormonal ointments, nerve conductors, muscle relaxants, etc. The choice of drugs depends on the patient's condition and the cause of the deformity;
- massages Performed daily by a certified specialist. It contributes to the normalization of muscle function and reduces pain and spasticity;
- Physiotherapeutic treatments – in order to achieve a positive therapeutic effect without putting undue stress on the body. Physiotherapeutic treatments include electrophoresis with calcium preparations, paraffin therapy, darsonvallisation, acupuncture, medicinal baths, cryotherapy, mud packs;
- therapeutic exercises. The choice of exercises depends on the etiology of the deformity. The complexes can be performed both in the gym with a trainer, and at home. Maximum recovery can be achieved with a combination of home exercises and physical therapy with a specialist.
If conservative treatment doesn't work, the doctor decides to have surgery. Surgical interventions are aimed at restoring the function of the lower limbs or relieving the symptoms. These techniques are commonly used:
prevention
The main cause of the development of a foot defect in a child is the lack of attention to motor functions. From the first days of the child's life, parents need to take care of the health of the lower limbs. Preventive measures include:
- A balanced daily diet with lots of fruit, vegetables and protein;
- Daily walks in the fresh air;
- sufficient healthy sleep;
- Comfortable everyday footwear that meets international standards;
- Gymnastic exercises, fitball or orthopedic mat exercises;
- taking an aqueous vitamin D solution;
- Daily firming massages;
- walking barefoot on rough surfaces;
- Hardening in the sun and in water.
A common cause of valgus is early weight bearing on the feet. Don't try to get your child to their feet or teach them to walk without their initiative. Annual consultations with a neurologist and trauma surgeon can identify and correct valgus deformities in children.
Read more:- Longitudinal and transverse arches of the foot.
- Which ligaments strengthen the transverse arch of the foot?.
- Flatfoot Deformity.
- Which doctor treats flat feet?.
- flat feet (valgus foot).
- Icb flatfoot.
- flat foot pronation.
- flatfoot μb.
