Ischemic compression of the tarsal contents alters the blood supply to the foot and causes weakness of the short flexor thumb. Chronic compression resulting from disruption of the same innervation contributes to hammertoe (cat's head) deformity. It is also noted that this pathology accompanies almost all cases of valgus foot deformity.

- pain in the ankle
- Causes of ankle pain and associated symptoms
- causes of injury
- Severity of ligament injury
- Osteochondral injuries of the calcaneus (OPBTC)
- diagnosis
- Pathogenesis of tarsal tunnel syndrome
- Classification and stages of development of tarsal canal syndrome
- Stenosal ligamentitis
- contraindications
- rehabilitation
- complications
- Subtalar ligaments
- Muscle chains and running
- Types of taping for torn ankle ligaments
- Taping of the ankle joint for torn ligaments
pain in the ankle
The development of pain in the ankle joint has many different causes, which depend on age, lifestyle and accompanying pathology. However, in the absence of trauma, the development of ankle pain can indicate a number of pathologies - gout, bunions, arthritis and many other problems. The most obvious causes of ankle pain are acute injuries (sprains, twists, fractures) caused by falls, traffic accidents or an active sport and lifestyle.
Ankle pain itself varies greatly: it can be stabbing or burning, aching or throbbing, it can come on gradually or suddenly and violently. It is very important for the doctor to diagnose the cause of ankle pain and select the appropriate treatment. Based on the type of pain and the accompanying complaints, symptoms and manifestations, the main causes of the joint problems can be identified and the treatment tactics, the scope of the necessary diagnostic measures and the subsequent rehabilitation can be determined. Sometimes treatment only requires rest and protection, but in some cases surgery may be the only salvation.

Causes of ankle pain and associated symptoms
The ankle joint is a very complex structure. It consists of bones, cartilaginous structures and soft tissues (ligaments and tendons). Any injury or disease that affects the bones, articular surfaces or ligaments can cause ankle pain. The patient is not always able to associate the pain syndrome with previous events, injuries or illnesses, so the cause of the problem must be determined. The most common causes of ankle pain include:
Ligament sprains – damage to one or more ligaments as a result of various traumas (fall, walking on uneven surfaces, sports). A quick twist or twist of the ankle inward can damage the ligaments. Most commonly, the anterior ligament (talar-malofemoral ligament) is damaged, resulting in severe, throbbing pain on the outside of the ankle. There may also be bruising, swelling or instability of the joint. The medial ligaments are less commonly affected - the symptoms occur on the inside of the ankle.
Tendinitis is irritation and inflammation of the tendons that connect muscle to bone. Hamstring tendonitis is most often caused by damage to the tendon that connects the thigh muscle to the bone on the outside of the ankle. It often occurs after exercise or when walking on slippery, uneven surfaces. With this type of injury, the ankle feels painful, and the feeling is bothersome, dull, lasts for several weeks, and increases with walking and standing. There may be swelling and a cracking sensation in the outer part of the ankle. Possible posterior tibial tendonitis, which is characterized by pain and swelling on the inside of the joint, with severe limitation of movement without treatment.
Osteoarthritis – age-related changes in the joint caused by the gradual destruction of cartilage and rubbing of bones against each other. Damage to the Achilles tendon, which connects the lower leg muscles to the heel bone, causes a burning pain in the back of the ankle with tissue swelling and stiffness in the heel and calf. Such problems can occur with exercise, wearing ill-fitting footwear, and in the presence of a bony heel spur. Osteoarthritis often causes ankle pain when walking and at rest. At this point, three types of osteoarthritis are possible. Over time, osteophytes (bony outgrowths) form, making movement difficult and causing discomfort. The symptoms are initially annoying and only occur sporadically, then gradually become constant and acute.
causes of injury
First, let's consider the mechanism of injury to the internal collateral ligament. As already mentioned, it is injured quite often. The situation in which it occurs is an impact just below the knee on the outside of the shinbone. The leg is usually in an upright position and is more likely to be injured (more common in soccer players). Otherwise, falls can occur in which the shinbone is blocked and the body moves sideways with a twisting movement of the leg (injuries to skiers and snowboarders). In contrast, for an external collateral ligament rupture, the impact must involve the inside of the tibia and there must be excessive knee extension or inward rotation of the body on the supporting leg.
When the ankle ligament is torn, patients complain of pain in the ankle when walking.
Examination reveals swelling and hematomas, and the injured area is very sensitive to touch.
Orthopedic surgeon Eduard V. Zhezhera comments:
In the event of a sprain, the injured person can lean on their foot. In a more serious injury, when the ligaments are torn, movement is difficult and painful, the entire foot swells, and great effort is required just to support the foot.
An ankle ligament injury usually occurs when a person makes an unnatural movement, such as walking. B. a strong twist or turn of the leg. The more violent the movement, the more likely it is that the ligaments will become damaged or tear. In such an unfortunate moment, the affected person loses their balance, falls and can only stay on their feet with pain. Sometimes a crunching noise can even be heard during this time.
Severity of ligament injury
Different degrees of injury present with different clinical presentations and require different treatment strategies. A distinction is made between:
- 1 degree– The first degree involves a partial tear of the superficial fibers. Pain will occur at the site of the deformity and swelling may occur.
- Second– Damage to most of the ligament fibers. The pain is more diffuse, the swelling of the joint increases rapidly, may be accompanied by hemarthrosis, and a hematoma may form on the lateral surface of the joint.
- Third – Complete rupture. In addition to the above symptoms, dysfunction and instability of the joint occur.







Osteochondral injuries of the calcaneus (OPBTC)
Osteochondral talar block injury (TKO) is a common cause of chronic ankle pain, particularly in younger patients (under 40 years of age).
These injuries are often not limited to the hyaline articular cartilage, but also affect the subchondral bone in the weight-bearing portion of the talar block. If left untreated, there is a risk of rapid development of osteoarthritis (cirroses).
The symptoms of TKA are often non-specific, with the most common complaint being diffuse ankle pain that occurs with exertion. Less common are swelling of the ankle joint, restricted movement, mechanical symptoms such as cracking, locking of the joint or a feeling of instability.
It is believed that most urinary tract infections result from trauma to the ankle joint. This is due to the peculiarities of the blood supply to the ankle joint and its lower ability to regenerate due to the significant mechanical load on the hindfoot.
The most common nontraumatic theories are vascular and endocrine disorders, soft tissue impingement of the inferior interosseous ligament, and chronic ankle instability.
diagnosis
Examination and radiographs of the ankle joint are not sufficient to make a diagnosis because more than 40 % of OPBTK are not detectable on radiographs.
Therefore, magnetic resonance imaging (MRI) is often part of the diagnostic minimum to identify the lesion and its location, estimate the approximate size and sharpness of the underlying processes by visualizing the swelling of the adjacent bone tissue. MRI also makes it possible to assess the condition of the ankle ligaments. It should be noted that MRI data tends to exaggerate the size of the fibula due to signal variability.
For this reason, to accurately determine the extent of the lesion and select treatment, computed tomography (CT) data is used, which clearly visualizes the bony structures.
Pathogenesis of tarsal tunnel syndrome
To understand how nerve damage occurs and what processes contribute to it, we need to look at the normal The structure of the peripheral nerve. It resembles a cable consisting of nerve bundles of different diameters surrounded by a connective tissue sheath called the epineurium. This connective tissue is a loose, fatty covering that is reinforced with longitudinal and transverse collagen fibers. In the muscle beds, the epineurium acts as a shock absorber - it alleviates the stress. The actual nerve sheath consists of the perineurium, a multilayered, circular tissue composed of flattened cells covered on both sides by a basement membrane. [12]
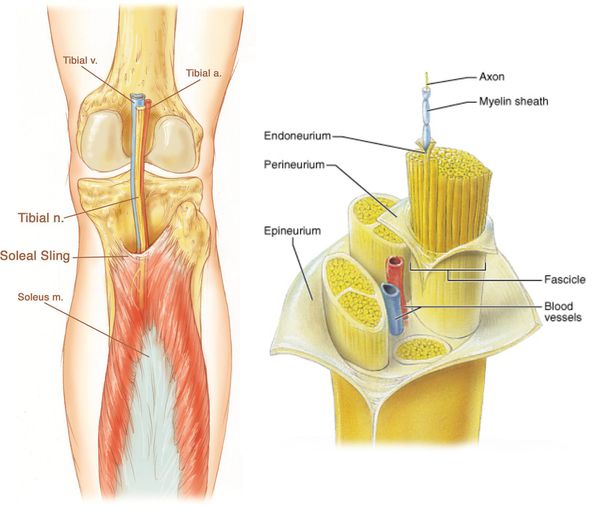
One of the branches of the peripheral nervous system is, among others Tibial nerve. It begins in the lumbosacral plexus of the dorsal roots, runs medially to the popliteal fossa laterally (as if to the side) and superficially to the popliteal vessels. [4] The nerve then passes down between the two heads of the calf muscle, enters under the tendon arch of the cambioid muscle, and then passes between this and the deep muscle down to the medial malleolus of the tibia.
At the level of the ankle joint, the tibial nerve passes through a rigid bone tunnel - the Tarsal canal. [1] This space is bounded anteriorly by the tibia and externally by the posterior talar and calcaneal processes and the flexor tendon capital.
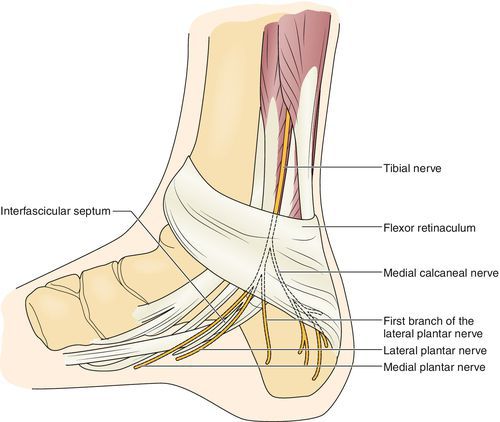
Anatomically, there are several tendon muscles in this canal: the tibialis posterior, the toe flexor, and the long toe flexor. [8] [9] In addition, the short and long toe flexors are the main muscles that are innervated after the nerve exits the tarsal canal.
Classification and stages of development of tarsal canal syndrome
There is no specific classification for this syndrome. It is a form of compression neuropathy of the lower limbs. In addition, the following forms are distinguished:
- Bernhardt-Roth paresthetic geralgia is a compression of the cutaneous nerve on the outside of the thigh, which arises from L2-L3 and runs under the vaginal ligament, where it is compressed. Clinically, it presents with paresthesia followed by pain on the anterolateral surface of the thigh.
- In Morton metatarsalgia, there is compression of the plantarfemoral nerves in the IV area. Pain and paresthesia around the heads of the III-IV metatarsals.
- Entrapment syndrome of the plantarfemoral nerve in the popliteal area and under the long humerus muscle. The peroneal nerve arises from the L4-L5 system. The entrapment occurs at the junction of the ankle nerve under the tendon of the biceps femoris muscle. It is manifested by weakness of the foot flexors, pain and paresthesia in the front of the lower leg.
Stenosal ligamentitis
There are the following types of ligament inflammation
- Inflammation of the toe ring (Nott's disease, clubfoot);
- Inflammation of the palmar and transverse ligaments of the wrist (carpal tunnel syndrome).
In carpal tunnel ligament inflammation of the hand, one of the fingers of the hand (often the thumb or index finger) makes a clicking sound when flexed and then locks into the flexed position. Inflammation of the ligament is usually accompanied by inflammation of the tendon of one of the finger flexors. The disease is accompanied by pain in the affected area and eventually spreads to the entire hand. The interphalangeal joints are often affected.

Stenotic inflammation of the palmar and transverse ligaments leads to swelling and thickening of the fibers. This leads to compression of the median nerve under the transverse ligament and thus to carpal tunnel syndrome. This disease is accompanied by severe pain and numbness in the fingers. Most people who suffer from carpal tunnel syndrome are women and people in certain jobs that place particular strain on the fingers and hands during work.
contraindications
Although MRI is a safe and informative method, not everyone can undergo an MRI of the ankle. The scanner's strong magnetic field interacts with metal objects and can interfere with embedded medical devices. Therefore, people with heart valves, cardiostimulators, neurostimulators and cochlear implants should not have an MRI scan. People with insulin pumps for medication dosing also cannot undergo an MRI scan. The decision as to whether such patients can undergo an MRI scan depends on whether the implant data sheet indicates that the product is MRI compatible.
Restricted patients include those who have a non-removable metal object in their body - shrapnel, bullets, staples, needles, metal plates and blood vessel clips. The strong magnetic field can heat or loosen the metal, causing burns or internal bleeding.
MRI scans are safe for pregnant women and children, but expectant mothers are not advised to have MRI scans in the first three months of pregnancy without a doctor's referral.
rehabilitation
THERAPEUTIC EXERCISES. After ankle arthrodesis, therapeutic exercises should be performed from the first day to prevent muscle wasting, blood clots and pulmonary embolism. This includes breathing exercises, isometric exercises to maintain and strengthen the lower and thigh muscles. In gymnastics, the load is increased gradually.
Pharmacological treatment. It includes highly effective treatment against infectious pathogens, the use of symptomatic drugs and the use of drugs against thromboembolic complications.
From the second day the patient is able to stand up. Walking is only permitted with crutches and the operated limb must not be put under any weight. After the first signs of ankylosis appear (after about 6 weeks), light axial loading of the affected leg is permissible. The patient will be able to walk normally again after 4-6 months at the earliest. Removal of metal structures usually after 10-12 months. Internal fixators do not always need to be removed.
complications
The complication rate after standard open surgery is higher than after arthroscopic procedures. Here are some comparative data on the adverse effects of the two types of surgery (without external fixators) noted in the first 3 weeks.
- Phlebothrombosis is detected in 22 % of cases after open arthrodesis of the ankle joint, in 1.8 % after minimally invasive surgery;
- About 12 % of patients develop a wound infection, while this risk is practically zero after arthroscopy (
- necrosis of the surrounding tissue in 17 % and 0.2 %;
- Wound hematomas and hematomas: 22 % i 0.9 %.
Intraoperative blood loss after a standard arthrodesis is 150-200 ml, after arthroscopic bleeding about 120 ml. Failed ankylosis after 6 months is found in 5-6 % of patients who underwent the conventional variant and in 0.5- 0.9 % of patients who underwent arthroscopy with intramedullary fixation. After any type of artificial ankylosis, there is an increased risk of osteoarthritis in the remaining joints of the limb and a reduction in leg length of up to 3 cm.
Subtalar ligaments
The talus and heel bones are connected to each other by short but strong ligaments as they are exposed to high loads when walking, running and jumping.
The most important bond is this The most important ligament is the interosseous trochanteric ligament (interosseous trochanteric ligament) (Figure 19, frontal and external view), which consists of two fibrous bands. These dense quadrangular bands lie in the tarsal sinus, a relatively large space between the lower outer surface of the calcaneal neck and the top of the front half of the calcaneus.
- Anterior thrust 1 This has an attachment to the notch of the heel bone, which forms the floor of the tarsal sinus, immediately above the spinous process. Its dense, shiny fibers run obliquely upward, forward, and outward, attaching to the calcaneal notch, which forms the superior arch of the sinus, just behind the cartilage surface of the heel head.
- The posterior trochanter 2 lies behind the anterior one and attaches to the floor of the maxillary sinus, directly in front of the heel bone. Its thick fibers run obliquely upwards, backwards and outwards and attach to the roof of the maxillary sinus in front of the posterior surface of the heel bone.
The talus bone is connected to the heel bone by two other, less important ligaments (Figures 19 and 20):
- The external talofibular ligament3 begins at the outer tuberosity of the heel bone and runs downward and backward parallel to the intervening outer collateral ligament of the ankle joint and ends at the outer surface of the heel bone.
- The posterior talofibular ligament4 is a thin fibrous band that extends from the posterior tuberosity of the calcaneus to the top of the calcaneus.
'Lower limbs. Functional anatomy'.
AI Kapanji
Muscle chains and running
One should not think that all the muscles listed work unevenly 'everyone for themselves'. Rather, they obey very specific motor circuits that come from the brain, but above all from the…
All muscles of the lower limbs are important for walking. This means that the slightest deficiency in one of these muscles can lead to more or less severe gait disorders. 9 drawings.
Bone-Surgery.com – Surgery and Treatment Articles, Surgery Videos, Photos and Forum © 2010
Copying without an active link to Bone-Surgery.ru is prohibited.
Types of taping for torn ankle ligaments
The effectiveness of taping directly depends on the quality of the plasters used. The most important criteria for product selection are:
High-quality tapes ensure proper immobilization of the injured limb, help relieve pain and reduce swelling. The products may differ in their properties:
When selecting tapes, the type of taping carried out should be taken into account:
- functional. To prevent ankle injuries. Most effective use in sports;
- Immobilizing. Allows the injured ankle to be immobilized, thus preventing the risk of complications.
Rehabilitation after operations and sports injuries is therapeutic in nature; It serves to relieve pain and stabilize the joint while maintaining motor function.
Taping of the ankle joint for torn ligaments
Bandaging a torn ankle with wide ligaments with high elasticity and strength is as follows
- The bandaging starts at the toes and runs over the back of the foot to the middle of the shin;
- Another band is attached to the sole of the foot;
- The ankle and heel are bandaged separately - the middle of the band is placed on the heel side of the sole perpendicular to the length of the foot. The ends of the band are glued upwards slightly above the ankle.
For mild sprains, taping is performed in the same way, but with greater fixation of the joint. Once the tape is applied, it is tightened to achieve the necessary immobilization.
For ankle and ankle injuries, wide bands are applied from bottom to top. The ankle joint should be in a relaxed position. Absorbent tapes are recommended for ankle bruises.
Support bandages are also recommended for ankle bursitis. With this disease it is necessary to relieve the joint. The ankle is immobilized with a figure-eight bandage, then the heel is wrapped - wide, one-piece straps are attached to the sole, the ends of which are fastened 10 cm above the ankle.
Read more:- Injury to the navicular semilunar ligament.
- The pubic ligament where it is located Photo.
- The Ligamentum Treitz, where it is located.
- The hock in which the person is located.
- The ankle bruise is where the picture is taken.
- dislocation of the ankle.
- Structure of the human ankle.
- ankle-shin.
