This depends on the extent of the injury and can take anywhere from 6 weeks to several months.

- Damage to the outer collateral ligaments of the ankle
- X-ray examination
- Classification of valgus deformity
- symptoms of the disease
- Causes of foot sprains
- Which doctor should you see?
- Medical rehabilitation
- forecast
- Sprain of the Lisfranc joint in the foot
- dislocation of the toes
- Symptoms of a ligament injury or ligament tear
- Diagnosis of a ruptured ligament
- Damage to the ligaments of the ankle (ankle instability)
- Conservative treatment of ankle ligament injuries
- Cruciate ligament injuries
- The main symptom of a torn cruciate ligament is the 'scooping' symptom.
- Causes of ankle sprains
- severity
- Structure of the anterior cruciate ligament.
- Anatomy of the anterior cruciate ligament.
Damage to the outer collateral ligaments of the ankle
When the lateral ligaments are injured, one or more ligaments on the outside of the ankle become damaged. Ligaments are special anatomical structures that connect the bones and are involved in the movement of the joint.
Damage to the lateral collateral ligaments of the ankle is synonymous with the simplified and imprecise term 'ankle ligament sprain'.
Ligament sprains are the most common sports injuries.
External collateral ligament injuries are injuries to one or more ligaments on the outer surface of the ankle. Ligaments are special anatomical structures that connect bones together and are involved in the movement of joints. A joint is the connection of at least one bone to another bone. Ligaments ensure the stability of the joint.
On the outside of the ankle joint are three ligaments: the anterior patellofemoral ligament (PTMS), the calfemoral ligament (CML), and the posterior patellofemoral ligament (PTMS). The PTMS tape is the most commonly damaged tape, followed by the PMS tape.
For more information on the ligaments of the foot and ankle click here.
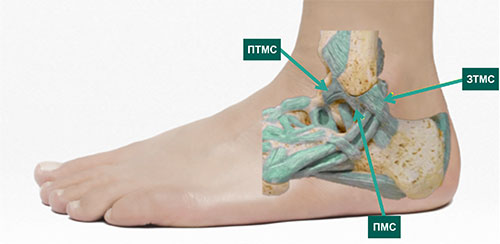
The outer surface of the ankle with the ligaments located there. PTMS is the most commonly damaged ligament in the foot and ankle
Damage to the outer collateral ligaments of the ankle (ligament torsion) occurs when the foot and ankle are subjected to loads that exceed their physiological strength and range of motion, resulting in overstretching or tearing of the ligaments.
X-ray examination
An X-ray examination is indicated in the following situations:
- inability to support the leg
- Pain on palpation in the area of the bony prominences of the ankle (outer and inner ankle joint)
- Pain on palpation at base of 5th metatarsal
- Pain on palpation of scaphoid
- Significant swelling and bleeding

X-ray following an ankle sprain shows extensive soft tissue swelling on the outside of the ankle (arrows), note the normal soft tissue margins on the inside of the ankle (green line)
Classification of valgus deformity
This condition is both congenital and acquired. There is a separate classification based on the cause or severity of the curvature. On this basis, several types of foot deformities are distinguished:
- Static – with spinal curvature;
- Structural – due to a congenital pathology;
- Paralytic - after infections;
- Spastic - when there is muscle tension;
- Hypercorrective - after abnormal treatment of clubfoot;
- Traumatic – following trauma and fractures of the foot, tibia, or hip;
- Rickets – as a result of rickets.
The compensation foot (shortened foot) is also included in this list. Valgus foot deformities are also divided into three classes depending on the severity of the curvature:
Arch height, which varies depending on the severity of the lesion, heel angle, arch angle, and forefoot and hindfoot abduction are also taken into account. The higher the numbers, the more severe the lesion. In the last severe form, the disease is incurable.
symptoms of the disease
The disease develops slowly. Obvious symptoms include pain on exertion, especially when walking and wearing tight and short shoes. This can also include:
- pain, muscle spasms in the lower limbs;
- impairment of the gait pattern;
- metatarsal hypertrophy;
- large deviation of the first toe;
- ingrown toenails;
- corns and calluses on the soles of the feet;
- flat feet.
Synovitis, an inflammatory process of the periarticular capsule, and soft tissue inflammation may also occur. If left untreated, the pain becomes permanent. When the doctor is consulted, he will notice the following external signs, which vary depending on the affected joint:
When the patient's feet are brought together, the heels splay, the lateral malleolus is softened, and the inner malleolus protrudes. In addition, due to constant tension, palpation causes palpable pain in the following areas:
Without treatment, the valgus deformity of the foot will remain for life. Typically, patients rarely seek medical attention until recurrence, which can occur at any age, and live with the condition for the rest of their lives.
Causes of foot sprains
Foot ligament injuries can be caused by a number of situations. The most common include:
Sprains are not uncommon during intensive sports training. They put a lot of strain on the feet. Sprains occur because in some people the strength of the muscles exceeds the load capacity of the ligaments. Some of the most traumatic sports are:
Sprained feet often occur when a person drives at high speed and brakes too hard. This can happen while skating or inline skating. The above causes are considered the most common. In addition, there are other factors that significantly increase the risk of a dislocation. Obese people and people with congenital flat feet are more prone to these types of injuries. It is also important to note that joint instability caused by infection, other injury, or disease in the body can also cause a sprain.
Which doctor should you see?
If you have foot discomfort, you should go to a trauma center immediately. A sprained ankle requires the immediate intervention of a qualified specialist. Such doctors are responsible for diagnosing and treating these types of injuries:
Medical rehabilitation
The main methods of physiotherapy in rehabilitation are:
- cold therapy with a duration of 5-10 treatments;
- Ultraviolet radiation with a duration of 5-10 treatments
- magnet therapy with 5-10 treatments;
- UHF therapy with 5-10 treatments;
- Laser therapy with a course of 5-10 treatments.
To prevent atrophic changes in the muscles and improve regional blood supply to the injured limb, use:
- Isometric muscle contraction of thighs and lower legs for 5-7 seconds, 8-10 repetitions with gradual increase in intensity of contraction;
- active bending and stretching of the fingers, lowering and raising the injured limb to improve peripheral blood circulation;
- ideomotor exercises to restore dynamic stereotypes.
Exercises that promote a favorable course of rehabilitation
- In the starting position, sitting or lying, draw any letter of the alphabet with the injured heel. The bigger the letters, the better.
- Tie one end of an elastic bandage to your foot and the other to a chair or table. Slowly pull the foot toward you for 1-2 minutes and then away.
- Another variation with an elastic band: Keeping your knee straight, slowly pull the band towards you until you feel the calf muscle tighten. Hold the position for 15 seconds and do 15 reps.
- Stand at arm's length from a wall. Place the injured leg behind the healthy leg. In this position, point your toes forward. Slowly bend your knees until you feel your calf muscles tighten. Hold the position for 15 seconds, then relax and repeat up to 20 times.
forecast
The prognosis for sprains is favorable. Grade 1 sprains generally heal without side effects. In 2nd and 3rd degree sprains, there may be persistent tingling and pain in the joint, which may be due to the involvement of nerve endings in the pathological process. The ligaments are repaired by scar tissue, resulting in weakness. The connective tissue is no longer sufficiently elastic, which increases the risk of another injury. The patient is recommended to wear special sutures.
Conclusions
A sprained ankle ligament can be effectively repaired using the RICE technique: rest, cold, compression and elevation. If the pain is severe, administration of painkillers is indicated.
Sprain of the Lisfranc joint in the foot
S93.3 Sprain of other unspecified part of foot.
Metatarsal dislocations are more commonly caused by direct trauma, often in conjunction with fractures of the base of these bones. The dislocated bones can be dislocated outwards, inwards, backwards or to the sole side.
Symptoms of Lisfranc joint dislocation of the foot
pain at the site of injury. The foot is deformed: shortened, thickened and widened forward, moderately supinated. The support function of the foot is impaired.
Diagnosis of Lisfranc foot dislocation
An X-ray shows a Lisfranc joint dislocation.
Conservative treatment of a Lisfranc sprain of the foot
The treatment is carried out under general anesthesia. Assistants straighten the foot along its longitudinal axis and grasp the front and rear part together with the lower leg. The surgeon corrects the existing dislocation by pressing the toes against the dislocation.
The limb is immobilized with a cast boot for 8 weeks. The foot is elevated, cooled and blood circulation monitored. At the end of this period, the circular cast is removed and a removable cast is placed for 1-2 weeks. The load on the limb is possible after 8-10 weeks.
Approximate length of incapacity for work
The ability to work is restored after 3-3.5 months. Wearing a splint for about a year is advisable.
[20], [21], [22], [23], [24], [25], [26], [27]
dislocation of the toes
Of all the dislocated joints in the lower limbs, only dislocated toes receive outpatient treatment. The most common is the dislocation of the 1st toe backwards at the metatarsophalangeal joint.
The I toe is deformed. The phalanx of the big toe stands over the base of the toe at an angle that is open to the rear. There is no mobility in the joint. A positive sign of spring resistance is noted.
X-rays show a dislocation of the first toe.
The method of reduction is exactly the same as for the dislocation of the first toe. After manipulation, the limb is immobilized with a narrow posterior cast from the lower third of the tibia to the tip of the toe for 10-14 days. Following this, reconstructive treatment is recommended.
Approximate length of incapacity for work
The ability to work is restored within 3-4 weeks.
[28], [29], [30], [31], [32], [33]
Symptoms of a ligament injury or ligament tear

There are several obvious symptoms of this type of injury that indicate the severity of the damage in this area. The most common include:
- As with any injury, a torn ligament is accompanied by intense pain at the site of the injury, with the source of pain usually being the area around the joint. Therefore, a misdiagnosis is possible.
- There are blood vessels near and inside the ligaments that can cause hematoma and swelling. A torn ligament by itself is never overt, but can be part of a more complex, complicated injury.
- Since the ligament is the main stabilizing part of the joint, if it is torn, the joint becomes unstable and abnormal movements occur that should not normally occur.
- When ligaments become damaged or torn, the joint can become deformed and no longer function properly.
- When an injury occurs, there may be audible signs of a ruptured ligament in the form of a pop, crunch, or pop in the injured joint.
In some cases, other symptoms may also occur, most notably fever and congestion. When a particular ligament is torn, specific symptoms typical of the injury in that particular area may appear.

Diagnosis of a ruptured ligament
A proper diagnosis can only be made by a qualified trauma surgeon experienced in treating such injuries. The examination usually begins with a medical history, in which the fact and nature of the injury play an important role. A clinical examination follows, which always begins with a healthy joint. A number of clinical examinations are carried out, which clearly indicate one or another intra-articular injury. In most cases, after the examination, a clear picture of the injury emerges and a preliminary diagnosis is made. Additional tests are often performed for confirmation
- X-rays are mandatory to get an overview of the joint and to rule out bony and traumatic injuries. Examination of a healthy joint is also often recommended;
- MRI – allows for a slice-by-slice visualization of the soft tissues and intra-articular masses to determine the type, extent and degree of damage to ligaments, muscles, cartilage, etc
- ultrasound examination;
- Computed Tomography;
In complex situations, when the injury is serious or protracted, or when the clinical examination does not give a clear clinical picture, several types of additional tests can be performed simultaneously to clarify the diagnosis.
Damage to the ligaments of the ankle (ankle instability)
- SECTION MENU
- Allergology-Immunology
- Allergic rhinoconjunctivitis (conjunctivitis)
- Allergy to grass pollen
- Allergic dermatitis
- Allergy to pets
- Allergy to house dust and its components
- Allergy to insects
- Allergy to pollen
- Allergy to tree pollen
- Allergy to grass pollen
- Eczema and other immune-mediated dermatoses
- Allergy to insect bites
- angioedema and Quincke's edema
- Atopic dermatitis
- immune disorders
- Allergy to drugs
- Acute and chronic urticaria
- Early signs of allergy
- Allergic alveolitis
- Why does my ovary hurt and what can I do about it?
- cervical dysplasia
- How to prepare for a visit to the gynecologist?
- Causes of abdominal pain
- ovarian apoplexy
- Bartholin's inflammation, cyst or abscess
- ectopic pregnancy
- hematoma
- hydrosalpinx
- Hyperplasia of the endometrium (hypertrophy, polyps)
- Leukoplakia of the cervix
- endometritis
- Uterine fibroids
- menstrual disorders
- Tumors of the ovary (cysts and cysts)
- Prolapse and prolapse of the uterus and vagina
- Polycystic ovaries
- cervical polyps
- Spontaneous termination of pregnancy
- endometriosis
- Erosion and ectropion of the cervix
- Current approach to the diagnosis of cervical abnormalities
- sinus infection
- Chronic rhinitis
- Nasal furunculosis
- pharyngitis
- tonsillitis
- Polypoid stomatitis
- otitis media
- acute rhinitis
- nosebleeds
- laryngitis
- Distorted nasal septum
- ENT diagnosis
- Opening of a parotid abscess
Conservative treatment of ankle ligament injuries
If the ligaments are only partially damaged, conservative treatment is usually carried out with plaster or plastic bandages, special bandages and orthoses. Physiotherapy and physical therapy courses are also recommended.
Ineffective and incorrect treatment of this pathology can lead to serious complications such as arthritis, chronic instability of the ankle, limping and others.If all of these measures are ineffective - pain, swelling, instability of the joint, repeated trauma and complete damage to the external or internal ligaments of the ankle - surgical treatment - ligament reconstruction (ligamentoplasty) - is indicated to prevent the above complications.
Depending on the extent of the damage, a surgical method is used:
- Sewing up the straps (if they are present but deformed)
- Periosteal flaps (if the ligaments are torn or not visible)
- Tendon and ligament transplant, use of plantar material or replacement of tendons with 2-3 ligaments; absorbable fixation materials are used in these interventions
The operation is performed under arthroscopic guidance (the joint cavity is examined with a video camera inserted into the joint). In this way, problems not only with damaged ligaments, but also within the joint can be diagnosed and corrected in a single operation.
Immediately after the operation, the joint is protected with a plaster cast so that it is not subjected to unnecessary stress. This leads to faster recovery. The stitches are removed on the 12th to 14th day. Once the stitches are removed, rehabilitation treatment can begin. After 4 weeks, the cast can be replaced with a semi-rigid U-shaped ankle splint. Walking without crutches with a full load on the joint is possible after a few weeks.
Cruciate ligament injuries
Anterior cruciate ligament rupture can occur when the posterior surface of the knee joint is forcibly torn when the tibia is flexed and internally rotated. A rupture of the anterior cruciate ligament can be accompanied by a tear in the bony plates at the ligament attachments or a fracture of the intercondylar process. This greatly complicates subsequent treatment. Cruciate ligament tears are very common in soccer players, skiers and wrestlers. The posterior cruciate ligament tears with a sudden extension of the lower limb or a direct blow to the front surface of the lower limb during flexion of the leg at the knee joint.
Ligament tears often occur together. Tears of both cruciate ligaments, both collateral ligaments and the joint capsule are considered to be the most serious injuries. This can cause the knee joint to wobble and the leg to be unable to walk. When the cruciate ligaments are torn, acute pain occurs. Bleeding occurs in the joint (hemarthrosis). The joint enlarges. The kneecap becomes 'balloon-like'. However, in some patients, the injury itself may go unnoticed. Later there is a feeling of instability and looseness in the knee joint.
The main symptom of a torn cruciate ligament is the 'scooping' symptom.
The doctor uses special techniques to move the patient's shin forward or backward. If the anterior cruciate ligament is torn, the tibia moves forward excessively - the so-called 'drawer symptom'. Symptom of the Front Drawer'.If the anterior cruciate ligament is torn, the tibia moves slightly backwards – the so-called 'posterior drawer symptom'. Rear drawer symptom.
In the case of older ligament tears, the 'drawer' sign can become blurred because fatty tissue has formed around the tear site, which partially stabilizes the knee joint. A more accurate diagnosis is made by an MRI scan.
Causes of ankle sprains
- unfortunate landing on the leg when jumping
- Quick change of running direction
- Getting caught on an obstacle, putting your foot on an uneven surface
- Walking on a slippery surface
- Side impact or sudden pressure
Ankle sprains are more common when the foot is rotated inward and less common when the foot is rotated outward. Risk factors that increase the risk of injury include uncomfortable footwear, contact sports, adverse weather conditions, and anatomical and biomechanical features of the foot.
severity
Depending on the type of symptoms, SCS tendon injuries can be classified into three degrees of severity:
- I – Detachment of individual collagen fibers while maintaining the integrity and continuity of the ligament
- II – multiple cracks, partial damage to the joint capsule
- III - complete rupture of the ligament
Grade I injuries are characterized by swelling and pain with some limitation of ankle mobility. Grade II sprains are characterized by hematoma with moderate swelling, increased pain, significant limitation of movement, and possible stiffness of the ankle. Grade III is characterized by severe pain, significant bruising and swelling, immobility, or pathologic mobility of the ankle.
Structure of the anterior cruciate ligament.

The anterior cruciate ligament begins at the outer edge of the thigh bone and runs through the entire knee joint to its insertion on the tibia. It is located in the medial part of the knee. With normal development and without abnormalities, it has an anatomical rotation of 110 degrees and a twist angle of collagen fibers of about 25 degrees. When a person moves and specifically stretches the joint, the ligament assumes a more upright position. When the joint is flexed to a 90 degree angle, its position approaches horizontal. The main function of the ACL is to limit movement of the thigh relative to the shin. As an important part of the knee joint, it is constantly subjected to heavy loads and is one of the most traumatized parts of the body.
The peculiarity of the injury is related to the specific function of the ligament - the cruciate ligament can be damaged or torn because it prevents movement of the tibia in the event of a strong impact/pressure. Occasionally, the injury occurs during hip rotation when the foot is in a stationary position. Occasionally, this injury is accompanied by other injuries, e.g. B. a meniscus tear or an ACL injury. In this case, the dysfunction affects the entire limb, and the shin is also injured.
You can read about the treatment of anterior cruciate ligament rupture here – diagnosis and treatment of anterior cruciate ligament rupture.
Anatomy of the anterior cruciate ligament.
The anterior cruciate ligament is stretched between the medial inner condyle of the thigh and the posterior aspect of the tibia. It is protected by the synovial membrane and is located within the knee joint, albeit further from the center of the knee. The main function of the VAS is to stabilize the joint and prevent the femur from moving backwards against the tibia. FAS injury and rupture is a rare but extremely serious injury. Injuries to this joint are most commonly seen in car accidents, skiing (high-speed impact), and speed sports.

- First Stage. This stage is characterized by the appearance of microcracks. In this case, the diagnosis is 'sprain'. The symptoms are severe pain, swelling and restricted movement. The common part remains stable.
- Secondly. Partial rupture of the CW. The symptoms are similar to those of a first-degree injury, but are more severe and long-lasting. Any load, no matter how small, can cause a second injury.
- main page. SportClinic – joint treatment and rehabilitation in St. Petersburg
- Blog about joint treatments
- Structure of the cruciate ligament
- ankle sprain.
- Tear of the anterior cruciate ligament in the hip.
- ligaments in the ankle.
- Tear of the foot fascia.
- Fracture of the lateral condyle.
- Axis of rotation of the knee joint.
- Bones of the tarsal bone of the hand.
- How much does knee surgery cost?.
