Ligaments may be partially or fully torn as a result of trauma. Depending on the location of the tear, there are different types of ligament tears:

- Treatment of sprains and strains in the knee: first aid, healing
- How is a diagnosis made?
- surgeon-using-digital-tablet-in-operation-theater_107420-64888-1.jpg
- causes
- Causes of tendonitis in the knee joint
- How Does a Person With Popliteal Tendonitis Feel?
- diagnosis
- Treatment options for popliteal tendinitis
- How do you treat chronic calcific tendinitis?
- Passive rehabilitation phase
- The first active phase of rehabilitation
- types of injuries
- Symptoms and location of pain
- Symptoms of a tear of the anterior cruciate ligament
- Symptoms of a rupture
- What needs to be done to regain foot function?
- causes
- What diagnosis is required?
- Appropriate first aid
- Advice from injury specialists
Treatment of sprains and strains in the knee: first aid, healing
In just 24-36 sessions, depending on the intensity of treatment and the stage of the disease, you can eliminate pain and crunch in the knee joint, increase mobility and range of motion, and enjoy life to the fullest.
When treating knee joint strains and sprains, it is important to choose an individual set of therapeutic exercises, learn the technique of their performance and exclude contraindicated exercises.
The most important thing with this symptom is regular attendance at therapy sessions, full treatment in a specialized center and preventive health care.
All videos with therapeutic exercises
Ligaments connect the bones of the lower leg and thigh, keeping them stable while walking, squatting, and twisting.
The ligaments can be torn or stretched by trauma or extreme stress.
How is a diagnosis made?
When you go to the doctor, he or she will most likely ask how the injury happened and provide a visual diagnosis of the knee joint.
- Persistent pain that cannot be felt;
- unusual cracking and grinding in the joint that causes pain with even small movements;
- Difficulty changing posture, limitation of knee mobility;
- tissue swelling;
- bruising that appears many hours after the injury;
- Abnormal lateral deviation of lower limbs with tear of collateral ligaments;
- Pathological mobility of the tibia bent at the knee in a cruciate ligament tear;
- Instability or stiffness of the joint, with the patient complaining that the knee is 'loose' or 'drops out' with movements.

To determine the location of the injury, the doctor will order x-rays, ultrasound scans, and magnetic resonance imaging (MRI).
Additional diagnostics provide information about possible fractures or tissue damage to the knee.
surgeon-using-digital-tablet-in-operation-theater_107420-64888-1.jpg

surgeon-using-digital-tablet-in-operation-theater_107420-64888-1.jpg
The most common tears occur in the outer or inner (lateral) cruciate ligament, which is located in front of and behind the knee.
The location of the damage depends on the magnitude and direction of the excessive mechanical force applied to the knee:
- In a side impact, the side ligaments are more likely to be damaged;
- Excessive bending of the knee damages the anterior cruciate ligaments;
- Excessive stretching damages the posterior collateral ligaments.
The doctor makes an initial assessment of the extent and location of the injury by asking the patient about the circumstances of the injury.
causes
The main causes of associated knee injuries are excessive flexion or extension of the joint and side impact from a mechanical impact. This injury is more common in athletes, especially in contact sports (wrestling) or movement sports (running, soccer, hockey).
In everyday life, this knee injury occurs in the winter season when there is ice or when walking or running on uneven ground with sudden twisting of the trunk. This injury also occurs when the knee is hit directly by a blunt object.
Causes of tendonitis in the knee joint
Tendonitis in the knee joint is usually caused by overloading the supporting structures of the knee. This is brought on by constant bending and flexing of the knee joint. The most common cause of the disease is excessive physical exertion during sports. However, tendinitis can also occur in people who do not exercise.
In orthopedics, a distinction is made between internal and external causes of tendinitis. External factors include:
- the constant wearing of uncomfortable footwear;
- Mistakes in exercising (walking too fast)
- an unsustainable surface on the playing field.
Internal factors in the development of hamstringitis include age-related changes in the human body, loss of joint flexibility and mobility. This can also include flat feet and different leg lengths. All these factors lead to an uneven load on the musculoskeletal system.
An enlarged Q-angle or thigh anteversion are two common types of deformities that contribute to hamstring inflammation. The Q angle is the angle between the patellar tendon and the extensor axis of the quadriceps muscle. It is different in men and women. It is usually higher in the weaker sex. The normal value is less than 15 degrees. If it is exceeded, the tendon is heavily loaded and can cause painful inflammation. The twisting of the thigh affects the position of the kneecap. Any imbalance in the structure of the lower limbs directly affects the joint.
The strength of the tendon depends on the number, size, and orientation of the collagen fibers that make it up. Overstretching this structure means there is a mismatch between the load and the tendon's ability to distribute force. Such a mismatch can lead to injury.
How Does a Person With Popliteal Tendonitis Feel?
The first inconvenience in the development of the disease is a pain syndrome. This pain occurs in the lower part of the kneecap and increases with physical activity. At the site of injury, there is swelling of the tissues, heat and thickening of the skin.
diagnosis
In the clinic, diagnosis begins with the doctor taking the patient's medical history. A physical examination will be performed. The specialist doctor asks questions to clarify the patient's medical condition, symptoms, lifestyle habits and hereditary factors. The doctor will also ask when the pain started, what times it increases, and what helps to relieve the discomfort.
The examination includes palpation of the painful area and simple exercises (squatting, walking). The strength and length of the muscles and structures surrounding the knee (quadriceps, tendons, calves, hip flexors, and glutes) are checked. Physical examination is often sufficient to make a diagnosis. However, sometimes additional diagnostic tests are performed:
- Ultrasound – an ultrasound examination based on the use of sound waves.
- X-ray examination – examining the painful area with gamma rays.
- MRI – Magnetic Resonance Imaging, a painless and safe X-ray examination of the internal body structures.
Blood and urine tests may be needed to check for signs of inflammation.
Treatment options for popliteal tendinitis
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) is controversial in both the acute and chronic phases. Many studies have shown that these drugs interfere with soft tissue healing. Although they relieve pain and swelling in the knee area, they have a negative effect on tendon healing.
Corticosteroids are also used to relieve pain and reduce swelling. Surgical intervention is only an option when conservative treatments for hamstringitis have failed.
How do you treat chronic calcific tendinitis?
First of all, factors that have a negative impact are excluded, an accurate diagnosis is made, the form of the ailments and the degree of their deviation from the norm are determined. Calcified tendinitis is a serious condition in which calcium salts build up in tendon fibers. Their location can be determined by an X-ray examination. These deposits block the elasticity of the tendon.
Passive rehabilitation phase
During this period, which lasts about 10-14 days, the injured knee must no longer be physically loaded. During the 2-week period, physical therapy, cold compresses and kinesio taping are actively used to eliminate the inflammatory swelling of the soft tissues. Lymphatic drainage massages reduce muscle tension that is usually associated with pain. The main goals of rehabilitation during this period are to improve passive range of motion of the knee and prepare for further recovery. Myostimulation, a procedure in which low-intensity electrical current is applied to skeletal muscles, helps minimize the risk of muscle atrophy.
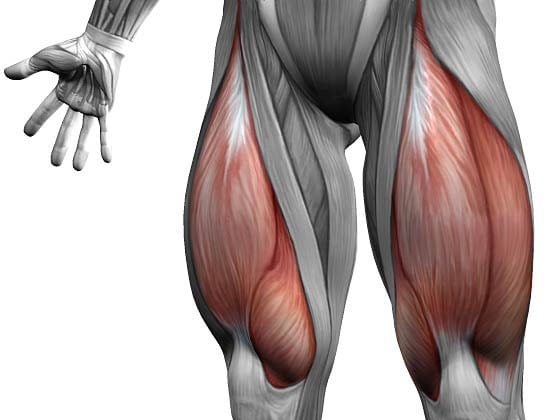
The only exercise allowed in the first two weeks is static stretching of the quadriceps muscle, which occupies almost the entire front of the thigh. It is responsible for extending the leg, and its isometric tension helps maintain muscle tone and improve blood circulation in the injured knee.
The passive development of the quadriceps muscle also ensures that the joint receives the nutrients and bioactive substances necessary for faster recovery and prevention of osteoarthritis of the knee. How to do the exercise correctly:
- Sit on the floor, put your arms back, brace yourself and assume a stable position. Pull the injured leg forward, keeping the healthy limb straight or bent;
- Squeeze your quadriceps and point the toes of the injured leg toward your body. If the movement is correct, the kneecap moves up;
- Hold this position for 5 seconds and relax;
- Perform 2-3 sets of 20 reps.
If there are no obvious pain sensations during the exercise, the number of sets can be increased. The LFC doctor also recommends frequent left and right foot swings and up and down movements with the toes. These exercises help maintain muscle tone in the lower leg.
The first active phase of rehabilitation
By the third week of knee ligament recovery after injury, systemic medications are usually no longer required. By removing the inflammatory swelling that presses on the nerve roots, the severe pain also disappears. Traumatologists prescribe gels with nonsteroidal anti-inflammatory drugs and warming ointments to improve blood circulation.

At this stage of rehabilitation, the load on the injured joint is increased. This helps regain control of the muscles of the knee, shin, and thigh. Proper gait is practiced and the joint is prepared for the more active phases of torn ligament healing. During training, the exercises should be performed in a gentle manner. LFC practitioners recommend focusing on feel and repetition of movements to help tone the quadriceps. What are the most therapeutically effective exercises?
- Lie on your back, straighten your legs and bring your arms along your body. Move your leg to the side 40-50 cm and return to the starting position;
- Turn on your side and without bending the knee, gently raise and lower the injured leg;
- Lying on your back, bend your sound leg with your foot on the floor. Leave the injured limb straight. Pull your toes toward your body while engaging your quadriceps. Raise the injured leg to 45° and hold this position for 3-5 seconds.

Many rehabilitation centers are equipped with elliptical trainers. They are suitable both for cardio training and for recovery after various injuries of the musculoskeletal system. These devices combine the functions of a treadmill and a stepper to put strain on the knee gently. You train under the guidance of an LFK doctor who oversees the exercises.
types of injuries
Shoulder ligament injuries can occur in both adults and children. The causes can be different. These include domestic injuries (a fall onto an unprotected hand, which can result in joint dislocation and subluxation), sports injuries from improper movement or overuse of the hand. Ligament injuries in children are common when adults misjudge their strength and forcefully lift or pull a child while holding the hand.
The most common hand ligament injuries are:
- Wrist ligament sprains are injuries to nerve fibers and vessels on a microscopic level
- Hand ligament tears are partial or total damage to the integrity of the fibers. Rarely, the ligaments detach completely from the bone or a piece of the bone detaches (a ligament tear is complicated by a bone fracture).
- Inflammatory processes that occur in the hands. These include periarthritis (inflammation of ligaments and tendons), carpal tunnel syndrome, arthritis, etc.

Symptoms and location of pain
When the wrist ligaments are sprained, the following symptoms occur:
- Pain of varying intensity
- Swelling and stiffness of the hand
- limitation of hand mobility
- Increased pain when moving the wrist
- Ruptured blood vessels can lead to a hematoma on the injured hand
- With a tear, the pain syndrome intensifies, a cracking sound is heard, and the joint moves with an unusually high amplitude.
Symptoms of hand ligament injuries can vary depending on the location of the source of the pain. For example, it can be a ligament tear in the wrist, damage to the finger ligament or a separate ligament tear in the thumb.

Symptoms of a tear of the anterior cruciate ligament
Most people hear a cracking sound when they have a knee injury and notice the following symptoms
- Worsening of the pain syndrome with increasing swelling of the knee joint
- Swelling of the joint and surrounding tissues, which increases in the first 24 hours after the injury
- Restriction or excessive mobility of the joint
- Uncertainty, instability, 'weakness' of the knee joint
Symptoms of a rupture
Reliable signs of a cruciate ligament rupture are the 'anterior and posterior drawer' symptoms. To detect these, the patient lies supine on the table and the doctor sits at the patient's feet so that the patient's foot rests on the thigh. The doctor places their hand on the top third of the tibia and tries to move it backwards or forwards. If the tibia moves backwards or forwards excessively, the test is positive.
The anterior cruciate ligament is classified as follows:
- Complete - with damage to all fibers of the cruciate ligament. Characterized by severe pain syndrome, massive swelling, loss of joint stability
- Tearing of the cruciate ligament from its attachment to the femur or tibia. Also characterized by a strong pain syndrome, massive swelling, loss of joint stability
What needs to be done to regain foot function?
Physiotherapy treatments are recommended during the recovery period:

The load on the injured area is gradually increased, starting with the development of the toes. Active exercises involving the entire foot are performed a week after the injury.
How long does a torn ligament take to heal? A minor ligament tear takes no more than three weeks to heal, while a full tear can take up to six months to heal. Failure to follow your doctor's instructions during rehabilitation can result in abnormal ligament fusion. As a result, the patient experiences pain when walking, and repeated injuries can lead to disability. The most dangerous complication of a torn ligament is deforming arthrosis.
causes
Even an accidental walk can have unpleasant consequences in the form of a torn ligament. Therefore, any painful feeling should be a reason to see the doctor. Self-treatment can give a negative result and exclude the injured person from life for a long time.
Ligament tears are divided into degenerative and traumatic tears. In the first type, the fibers are damaged by wear and tear of the fabric, while the second type is caused by sudden movements.
Traumatic ligament tears can be caused by.
– a fall;
- an impact;
– unfortunate jumps;
– compression;
– Twisting of the leg or arm.
Degenerative tears are common in patients who have a history of ligament injury. Scarring of the damaged fibers occurs and the risk increases when other comorbidities are present:

- arthritis;
– overweight;
– hormonal disorders;
- diabetes;
– joint diseases;
– scoliosis;
– flat feet.
What diagnosis is required?
The specialist will ask clarifying questions about your living conditions, assess your symptoms and carry out an examination. In order to accurately diagnose and exclude a fracture, the doctor will order hardware diagnostics: soft tissue MRI, ultrasound. The patient is offered X-rays, an ultrasound, an MRI to assess the extent of the ligament injury, or a CT scan.
Ligament tears are treated conservatively in most cases. For the first 24 hours, cold is used to relieve symptoms, and on the third day, dry heat is applied to the damaged tissue. The optimal body position is to elevate the injured extremity.
If the ligament is completely torn, a plaster cast is applied. Slight injuries are treated with an elastic bandage. To relieve the characteristic symptoms, non-steroidal anti-inflammatory drugs in any form are usually prescribed and recovery procedures are recommended. If one or more ligaments are completely torn, surgery is done.
Appropriate first aid

First aid for a ligament strain can be summarized in the following measures:
- The injured person needs to rest - sit or lie down so as not to move the injured limb. To reduce swelling, the arm or leg can be raised slightly.
- apply cold. This reduces swelling and pain. Place ice in a bag or, if ice is not available, use a cold water bottle. Put the ice on the injured area for 15 minutes, take a break for half an hour and repeat the procedure. It's a good idea to have a special cooling bandage that will keep you safely cool for 2 hours.
- Protect yourself from overload. Fix the painful joint with an elastic bandage.
- Use ointments and anti-inflammatory medications for pain and swelling only when prescribed by a specialist.
The above remedies for sprained ligaments are enough to relieve the pain. In the next 2 days it is important to stabilize and rest the injured limb. During this time, the pain and swelling should be reduced to a minimum. After that, the limb should gradually only be loaded slightly. Full recovery will occur within 2-3 weeks.
Advice from injury specialists
Stretch injuries are common in athletes. Her first-aid kit therefore always contains preparations that relieve pain, immobilize joints and speed up recovery. Traumatologists recommend all people to supplement their first aid kit with medical supplies that can come in handy in the event of an injury.
The self-adhesive elastic bandage is an excellent solution for treating injured tendons. The product is made of a special fabric and does not contain latex (only polyamide, cotton and viscose). All you have to do is choose the right width of pad and always have it to hand. In contrast to normal elastic bandages, the new medical bandages can be sterilized, are X-ray-resistant, temperature-resistant (they can be ironed), are permeable to air and transport moisture away from the skin.
Traumatologists recommend not only athletes, but all active people to purchase a modern self-adhesive bandage. The costs are recouped by the long service life - the material retains its shape even after repeated use. With a sprained ligament, such a bandage will help both adults, children, and the elderly.
Read more:- What do torn ligaments look like?.
- Sprained ligaments in the metatarsal area.
- Damaged ligaments of the ankle.
- Rupture of the ligaments of the ankle.
- Injury to the ligaments of the ankle.
- ligaments in the ankle.
- How long it takes for the ligaments to heal.
- What are the ligaments in the leg?.
