Gymnastics strengthens muscles and bones, reducing the risk of fasciitis progression and accelerating the patient's recovery. Gymnastics also stimulates lymphatic drainage, which prevents or reduces swelling.
- Treatment of heel spurs with MAG-30
- What is Plantar Fasciitis?
- When is it better to proceed?
- Basic recommendations of doctors
- symptoms
- diagnosis
- Diagnosis of plantar fasciitis, how to recognize it
- Heel pain: which doctor is responsible?
- Treatment of plantar fasciitis
- Surgical treatment of plantar fasciitis
- How to treat plantar fasciitis at home
- Prevention of plantar fasciitis
- Treatment of heel spurs
- Conservative therapy
- prognosis and prevention
- How to treat plantar fasciitis with folk remedies?
- Plantar fasciitis (sole spur)
- symptoms
- See also:
- Plantar fasciitis (heel spurs)
- Etiology:
Treatment of heel spurs with MAG-30
Heel spurs (or plantar fasciitis) are diseases of the musculoskeletal system and are a consequence of upright posture: around 10 % of the population have symptoms of plantar fasciitis in one form or another.
The disease requires compulsory treatment: a quarter of all diagnosed cases result in partial loss of mobility. The disease is characterized by pain in the heel bone caused by microtrauma to the longitudinal fascia. The sensation of pain occurs when the foot is supported or put under pressure and increases in the morning or after prolonged rest or exercise. According to statistics, more than 70 % of those seeking help are urban women over 40.
It's important to remember that heel pain is not necessarily caused by heel spurs. Only a doctor can make an accurate diagnosis after analyzing the patient's complaints and X-ray images.
What is Plantar Fasciitis?
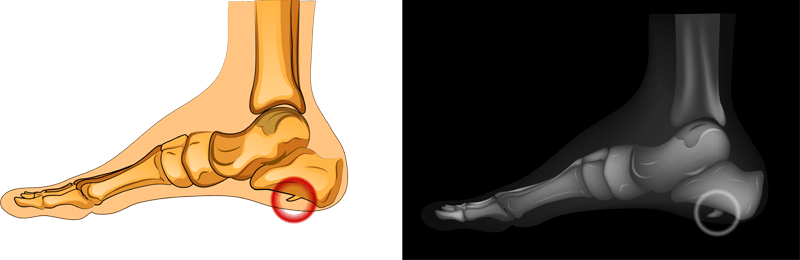
Dense connective tissue is attached to the heel bone and the heads of the metatarsal bones, which provides support and the formation of the longitudinal arch of the foot. This tissue is called the plantar fascia, and its inflammation at the point where it connects to the heel bone is called plantar fasciitis or heel spur.
plantar fasciitis is caused by inflammatory and degenerative changes in the longitudinal fascia tissue: overstretching and resulting inflammation of the longitudinal ligament. The painful tissue is caused by a bony protrusion (spur) at the end of the heel that can be anywhere from a few millimeters to a centimeter in size.
The tissue of the plantar fascia is most stressed where it borders the calcaneal tuberosity. Running or walking puts a lot of stress on the foot, and micro-injuries often occur in this area and repair themselves. However, when the foot muscles do not function properly and the connective tissue is overstretched, the repair function is impaired, and constant injury to the plantar fascia increases the risk of a compensatory reaction: periosteum and bone remodeling. The compensatory reaction manifests itself in a characteristic growth: On X-ray images, the heel spur looks like a thorn (osteophyte) growing forward.
When is it better to proceed?
A special feature of plantar fasciitis is that the heel pain begins in the morning after getting up. During the night, the micro-tears in the plantar fascia heal by keeping the feet still and relaxed.
However, if the person gets up after waking up and puts weight on the foot again, new micro-injuries appear in the foot and pain sensations arise. The pain only goes away when the foot is warmed up. For this reason, gymnastics for heel spurs begins immediately after getting up.
If the deformity of the affected area is severe, exercises before bedtime are also necessary. This helps to consolidate and reinforce the results of the overall treatment of the condition. After the exercises, the orthosis should be worn overnight.
Gymnastics for heel spurs before bed normalizes blood circulation in the foot, which promotes the healing of microfractures of the heel fascia during sleep. The orthosis prevents compression of the fascia, which promotes healing of the tear and avoids pain in the morning.
Basic recommendations of doctors
To maximize the effect of heel spur exercises, there are a few principles to keep in mind. This includes:
- The correctness and fluidity of the exercises performed. Failure to do so can aggravate the course of the disease and cause further damage to the heel area of the foot. Rapid movements lead to pain syndrome.
- Increase physical activity gradually. At the beginning, simple and short exercises are carried out. Immediate heavy strain on the foot should not be considered.
- Preparation for training. The patient should warm up the muscles of the lower leg, calf and foot before starting exercise.
- Regularity of training. Systematic training helps to achieve a therapeutic effect on heel spurs. If the exercises are performed infrequently, the fascia contracts, making further LFC more difficult. Regular exercise keeps the ligaments stretched.
After exercise, doctors recommend fixing the foot at a 90-degree angle to keep the fascia stretched. An elastic bandage or orthosis is used for this purpose.
symptoms
Although many patients with plantar fasciitis have a heel spur, the spur does not always cause pain. Nearly 10 percent of adults have a spur, but only 5 percent experience foot pain. Therefore, in most cases, treating heel pain does not require removal of the spur.
The most common symptoms of plantar fasciitis are:
- Pain in the lower part of the foot in the heel area
- Pain with the first steps after getting up in the morning or after a long period of rest, e.g. B. after a long drive. The pain subsides after walking for a few minutes
- Increased pain after (not during) exercise or physical activity.
Heel spurs often cause no symptoms. However, a heel spur can cause occasional or chronic pain - especially when walking or jogging if inflammation develops in the area where the spur formed. As a rule, the cause of the pain is not the heel spur itself, but rather a soft tissue injury originating from the spur.
Many patients describe Pain associated with heel spurs and plantar fasciitis as a pin protruding from the sole of the foot when they get up in the morning, and this pain later develops into a dull ache. People often complain that the stabbing pain occurs immediately after getting up or after sitting for a long time.
diagnosis

After collecting the patient's medical history and complaints, the doctor examines the foot: presence of a hollow foot, pain area in the heel area, presence of restricted movement in the foot. Instrumental examination methods may be required to verify the diagnosis. X-rays give a clear picture of the bony tissue. This examination method can be used to rule out other causes of heel pain, such as fractures or osteoarthritis. A heel spur is clearly visible on x-rays.
MRI is a very informative method that can be used to clearly visualize not only the bony tissue of the foot, but also the soft tissues (ligaments, cartilage), which is important for the diagnosis of plantar fascia, Achilles tendon damage or cartilage damage in osteoarthritis.
Ultrasound examination is also often used Diagnosis of heel spurs Although the image quality is inferior to MRI, ultrasound can also be used to diagnose plantar fasciitis and plantar fasciitis, such as monitoring the effectiveness of treatment, which is completely safe.
Diagnosis of plantar fasciitis, how to recognize it

It all starts with a visual examination, palpating the heels to check their sensitivity and find the source of the pain. At this stage, the doctor should rule out other problems such as: B. a fracture of the heel bone.
During the physiological examination, the foot is flexed and the fascia is felt at the same time. The pain usually increases when the big toe is moved or wiggled, even if it is not supported. Another characteristic symptom of plantar fasciitis is the redness and slight swelling of the heel.
The therapist will also examine neurological parameters:
A foot x-ray or MRI scan may also be recommended to rule out structural bone damage, rheumatoid arthritis, and bone spurs.
Heel pain: which doctor is responsible?
An initial examination should be carried out by a surgeon at your local health center. He or she will then likely refer you to an orthopedist/traumatologist.

Treatment of plantar fasciitis
Home Treatment: Rest, kinesiotaping, and anti-inflammatory ointments are the main treatment methods for plantar fasciitis. These are often enough to relieve the pain.
The most important thing is to take your time and not put too much strain on your sore feet. Recovery can take up to 1.5 months.
If this therapy is not enough, the doctor may prescribe corticosteroid injections directly into the damaged ligaments.
Another treatment for plantar fasciitis is electrophoresis in combination with steroid ointments.
Physiotherapeutic treatments such as massage, stretching of the Achilles tendon and strengthening of the lower leg muscles are the key to eliminating the condition. They help stabilize the foot and reduce pressure on the plantar fascia. If the problem is aggravated by excess weight, diet and weight loss are also necessary.
Surgical treatment of plantar fasciitis
Admittedly, the disease progresses quite gradually and often only becomes noticeable when a full-grown osteophyte (calf spur) has formed. Therefore, surgery is indicated if the pain and burning in the heel does not subside with conservative methods and persists for six to 12 months.
In this case, the surgeon performs partial removal of the inflamed tissue to reduce tension. However, a side effect of such a procedure is a weakening of the arch of the foot and a partial loss of function.
If the patient has trouble flexing the foot even after further dislocations, the doctor may recommend partial resection of the calf muscle. The aim of the operation is to lengthen the muscle to make the ankle more mobile and to partially relieve pressure on the plantar fascia.
The main complication of the operation is partial damage to nerve endings and chronic pain in the legs. Therefore, surgery should only be considered as a last resort.
How to treat plantar fasciitis at home
As a rule, conservative treatment of fasciitis at home is sufficient as long as the doctor's instructions are followed and the feet are not put under strain. Unless heel spurs develop, plantar fasciitis usually heals within two to three months.
Prevention of plantar fasciitis
The most common preventative measures are as follows:
- Wear comfortable, well-cushioned footwear, especially when exercising;
- Avoid walking barefoot on cold surfaces;
- Control your weight and reduce it if necessary;
- Always stretch the foot and ankle tendons before exercising;
- Avoid self-medication - at the first symptoms a specialist will act more effectively.
Plantar fasciitis is a serious problem due to the pain syndrome. Although there are a variety of therapies available, none of them guarantee a complete cure. Good results and ease of use make Kinesio taping a promising treatment option for this pathology.
Treatment of heel spurs
Treatment is conservative and is usually carried out on an outpatient basis. Surgical interventions are only carried out in cases of long-term and severe disabilities.
Conservative therapy
Non-pharmacological methods play a crucial role in the treatment of heel spurs. Medications are rarely prescribed. Instead they are used:
- Optimization of foot load. Patients are advised to limit standing time and walking time. With corrective exercises, most patients experience pain relief within six months, regardless of other therapies.
- Therapeutic' exercises. A series of exercises for heel spurs is aimed at stretching the soleus aponeurosis. They are carried out for a long period of time in the absence of intense pain syndrome.
- Orthopedic devices. According to experts, custom-made orthoses are the most effective. The use of standard orthoses and insoles is possible. Longitudinal orthoses can be used at night to lengthen the plantar fascia.
- immobilization. Indicated for severe, non-painful pain. An orthopedic shoe is placed over the leg so that the foot can be supported. A limitation of this technique is that prolonged fixation is undesirable due to possible muscle atrophy.
- Administration of corticosteroids. It quickly eliminates even severe pain, but increases the likelihood that the plantar fascia will tear and is therefore only performed if other therapeutic measures have failed. The injection is given from the inside of the foot in the area where the pain is most severe. A course consists of a maximum of three treatments; the interval between treatments should be at least six months.
Shock wave therapy is considered a promising treatment for heel spurs. Taping is effective, but is usually only used in the initial phase of therapy before insoles are made due to the necessary bandages and discomfort to the patient.
prognosis and prevention
The prognosis is favorable. The pain usually disappears completely within 1-2 years. The exostosis remains lifelong, but does not cause any unpleasant symptoms afterwards. In chronic synovitis, the duration of the disease can be prolonged. Prevention includes normalizing body weight, avoiding overuse, using comfortable footwear and early treatment of diseases that increase the risk of heel spurs.
2 Plantar fasciitis: diagnosis and treatment / Sereda AP, Moisov AA, Smetanin SM // Siberian Medical Journal (Irkutsk) – 2016 – № 4
How to treat plantar fasciitis with folk remedies?
It should be borne in mind that the use of folk recipes cannot eliminate the pathology. Treating plantar fasciitis with folk remedies can only relieve the symptoms.
Rub a fresh cabbage leaf with honey and apply to the problem area. Wrap the foot with cling film and a warm cloth. Leave the compress on overnight. Carry out 6-10 treatments.
Black radish or potato compresses are no less effective. The vegetables should be chopped. A good effect can be achieved by placing clay soaked in warm water on your feet overnight. The treatment is carried out in courses of 10-14 treatments.
Dissolve the salt in warm water in the specified proportion. It is recommended to use water hot enough not to cause burns. The feet are immersed in the solution for a quarter of an hour. Socks should be put on after the treatment. It is recommended to do this before bedtime.
Plantar fasciitis (sole spur)


Plantar fasciitis or heel spur is a pathological process in which osteophytes form at the insertion site of the plantar tendon (plantar tendon) on the heel bone. Its formation is caused by constant trauma to the attachment site of the aponeurosis during excessive stress on the foot.
symptoms
Plantar fasciitis manifests itself as pain in the sole of the foot when walking. It usually occurs after periods of rest, less often after long periods of walking.
The pathology is diagnosed based on the patient's complaints and clinical examination. X-rays, ultrasound, MRI and CT examinations are carried out to confirm the diagnosis.
Treatment for plantar fasciitis aims to relieve the inflammation and includes:
Physiotherapeutic treatments, gymnastics courses and wearing orthopedic shoes show good results.
The qualified orthopedic traumatologists of the Medic Clinic in Khabarovsk provide effective and comprehensive treatment of heel spurs.
See also:
Please ask our specialists about possible contraindications.
The information contained on this website is not a public offer.
Make an appointment, advice for all your questions
Plantar fasciitis (heel spurs)
Plantar fasciitis (heel spurs) is a condition whose main symptom is pain in the heel that occurs or increases with exertion. In most cases, the pain syndrome is caused by inflammatory and degenerative changes in the sacrum (plantar bone).
Plantar fasciitis (heel spurs) – is a condition in which the main symptom is pain in the heel that occurs or increases with exertion. In most cases, the pain syndrome is caused by inflammatory degenerative changes in the longitudinal fascia (plantar fascia). More rarely, heel pain is directly related to permanent trauma to the surrounding soft tissues caused by bony outgrowths (heel spurs).
Etiology:
The plantar fascia attaches to the fibula tubercles and the heads of the metatarsal bones and supports the longitudinal arch of the foot. When standing, around half of the body weight rests on the longitudinal fascia, with the greatest tissue stress occurring at the transition to the calcaneal tuberosity. Due to the constant strain, micro-injuries to the fascia can occur, which usually resolve spontaneously. However, in some cases, persistent microinjuries can lead to chronic aseptic inflammation with pain syndrome. When the plantar fascia becomes inflamed, marginal bony outgrowths known as 'heel spurs' can form as a compensatory reaction.
If you have a heel spur, an X-ray examination of the foot is recommended to clarify the type and extent of the pathological changes in the bony structures. To assess soft tissue changes in chronic heel spurs, magnetic resonance imaging of the soft tissues of the foot can be performed if this helps the attending physician to determine the treatment tactics more precisely.
Read more:- Treatment of plantar fasciitis.
- How to cure plantar fasciitis forum.
- Treatment of plantar fasciitis ointment.
- Treatment of plantar fasciitis on the sole of the foot.
- Orthopedic shoes for women with heel spurs.
- Longitudinal soleus muscle.
- Tear of the foot fascia.
- Heel spurs and Achilles spurs.
