This video shows a variant of the manual muscle test for the posterior tibialis muscle:
- tendon dysfunctions of the ankle and foot
- Anatomical and functional features of the tendons.
- etiology
- pathology
- diagnosis
- orthoses
- braces
- Our courses are suitable for both beginners and experienced trainers and offer income growth and career development.
- Why does inflammation of the shin and fibula nerves occur?
- What is inflammation of the tibial and ankle nerves?
- overview
- Anatomy of the tibial nerve
- Causes of tibial nerve neuropathy
- Pelvic muscles (muscles of the pelvic girdle)
- movements of the lower limbs
- signs of injury
- Causes of quadriceps strains
- Which doctor should I see?
tendon dysfunctions of the ankle and foot

One of the most important tendons in terms of physiological function runs along the lateral, anterior, and medial surfaces of the ankle. These tendons are the posterior and anterior tibialis tendons, the tendons of the humerus musculature, and the Achilles tendon, which are discussed separately below.
Since these tendons are responsible for human movement, they are subject to heavy use and are susceptible to injury, inflammation and subsequent tendinitis.
Anatomical and functional features of the tendons.
1. The anterior tibialis muscle is responsible for the stability of the ankle during movement (running, walking), when the foot is resting on the ground, and also provides its flexion when stepping down. It is also the muscle that applies 50 % of the force needed to lock the ankle, such as B. in football.

Fig. The tendon of the tibialis anterior muscle.
2 The posterior tibialis muscle, which originates from the fibula and tibia and attaches to the scapula on the other side, is responsible for rotating the foot, flexing the ankle and (key) stabilizing the arch of the foot.
When this muscle contracts while running or walking, it locks the ankle so it acts like a rigid lever. An injury, strain, or tear to the posterior tibialis tendon leads to the development of a widespread condition called flatfoot.
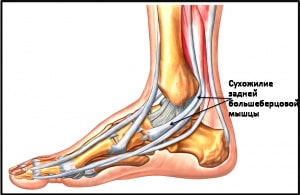
Fig. The tendon of the posterior tibialis muscle (TMP).
3 The short and long fibers that originate from and run along the fibula are attached to the metatarsal on the other side and serve to flex the sole of the foot.
The fibulae allow eversion (external rotation) and plantar flexion of the foot.
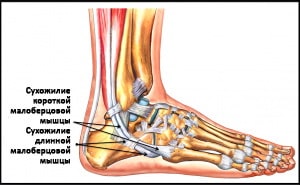
Fig. The tendon of the tibialis anterior (TAA) muscle.
etiology
The causes are unclear and are related to the following diseases:
- Obesity.
- Excessive pronation of the foot causing compression and poor blood supply to the tendon that wraps around the medial ankle deep below the point of support.
- Structural and anatomical abnormalities, e.g. B. scaphoid process, rigid or mobile flatfoot, overgrowth of osteophytes in medial malleolus groove, shallow groove and equinus of the ankle.
- Inflammatory joint disease, RA, seronegative arthritis.
- Collagen vascular diseases.
- Direct injuries where the tendon is severed through fractures of the medial malleolus.
- Indirect injuries such as ankle fracture, ankle sprain, acute rupture of bursa and sprain of posterior B/B muscle tendon.
- Iatrogenic exposure (injection of steroids into this area).
pathology
The dysfunction can be divided into 4 stages:
- Asymptomatic stage. When examining the patient, it is possible to identify hidden abnormalities that can lead to the development of dysfunction. For example, a fully compensated varus hindfoot or obesity.
- Stage of the first symptoms. Tendonitis (inflammation of the tendon sheath in the area of the flexor tendon). Slight muscle weakness b/w.
- Stage of severe dysfunction. Characterized by damage within the tendon, stretching without damage, or even detachment of the tendon from the bursa.
- Strong pronation of the medial part and abduction of the anterior part.
- acute phase. Lasts 2 weeks from the onset of the disease, in which tendon pathology may not be diagnosed. Typical: diffuse swelling, tenderness on the medial side of the ankle. Lower extremity pain and muscle fatigue may occur.
- subacute phase. It lasts between 2 weeks and 6 months. There is pain and swelling along the tendon, from the rear inner malleolus to the inner longitudinal arch. It can also be a symptom of tarsal tunnel syndrome due to local compression of the nerve. Passive movements in the subtalar and metatarsal joints are usually painless, but there is a change in gait, lack of thrust, anterior retraction, lack of supination with heel and toe strikes.
- chronic phase. Occurs after about 6 months. Patients present with a unilateral stiff flatfoot. In advanced cases, the pain may shift from the medial to the lateral side of the tarsal sinus. The lateral pain results from a progressive valgus deformity of the hindfoot leading to axial calcaneofemoral loading, periostitis, patellar tendinitis, and popliteal tendonitis.
diagnosis
– Palpation: the area behind the medial malleolus can be swollen and painful, the tendon itself is thicker if we compare its size with the opposite side
– Running analysis: The pronation time is increased and can persist even when pushing off with the toes
– ULTRASOUND, MAGNETIC RESONANCE IMOGRAPHY
Treatment
rest and relief
Continuing to walk makes the situation worse. However, rest alone is not enough, the cause of the tendinotopia must be eliminated.
To allow the tendon to rest (when you're 'on your feet' all day), taping can be applied to reduce pronation and thus reduce stress on the tendon (video or photo).
Shoes that support the arch of the foot also reduce stress on the tendon.
Another way to reduce stress is with orthotics. A well-fitting insole can make life a lot easier, especially at the beginning of rehabilitation.
exercises
Strengthening the posterior tibialis muscle is critical to treating and preventing this condition. Functionally, this muscle moves the foot from dorsiflexion and eversion to plantarflexion and inversion. We will work with this movement, gradually increasing the load. The following exercises can be used in the first phase:
orthoses
Orthotics and braces are effective for most patients. Orthoses are orthopedic insoles. This is the most common conservative treatment for flat feet.

For patients with minimal changes in foot shape, simple factory orthoses may be sufficient. Custom-made insoles are usually required for moderate to severe flat feet. The latter, of course, are more expensive than factory-made insoles, but allow for better foot position control.
braces
Wearing a lace-up brace can be effective for mild to moderate flat feet. The orthosis supports the hindfoot and relieves the tendon. In severe forms of flatfoot with stiffness in the foot and degenerative changes in the joints, a custom-made orthosis made of natural materials (leather) may be necessary. With the use of an orthosis, an operation can even be avoided in some patients.
Physiotherapeutic measures to strengthen the tendon may be effective in patients with minimal to moderate damage to the posterior tibialis tendon.
Our courses are suitable for
for both beginners and experienced trainers and offer income growth and career development.


The User purchasing services on evotren.ru, hereinafter referred to as the 'Customer', on the one hand, and Evotren LLC, hereinafter referred to as the 'Contractor', represented by CEO FG Kapishev, acting within the framework of the Charter, on the other hand, are automatically included in this Agreement ( hereinafter referred to as the 'Contract') occurs if you purchase the Contractor's services under the following conditions:
1. TERMS AND DEFINITIONS USED IN THE CONTRACT
1.1. customer – natural person, sole proprietorship or legal entity, regardless of its legal form, who has placed an order with the Contractor in accordance with the terms of this Agreement and purchases the Services of the Contractor.
1.2. contractor – is the legal entity that provides services to the Customer under the Agreement.
1.3. Services – Services consisting in giving access to the study of the distance learning materials indicated in the description of the information courses.
1.4. site – The contractor's information resource, located on the Internet at: edu.evotren.com
1.5. The client's personal account – Programming interface on the website for studying the information material and other necessary information, accessible to the customer after authorization with a login and password.
1.6. Order – An automatically generated document specifying a set of services required by the customer. The order is created by filling out the necessary forms on the contractor's website -www.evotren.ru.
1.7. Acceptance of the terms of the contract – Acceptance by the customer of the terms of the contract by paying for the services in cash or by means of cashless or electronic means of payment. The acceptance of the contractual conditions is considered to have taken place when the customer has paid for the services in cash or by means of cashless or electronic means of payment.
Why does inflammation of the shin and fibula nerves occur?

First of all, it should be clarified that by 'inflammation of the tibial and fibula nerves' we mean two different pathologies, since the inflammation can affect only the tibial ramus and only the fibula ramus in isolation.
Traumatic influences such as fractures or bruises, dislocations and others can trigger the development of inflammation in said nerves. In 2016, researchers from the Republican Clinical Hospital of the Ministry of Health of the Republic of Tatarstan, Kazan, published a paper stating that post-traumatic inflammation of the fibula nerve is a common complication of hip displacement fractures and periarticular displacement fractures.
In addition, both the ankle and tibial nerves can be affected by compression, various infectious and toxic agents, as well as vascular diseases. Sometimes the disorder occurs as a result of a surgical procedure, e.g. B. after knee or ankle surgery.
Other possible causes are various pathologies of the knee and ankle joint, tumors, metabolic disorders and others.
What is inflammation of the tibial and ankle nerves?
Inflammatory lesions of the ankle nerve are primarily characterized by restricted extensibility of the foot and toes. This causes the foot to sink downward and rotate slightly inward. When trying to place the foot on the ground, the person first puts their toes down, then leans on the outside edge of the foot and only then puts the foot down completely.
A sensory disorder is mandatory. This can manifest as pain, numbness, or other discomfort in the posterior area of the foot and the anterolateral surface of the lower leg. Gradually, signs of muscle wasting appear. Standing and walking on heels is impossible.
Tibial neuritis can be accompanied by a variety of symptoms, depending on the extent of the lesion. For example, the affected person may be unable to bend the foot downwards and no longer be able to stand on their toes. There is atrophy of the posterior muscles of the lower leg and foot and a decreased reflex of the Achilles tendon.
Sensory disturbances, pain sensations spreading to the posterior surface of the shin, the sole of the foot and the dorsiflexion of the foot are also inevitable. Sometimes there is a burning pain syndrome on the sole of the foot, which often radiates to the calf muscle.
overview
Tibial neuropathy belongs to the group of so-called peripheral neuropathies of the lower limbs, which also includes sciatic neuropathy, femoral neuropathy, peroneal nerve neuropathy and external femoral cutaneous nerve neuropathy. The similarity of the clinic of tibial neuropathy with the symptoms of injuries of the musculoskeletal system of the lower extremities and foot, as well as the traumatic etiology of most cases of the disease, make it a subject of research and joint treatment by specialists in neurology and traumatology. The association of the disease with sporting overload and repeated trauma makes the problem relevant for sports physicians as well.
Anatomy of the tibial nerve
The tibial nerve (N. tibialis) is an extension of the sciatic nerve. The nerve begins at the top of the knee and runs through it in a medial direction from top to bottom. Then the nerve lies between the heads of the calf muscles, between the long flexor of the first toe and the long flexor of the fingers. In this way he reaches the medial ankle. The transition of the tibial nerve can be felt about halfway between the ankle and the Achilles tendon. This nerve then enters the tarsal canal, where it and the posterior tibial artery are fixed by a strong ligament—the flexor collateral ligament. After leaving the canal, the tibial nerve divides into terminal branches.
In the popliteal fossa and beyond, the tibial nerve gives off motor branches to the triceps, thumb and finger flexors, popliteus, posterior tibialis, and epicondyle; the sensory internal cutaneous nerve of the tibia, which, together with the peroneal nerve, innervates the ankle, the posterolateral surface of the lower third of the tibia, the lateral border of the foot, and the heel. The terminal branches of the tibial nerve, the medial and lateral plantar nerves, innervate the small muscles of the foot, the skin of the inner margin of the sole, the first 3.5 toes, and the dorsal surface of the remaining 1.5 toes. The muscles innervated by the tibial nerve allow flexion of the tibia and foot, elevation of the inner edge of the foot (ie, internal rotation), flexion, lowering, and extension of the toes, and extension of the distal phalanges.
Causes of tibial nerve neuropathy
Femoral neuropathy can occur as a result of trauma to the nerve resulting from tibial fractures, isolated tibial fractures, ankle sprains, trauma, tendon injuries, and ligament strains in the foot. Other etiological factors are repeated sports trauma to the foot, foot deformities (flatfoot, valgus deformity), persistent deformities of the lower limbs or foot with compression of the nerve. Tibialis (common in alcoholics), diseases of the knee or ankle (rheumatoid arthritis, deforming arthrosis, gout), nerve tumors, metabolic disorders (diabetes mellitus, amyloidosis, hypothyroidism, dysproteinemia), disorders of nerve vessel formation (e.g. vasculitis).
The most common tibial nerve neuropathy is associated with compression of the tarsal tunnel (known as tarsal tunnel syndrome). Compression of the nerve at this level can occur with fibrotic lesions of the canal in the post-traumatic period, with tendinitis, hematoma, bony exostoses or tumors in the canal area, as well as with neurodystrophic disorders of the ligamentous-muscular apparatus of the joint of vertebral origin.
Pelvic muscles (muscles of the pelvic girdle)
The pelvic muscles are divided into two groups - internal and external. The internal pelvic muscle group includes the iliopsoas muscle group, the internal obturator muscle group, and the sternocleidomastoid muscle group. The pelvic external muscle group includes the gluteus medius and gluteus maximus, broad fascia, quadriceps, and external obturator.
The hamstrings are divided into 3 groups: anterior (hip flexors), posterior (hip extensors) and medial (hip drive).
Because of their large mass and considerable extensibility, these muscles are able to develop a great deal of force, acting on both the hip and knee joints. The thigh muscles have static and dynamic functions in standing and walking. Like the pelvic muscles, the thigh muscles in humans are most developed due to the upright posture.
The muscles of the lower leg, like the other muscles of the lower limbs, are well developed, which is determined by the function they perform in relation to the upright posture, statics and dynamics of the human body. The muscles of the lower leg, which originate in the bones, the intermuscular septa and the fascia, act on the knee, ankle and ankle joints.
A distinction is made between the anterior, posterior and lateral tibial muscle groups. The anterior group includes the tibialis anterior muscle, the long toe extensor, and the long thumb extensor. The posterior group includes the triceps (consisting of the calf muscle and the camel muscle), the longitudinal and biceps muscles of the thigh, the long flexors of the toes, and the posterior tibialis. The lateral tibial group includes the short and long muscles of the fibula.
In addition to the tendons of the lower leg muscles, which attach to the foot bones and belong to the anterior, posterior and lateral groups, the foot has its own (short) muscles. These muscles attach to the skeleton of the foot and have a complex anatomic-topographical and functional relationship with the tendons of the muscles of the lower limbs, which attach to the bones of the foot. The muscles of the foot are located in the hindfoot and plantar muscle.
movements of the lower limbs
The hip moves around three axes in the hip joint (triaxial – multiaxial joint). Flexion and extension (around the front axis) is possible up to 80° with the limb straight and up to 120° with the tibia flexed at the knee. Abduction and adduction (around the sagittal axis) can be performed up to 70-75° and rotation around the longitudinal axis up to 55°.
Flexion of the thigh: iliopsoas muscle, rectus femoris muscle, caudal muscle, broad fascia muscle, pectoralis muscle.
Thigh stretch: gluteus medius muscle, biceps femoris muscle, semitendinosus muscle.
Thigh Extension: Adduction of the thigh: large adductor, long adductor, short adductor, pectoralis muscle, small muscle.
Thigh retraction: gluteus medius and small muscles.
Inward rotation of the hips: gluteus medius (anterior bundles), gluteus minimus, tensor fasciae broad.
External rotation of the hips: gluteus medius, gluteus medius, gluteus major, iliopsoas, quadriceps, external and internal adductor muscles.
signs of injury
The muscles of the hip include the posterior group, quadriceps, and adductors. The quadriceps is the most commonly injured muscle, especially in athletes. Injuries in this area can be recognized by a number of characteristics. Most commonly, dislocations occur as a result of abnormal, violent movement or exercise involving excessive weight. When a dislocation occurs, the sufferer feels it:
A characteristic sign is that the person is unable to repeat the exercise that caused the dislocation. It is almost impossible to determine the stage of the problem on your own. Dislocations are often accompanied by dislocations, joint dislocations and fractures, so it is advisable to see a specialist as early as possible. The appearance of the clinical picture largely depends on the extent of the injury, which can be mild, moderate, or severe and cause the corresponding symptoms:
A strain in the posterior muscles often causes swelling and limited mobility of the joint. If acute pain occurs, the load should be stopped immediately and the leg rested.
Causes of quadriceps strains
Stretching of the quadriceps femoris muscle is most often caused by a direct blow or impact. This injury is common in sports like soccer, hockey, rugby, martial arts, and others. A sprain can also occur accidentally during active games. Another cause is insufficient muscle warm-up before exercise. They are closely connected to tendons and joints, so heavy loading without proper preparation can easily lead to an injury. Possible causes:
- direct and tangential impacts;
- lack of physical preparation;
- sloppy, sharp movement of the foot;
- injuries resulting from a fall;
- Dislocated foot, lateral sprains.
For weightlifters, the issue of sprains is especially relevant. It can happen to them due to:
- Exercising too fast;
- Excessive exposure to body weight;
- Wrong amplitude of movement;
- non-compliance with the rules of practice;
- improper warm-up.
It is well known that muscles work best when properly warmed up. That's why it's so important to stretch and warm up before exercising and to rest your legs during exercise. This significantly reduces the risk of injury.
Which doctor should I see?
To diagnose and treat a hip sprain, you should see a doctor, such as: B:
Read more:- The flexor muscles of the foot.
- Syndrome of the tibial nerve.
- lower leg muscles.
- Tendon of the tibialis anterior muscle.
- How muscles and bones are related.
- Exercises for the triceps tibialis muscle.
- tibial fasciitis.
- The long section of the big toe.
