For minor injuries that do not endanger the overall integrity of the ligamentous system, conservative therapeutic measures are sufficient. For dislocated ligaments in the knee, medications are prescribed:
- Dislocation of the knee
- Subluxations of the knee joint
- ACL structure.
- Anatomy of the anterior cruciate ligament.
- Cruciate ligament sprain in the knee – symptoms
- Cruciate ligament strain in the knee – symptoms
- Ligaments of the lower leg
- The main causes of injuries are.
- treatment and rehabilitation
- What are the first steps?
- Causes of pain in the back of the knee
- Infectious and inflammatory processes
- Diagnostic search
- Extra-articular pathology of the knee joint
- Diagnosis of knee joint problems
- Rule 3 Immobilize the injured area
- Rule 4: Medication to relieve pain and inflammation
Dislocation of the knee
There are three types of dislocations or subluxations of the knee (knee joint): tibia, meniscus, and patella. Complete (forward, backward and lateral) dislocations of the tibia are extremely rare. The knee, which bends only in the anteroposterior (sagittal) direction, is prevented from moving forward by strong intra-articular cruciate ligaments: the anterior cruciate ligament (lig. cruciatum anterius, which extends from the external condyle to the anterior intercondylar fossa of the tibia (fossa intercondyloidea anterior tibiae ) runs and is tensioned when strongly flexed, and the posterior cruciate ligament (lig. cruc. Posterior cruciate ligament), which runs from the inner condyle to the posterior and anterior edge of the shinbone and prevents hyperextension of the knee.
The force acting on the shinbone from behind or in the sense of increased flexion only leads to a tear of the anterior cruciate ligament. The posterior cruciate ligament loosens. Together with the long collateral ligaments, it prevents the joint ends from completely dislocating, so that only an anterior subluxation occurs. If the posterior cruciate ligament is torn after the anterior ligament with sustained force, a complete anterior sprain occurs.
If a force is exerted on the shinbone from the front or by hyperextending the knee joint, the posterior cruciate ligament is stretched and tears. During this posterior dislocation of the tibia, the anterior cruciate ligament relaxes and, although it remains intact, together with the long collateral ligaments prevents the tibia from completely dislocating and only a posterior subluxation occurs. Rupture of the anterior ligament with sustained force results in complete posterior dislocation.
A complete anterior or posterior tibial dislocation requires very high sustained force to rupture both cruciate ligaments.
A lateral dislocation of the lower limbs requires the tear of not only both cruciate ligaments but also both long collateral ligaments and is even rarer.
Subluxations of the knee joint
Subluxations of the knee (knee joint) are much more common: Anterior and posterior subluxations. In subluxations, only one cruciate ligament is torn, either the anterior or posterior, evident from the history and hemarthrosis, with the rupture of the anterior cruciate ligament causing acute tactile pain below the patellar ligament at its insertion on the tibial plateau and the rupture of the posterior cruciate ligament in the posterior fossa where it attaches to the tibia.
There is also a symptom of anterior and posterior subluxation of the tibia, called drawer syndrome, in which there is a slight displacement of the tibia at the ends of the thigh. If the anterior cruciate ligament of the knee is torn and the thigh and foot are immobilized, the shin bone is tilted slightly forward away from the femoral condyles with both hands; If the posterior cruciate ligament is torn, the shinbone is pushed backwards by the femoral condyles. Patients are taught how to lengthen or retract the tibial box by placing the foot on the end of the bed or another foot and tensing the muscles of the slightly flexed knee to bring the tibia forward or backward from the condyles.
Fresh subluxations are treated like dislocations - normal positioning of the ends of the knee with a bandage that keeps the limb in an upright position for 3-4 weeks, followed by massage and passive and active exercises.
With the development of skiing, soccer, ice skating and snowboarding, knee subluxations have become more common. Long-term subluxations that recur frequently and hinder walking sometimes require surgery. Several plastic surgeries have been proposed to repair torn cruciate ligaments, including arthroscopic, minimally invasive procedures using endoscopic techniques.
ACL structure.

The anterior cruciate ligament begins at the outer edge of the femur and extends through the entire knee joint to its attachment to the shinbone. It is located in the medial part of the knee. With normal development and no abnormalities, it has an anatomical rotation of 110 degrees and a twist angle of collagen fibers of about 25 degrees. When the person moves and especially stretches the joint, the ligament assumes a more upright position. When the joint is flexed 90 degrees, it approaches horizontal. The main function of the ACL is to limit the movement of the thigh relative to the shinbone. As an important part of the knee joint, it is constantly under heavy stress and is one of the most traumatized parts of the body.
The specificity of the injury is related to the specific function of the ligament - the cruciate ligament can be damaged or torn because it prevents the movement of the shinbone when subjected to a forceful impact/pressure. Occasionally the injury occurs during hip rotation when the foot is in a stationary position. Occasionally this injury is accompanied by other injuries, e.g. B. a meniscus tear or an ACL injury. In this case, the disorder affects the entire limb, and the shinbone is also injured.
You can read about the treatment of anterior cruciate ligament rupture here – diagnosis and treatment of anterior cruciate ligament rupture.
Anatomy of the anterior cruciate ligament.
The anterior cruciate ligament is stretched between the medial inner condyle of the thigh and the posterior area of the tibia. It is protected by the synovial membrane and is located within the knee joint, although further from the center of the knee. The main function of the VAS is to stabilize the joint and prevent the thigh from pulling back against the shinbone. An injury and rupture of the FAS is a rare but extremely serious injury. The most common injuries to this joint are avulsions in car accidents, skiing (high-velocity impacts), and speed sports.

- First Stage. This stage is characterized by the appearance of microcracks. In this case the diagnosis is 'sprain'. The symptoms are severe pain, swelling and restricted movement. The joint portion remains stable.
- Second. Partial rupture of the CW. The symptoms are similar to those of a first-degree injury, but are more severe and long-lasting. Any load, no matter how small, can cause a second injury.
- main page. SportClinic – joint treatment and rehabilitation in St. Petersburg
- Blog about joint treatments
- Structure of the cruciate ligament
Cruciate ligament sprain in the knee – symptoms
Signs of a cruciate ligament sprain, symptoms can include:

Knee ligament sprain symptoms
- Painful sensations in the area of injury, the severity and location of which depend on how severe the knee ligament strain is and how many structures were involved in the pathological process.
- Swelling of the tissue and congestion of the skin as a result of the inflammatory reaction.
- Restriction of movement in the joint or, conversely, the occurrence of joint instability.
The symptoms of a knee ligament strain also depend on the degree of violation of the anatomical integrity of the connective tissue fibers and the involvement of other structures (bone substrate, meniscus). A severe knee ligament strain can result in limited mobility of the knee joint.
Cruciate ligament strain in the knee – symptoms
A cruciate ligament strain of the knee is accompanied by significant pain that initially occurs immediately after the injury. The pain that indicates a cruciate ligament strain in the knee is localized in the front or back. Posterior stretching of the ligaments below the knee usually occurs when the stretch is too severe and may be associated with abnormal mobility.
Strain of the collateral ligaments of the knee joint usually occurs when a mechanical force is applied that results in abnormal forward flexion. It is accompanied by severe pain that occurs on the inner or outer surface.
A strain of the medial collateral ligament of the knee occurs less frequently, but can lead to limited mobility. Occasionally there is combined damage to the connective tissue collateral ligaments and the cruciate ligaments of the knee. In this case, the symptoms are more pronounced and the pain becomes more intense.
Ligaments of the lower leg

Knee ligament injury is a common injury that occurs more frequently in active adolescents and usually occurs at home or during sports activities. Knee joint ligament injury is caused by excessive movements of the joint (hyperextension, twisting of the limb in the axial plane, adduction or adduction of the lower limb). Sometimes the injury is caused by a shock or pressure on the lower extremity. Patients with knee ligament injuries complain of pain, restricted movement and swelling in the joint area. The diagnosis is made on the basis of history and clinical examination; X-rays can also be taken to rule out a fracture. An MRI scan of the knee joint, a diagnostic puncture or arthroscopy are also indicated.
Knee ligament injuries are a common injury that occurs more often in active young people and usually happens at home or during sporting activities. Damage to the ligaments of the knee joint occurs as a result of excessive movement of the joint (hyperextension, twisting of the limbs in the axial plane, adduction or abduction of the lower limbs). Sometimes the injury is caused by an impact or pressure on the lower extremity.
- Grade I. Partial rupture of the ligaments of the knee joint (individual fibers are torn). This is often referred to as a sprain, although the ligaments of the knee joint are actually inflexible and cannot be stretched;
- Grade II. Incomplete ligament tear (tearing of the ligaments of the knee joint);
- grade III Complete rupture of the ligaments of the knee joint. Usually associated with damage to other joint components (capsule, meniscus, cartilage, etc.).
In traumatology, a distinction is made between injuries to the collateral ligaments (outside and inside) and the cruciate ligaments (front and back), depending on the location of the injury.
The main causes of injuries are.
- Trauma (sports or direct injury to the knee joint: falls, jumps, impacts, etc.).
- Ligament weakness caused by: tendonitis (patellar ligamentitis), chronic diseases (diabetes, rheumatoid arthritis, infectious diseases, etc.), taking steroid hormones
- Numerous microtraumas to the ligament
- Previous knee surgery
- Cracking and jumping in the joint with severe pain in the kneecap area
- Bleeding and swelling in the front thigh area
- Displacement of the kneecap upwards towards the femur
- muscle cramps
- 'Sinking' of the knee when walking
- Increased sensitivity in the knee joint area
- Inability to bend the knee
treatment and rehabilitation
If the patellar ligament is only partially damaged, conservative treatment can be carried out by anesthetizing the injury site with a plaster cast. Once the cast is removed, physical therapy, mud baths, and other treatments are recommended to restore mobility. In most cases, the patellar ligament is torn and surgery is required. During the operation, the torn ligament is sewn with stitches through holes in the bone at the tip of the kneecap. After the operation, the patient is given pain medication and the limb is immobilized with a splint or cast (if immobilized). The patient can also be moved with the help of crutches. After a certain period of time, the splint or cast is removed and the patient receives a course of treatment for improvement: therapeutic exercises, laser therapy, massage, ultrasound, etc.
Qualified medical care can be obtained in Moscow at NCC No. 2 (Central Clinical Hospital of the Russian Academy of Sciences).
What are the first steps?
If the pain in the back of your shin is very severe or you are unable to straighten your leg while walking, you should see your doctor for appropriate treatment.
Stop the activity causing the pain and place an ice pack on the back of your thigh as soon as possible.
Depending on the severity of the injury, you should rest your leg for one to three weeks. Repeat the application of ice packs at least once daily for two to four days after cessation of activity to reduce pain and swelling.
Applying an elastic bandage around the thigh during exercise reduces pressure by compressing the quadriceps and hamstring tendons. In any case, you should keep your legs slightly elevated and stretched forward.
Do not resume physical activity until the pain has subsided. Gently and gradually bend and straighten the leg. Perform tendon and quadriceps toning exercises under the guidance of a physical education instructor or physical therapist.
If the rest period and recovery exercises are carefully followed, there will be no long-term consequences.
To avoid recurrence, you should warm up sufficiently before exercising and work the muscles in the problem area.
Causes of pain in the back of the knee
- Infectious and inflammatory processes;
- autoimmune diseases;
- Degenerative and dystrophic processes;
- Neoplasms and tumor-like growths.
Infectious and inflammatory processes
Infectious processes can be related to trauma, poisoning, allergies, vaccination complications, or a combination of these factors.
The synovial membranes and periarticular tissue are well supplied with blood, and the joint structures are quickly involved in the inflammatory process. Common inflammatory diseases causing pain in the back of the knee include:
- Arthritis. Often complicated by post-traumatic conditions and infections. Arthritis is diagnosed against the background of rheumatic diseases. The disease occurs in acute and chronic forms. In the first case, the symptoms are clear; the pain can occur both outside the knee and in the back of the knee.
- Synovitis. Synovitis of the joint is not considered an independent disease. The pathological syndrome occurs as a complication of other joint diseases. The synovial fluid accumulates and the contents of the capsule become infected. The skin becomes shiny and swollen. The pain affects the entire knee, both from the outside and from the inside.
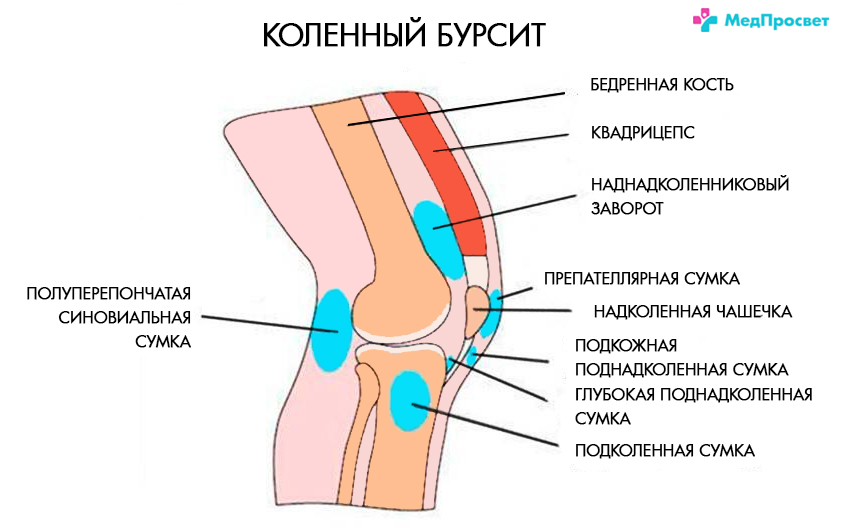
- bursitis – Inflammation of the joint capsule. The disease occurs with overuse and repeated trauma. The pain is localized to both the kneecap and the back of the knee.
- Lipoarthritis or Goff's disease. Occurs in athletes and the elderly. The pain is aching, dull and debilitating. Pain under the knee can occur at night. Feeling of slipping in the legs.
- Inflammation or damage to the blood vessels/nerves in the back of the knee (popliteal fossa). The tibial nerve, vein and popliteal artery are located in the ankle joint. Acute pain suggests entrapment, trauma, or hypothermia. Sometimes the pain is caused by thrombosis of the popliteal vein, osteoarthritis of the knee joint, or Baker's cyst.
Diagnostic search
Diagnosis of arthralgia in the knee joint is always difficult due to the polyetiology of the pathology. To make an accurate diagnosis, various tests can be carried out:
- Ultrasound of the knee joint – available method based on the study of soft tissue structures, presence of effusion;
- puncture – is an invasive examination method in which a part of the synovial fluid is removed using a thin cannula for histomorphological examination;
- General clinical blood tests, urinalysis – indicates inflammation and possible systemic abnormalities;
- X-RAYS – X-ray in two projections: bone condition, cartilage structure, contouring, anatomical criteria and more;
- arthroscopy – an invasive endoscopic examination to reliably demonstrate structural tissue changes – tissue can be removed for biopsy during the examination;
- MRI of the knee joint – MRI is a non-invasive examination used to visualize structures of the knee joint (ligaments, muscles, meniscus, cartilage, etc.) and pathologies (tumors, inflammatory processes, vascular pathologies, salt deposits, etc.).
If you have pain in the knee joint, a visit to a surgeon or orthopedist/traumatologist is indicated for treatment. You can make an appointment at the MedProsvet clinic by calling +7(812)374-84-00 or submit a request on the website.
Extra-articular pathology of the knee joint
– Tendonitis in the knee joint.
Excessive or improper strain on the tendons of the upper and lower leg muscles leads to their inflammation - tendinitis. Pulling pain at the front of the knee joint is caused by damage to the patellar tendon and quadriceps tendon - the most common cause of knee pain. Discomfort on the outside of the knee is caused by the iliotibial tendon rubbing against the femur - a condition known as runner's knee. On the inside, the muscles that attach the hamstring, scapula, and semitendinosus are known as goosebumps. The tendons of the calf muscle, biceps femoris and biceps femoris are located in the hamstring fossa. Damage to these tendons can lead to pulling pain in the back of the upper and lower leg.
– Musculofascial syndrome.
Painful muscle tension, called trigger points, causes discomfort and pulling in the knees when walking, running, climbing stairs, and squatting. Diseases of the knee joint or microtrauma of the muscles themselves lead to these points.
– Inflammation of the lymph nodes.
There are lymph nodes in the back of the knee that collect lymph fluid from the foot and lower leg. Infectious processes in the lower extremities or impaired lymphatic drainage lead to enlarged lymph nodes and symptoms.
– Varicose veins of the lower limbs
Benign varicose veins are asymptomatic. Swelling of the lower limbs, swollen veins and varicose vein nodes, as well as pulling in the legs require treatment. If you notice discoloration of the lower leg, severe one-sided swelling, pulling pain along the veins, or pain when palpating the veins, you should see a doctor immediately. These are symptoms of thrombophlebitis, a dangerous condition that requires immediate treatment.
Pain in the knee joint is also caused by herniated discs L2-L4, inflammation of the femoral and sciatic nerves. In rare cases, pulling pain in the knee joint is a sign of osteoarthritis in the hip or overloading of the ankle joint.
Diagnosis of knee joint problems
Diagnosing the problem is half the battle. At the beginning of every diagnosis there is a questionnaire: Find out what and where it hurts, how long it lasts and what the causes are. I then examine the knee joint closely and carry out special tests. I often notice a connection between knee pain and flat feet. In order to make an accurate diagnosis and initiate treatment, instrumental diagnostics is required. For this purpose, the following investigations are carried out:
– Magnetic resonance imaging of the knee joints.
This is the most accurate method for diagnosing intra-articular pathologies. Ligaments, meniscus, articular cartilage, tendons and joint capsules are clearly visible. The power of the device must be 1.5 Tesla to get a good image. If the patient wears a metal prosthesis, MRI is contraindicated. In this case, a combination of x-rays and ultrasound is informative.

– Ultrasound examination of the knee joints.
A good method for the diagnosis of periarticular tissue, Baker's cysts, vascular disorders and lymph nodes. Ultrasound allows assessment of tissue conditions at a significant distance from the joint that cannot be achieved with standard MRI.
– X-ray examination of the knee joints.
X-rays of the knee joints are a standard examination in the outpatient clinic. It provides information about the condition of the bone and articular cartilage and helps to rule out fractures. Most diseases that cause knee joint pain are not associated with bone damage. X-rays are therefore not very informative and are rarely indicated.
– Computed tomography of the knee joints.
This examination shows the condition of the bone most accurately and provides indirect information about the periarticular tissue. The main indications are the suspicion of a fracture, aseptic necrosis or the presence of an endoprosthesis. A CT scan exposes the body to a high level of radiation and should not be carried out without a doctor's referral.
Rule 3 Immobilize the injured area

A supportive bandage is always applied to the area of the sprain. This helps to immobilize the injured muscle or ligament, thereby accelerating healing and tissue repair.
The bandage should be snug enough but not restrict blood circulation in the injured area. Otherwise, the swelling will only increase or the blood vessels will become pinched, causing numbness in the limb. Ask your trauma surgeon for advice on which bandage is best and how to apply it correctly. In some cases, special orthopedic bandages (bandages) may be recommended.
Rule 4: Medication to relieve pain and inflammation
The need for medication depends solely on the severity of your symptoms. Your doctor may prescribe painkillers for severe pain and anti-inflammatory medications for swelling. Dual-acting painkillers and anti-inflammatories have been shown to work well. These include non-steroidal anti-inflammatory drugs: aspirin, ibuprofen, diclofenac. However, these medications should be used with caution and not for longer than 1 week. The use of warming ointments and gels is possible only from the third day and only with the consent of the traumatologist for mild to moderate sprains.
Stretched ligaments and muscles can lead to loss of mobility at the injury site, increasing the risk of re-injury. It is therefore essential that the patient performs a series of exercises as part of his rehabilitation to promote muscle recovery. Such prophylaxis takes place under the guidance of a specialist. For athletes, this can be done as part of normal training; for home injuries, this can be done in the physiotherapy practice of the nearest health center.
Depending on the severity of the sprain, the doctor will determine when therapy should begin. For example, if you have a moderate injury, you can start as early as the 10th day; if you have a torn ligament, training will have to be postponed for a month or longer.
Read more:- Rupture of the ankle.
- Axis of rotation of the knee joint.
- Rupture of the medial collateral ligament.
- Femoral collateral ligament.
- The medial surface of the tibia.
- tearing of the joint capsule.
- lower leg flexion.
- Diagram of a joint with and without a dislocation.
