As is known, the tibia is composed of the fibula and the tibia, so the duration of the cast depends directly on the injury and the complexity of the fracture. A closed fracture of the fibula lasts between 1 and 1.5 months, while a fracture of the tibia lasts 3 months or longer. In the event of a fracture of two tibia bones, a plaster cast is worn for up to 4 months or longer.
- tibia and fibula
- Treatment of diaphyseal fractures of the tibia and fibula
- Symptoms and causes of injury
- Fracture of the intercondylar process and condyles
- Fracture of the tibia and fibula
- diagnosis
- Types of fractures
- clinical picture
- For traumatic injuries to the fibula
- With a tibia fracture
- Diaphyseal fractures of the tibia in children.
- Fractures of the inferior tibial metaepiphysis.
- Symptoms of a broken bone
- Treatment of a tibia fracture
- signs of injury
- Causes of tibia fracture
- Which doctor should I see?
- Causes of tibia fractures in children.
- First aid
- Causes of lower back pain
- traumatic injuries
- diagnosis
- Symptoms of a displaced tibia fracture
- causes of injury
- Which doctor treats a stress fracture?
- Treatment of a fractured tibia
- Conservative treatment
- Surgical treatment – surgery for a fractured tibia
- prophylaxis
tibia and fibula
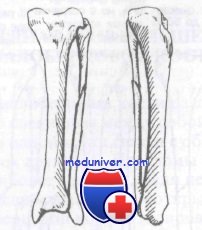
tibia and fibula The tibia and fibula lie parallel to each other and are strongly connected to each other by ligaments. As a rule, a displaced fracture of one bone is inevitably associated with a fracture or ligament injury of the other. Fractures of the tibia are not only the most common fracture of all long bones, but also the most common open fracture.
Diaphyseal fractures of the fibula rarely occur alone, usually in combination with fractures of the tibia. The fibula is not supported and can therefore be resected proximally without affecting function. In the distal section, the fibula is important for maintaining ankle stability.
Isolated Isolated diaphyseal fractures of the fibula are only treated symptomatically; they usually heal without complications.
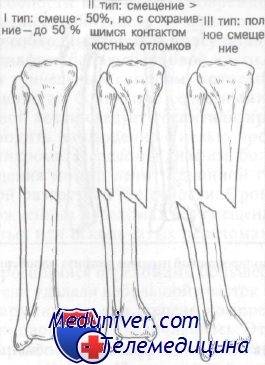
fractures of the tibia are classified based on the information provided by Nicoll and used by Rockwood and Green. According to Nicoll, three factors determine the outcome of tibia fractures: (1) the initial displacement, (2) the degree of fragmentation, and (3) the presence of soft tissue damage (open fracture).
Under Type I fractures There is only a slight displacement (0 to 50 %) and no crushing. In type II fractures, there is a displacement of more than 50 % and partial fragmentation may occur while the bone contact remains intact. Type III fractures involve complete displacement with crushing. Type II and III fractures can be open or closed. Type I fractures have a chance of healing of 90 %, while type III fractures only have a 70 % chance of healing.
shin The lower leg has three fascial sheaths that contain muscles, nerves and blood vessels.
1. The anterior sheath contains the anterior tibial muscle, the long thumb tendon, the third fibula, the long toe tendon, the anterior tibial artery and the deep peroneal nerve.
2. the outer covering contains the long and short muscles of the thigh and the superficial femoral nerve.
3. the posterior sheath contains the hamstring muscle, the calf muscle, the posterior tibialis muscle, the long flexor thumb and the long flexor finger.
Treatment of diaphyseal fractures of the tibia and fibula
Emergency treatment of diaphyseal fractures Fractures of the tibia require an initial examination, immobilization with a long shin belt and urgent referral to an orthopedist. Open fractures must be treated carefully and the wound should be immediately dressed with a sterile dressing. Emergency reduction of a closed fracture is indicated prior to obtaining radiographs if there is a vascular injury that threatens the viability of the limb.
Due to the high complication rate after taking x-rays, an urgent orthopedic consultation is required. In patients with diaphyseal fractures of the tibia, tunnel syndrome usually occurs at the same time, which only develops later. Therefore, most patients with severe diaphyseal tibia fractures should be hospitalized and the limb elevated and monitored to prevent the development of tunnel syndrome.

Diaphyseal fractures of the tibia Type I fractures without displacement can be treated with a long tibial cast, with full weight bearing on the limb. The average recovery time for uncomplicated fractures without displacement is 10-13 weeks. For displaced, open or displaced fractures, the recovery time is extended to 16-26 weeks.
In patients with didn't heal In patients with unhealed fractures, some researchers have removed a small piece of the fibula and found that compression between the two ends of the tibia was increased. This resulted in a higher healing rate in patients with complex tibia fractures. Nonunion of diaphyseal fractures of the tibia is a complex problem.
To improve the Consolidation Pulsed electromagnetic fields have been used to improve consolidation. Successful results were achieved in approximately 87 % cases and no further surgical treatment was required. Isolated diaphyseal fractures of the fibula are treated symptomatically. A plaster cast can be applied to relieve pain. Initially a long shin cast is more comfortable, after 2 weeks a short cast can be applied, which can be removed after 4 weeks.
Some patients had Some patients experienced only mild painSome patients have had no pain at all and can walk easily on crutches without a cast.
Symptoms and causes of injury
The symptoms of a tibia fracture are easy to recognize because clear signs appear immediately after the injury. The main symptoms include:
- Severe pain between knee and foot;
- Swelling;
- A cracking sound when you try to move your leg;
- inability to support the leg;
- stiffness in the limb;
- dullness and pallor of the skin at the site of injury;
- Shortening or lengthening of the limb.
These are the main symptoms that indicate a tibia fracture. Depending on the location of the injury and its stage, different symptoms may occur.
Nobody is safe from a lower leg injury. Most fractures occur as a result of a fall, a traffic accident or an impact. Athletes and older people are particularly at risk. In any case, medical attention should be sought after an injury, as the prognosis depends on the quality of initial care, treatment tactics and the rehabilitation period.
The clinical symptoms of a fracture are almost identical, but there are some differences depending on the location of the injury.
Fracture of the intercondylar process and condyles
When the intercondylar process is fractured, the following symptoms may occur:
- Swelling around the knee joint.
- Inability to move the leg.
- Bleeding into the joint cavity.
- Severe pain that increases on palpation or with any movement.
- Deviation of the tibia to the side with displacement of the fragments.
Fracture of the tibia and fibula
In the case of a fracture of the tibia and fibula, the clinical picture is as follows:
- Swelling and deformation of the leg.
- Bleeding, hematomas.
- Wound with bony protrusions (in open fracture).
- Shortening of the leg.
- Crepitation.
- Clear palpation of bone fragments.
diagnosis
Some lower leg fractures can easily be mistaken for a sprain or bruise, so you should see a doctor as soon as possible after the injury. Upon admission to the trauma unit, the doctor will conduct an examination and recommend an X-ray of the lower leg to assess the condition of the bone and determine the site of the injury and its extent.
If necessary, an MRI scan will be ordered to assess not only the condition of the bone but also the surrounding tissues. This diagnostic method allows the doctor to obtain a more complete clinical picture, make the correct diagnosis and carry out the necessary treatment.
Types of fractures
The shinbone has the most important supporting function. This small bone practically does not carry any axial load, but its importance lies in the formation of the knee and ankle joints. Depending on the strength of the impact, the shinbone can be damaged on one or both sides.
Depending on the location of the injury, its type and the number of bone fragments, clinical traumatology distinguishes the following types of disorders of tibial integrity
- Single and multiple fractures;
- Simple, oblique and spiral fractures;
- Simple and comminuted fractures;
- With or without dislocation;
- Open and closed fractures;
- Extra-articular and intra-articular fractures;
- Fracture of one or both tibias at different levels – fracture of the tibial condyles or fracture of the head and neck of the fibula, which is the upper part of the tibia. Ankle fractures are the lower part of the shinbone.
The type of bone defect determines the type of medical care, duration of treatment, and recovery time.
clinical picture
The symptoms of shin injuries are always different. Violation of one or another skeletal structure has its own nuances. Regardless of the type and location of the fracture of the lower limbs, the following symptoms occur when a bony structure is fractured
- Severe pain syndrome;
- Rapid increase in swelling of the lower limbs;
- discoloration of the skin;
- lack of active movement in the affected limb;
- Creaking of bone fragments when trying to move the leg;
- Deformity of the affected limb.
The appearance of these symptoms after trauma always indicates a tibia fracture. Distinguishing one lesion of one tibia from another is facilitated by the specific clinical features of each tibia.
For traumatic injuries to the fibula
Traumatic injuries to the fibula are accompanied by specific clinical symptoms. In addition to the general symptoms characteristic of a tibia fracture, the following symptoms occur with a fibula injury:
- Pain in the fracture area due to a periosteal defect with radiation into the ankle joint;
- percutaneous sensory disturbances on the outside of the lower leg and foot due to injury to the peroneal nerve caused by a fracture of the fibular head and neck. If there is extensive damage to nerve fibers, paresis of the foot muscles occurs with immobility of the foot;
- Hematoma at the fracture site after some time;
- Deformation of the limb due to displacement of bone fragments is possible.
Since the shinbone is the main support of the leg, the muscular framework around the shinbone is much more pronounced. If you break your tibia without dislocation, you can step on the broken limb, but the pain will be more severe.
With a tibia fracture
In addition to acute pain syndrome, the following injury symptoms can be observed with a tibia fracture:
Diaphyseal fractures of the tibia in children.
In 60 % cases, a bone (the tibia) is broken. In 40 % cases, both bones are broken. Generally the injury is located in the middle third. The fracture line usually runs obliquely, spirally or transversely; multiple comminuted fractures are rare.
The clinical signs are striking, making the diagnosis easy to make. Severe pain occurs after a fall or blow to the leg. The child is unable to put his foot up. Swelling appears at the site of the injury, possibly a hematoma. Deformation, crunching and mobility of the fragment can be noted.
To clarify the diagnosis and determine treatment, x-rays of the shinbone are taken. A CT scan is usually not necessary. If soft tissue interposition is suspected, the child may be referred for an MRI scan of the lower leg.
Peripheral vascular and nerve damage is not common with this injury. However, if such an injury is suspected, a pediatric neurosurgeon or a pediatric neurologist and vascular surgeon should be consulted.
Treatment is inpatient and carried out by a pediatric traumatologist. For fractures and breaks without displacement, a deep plaster cast is placed on the slightly bent shinbone for 2-3 weeks.
For spiral, transverse and oblique fractures with small displacement, a one-stage reduction of the tibia under anesthesia is possible, followed by a plaster cast for 4-5 weeks.
If there is significant displacement and unsuccessful attempts at repositioning, skeletal traction is indicated for 2-3 weeks. A plaster cast is then applied for another 2-3 weeks.
All fractures with displacement must be x-rayed at least three times: immediately after reduction or traction, 4-6 days later and before removal of the cast. If the child is in skeletal traction, the number of x-rays increases to four - the fourth is taken before the traction is removed.
Surgical treatment of tibia fractures in children is carried out if:
- If it is not possible to successfully reduce the fracture and achieve satisfactory stability with skeletal traction.
- Interposition of tissues.
- Open fractures.
- Risk of damage to skin, nerves and blood vessels through fractures.
Fractures of the inferior tibial metaepiphysis.
Osteoepiphysis of the lower end of the tibia associated with a fracture of the lower third of the fibula usually occurs in childhood. Fractures of the ankle joint occur less frequently. The cause of the injury is usually plantar flexion of the foot.
With osteoepiphysiolysis, the child complains of pain when trying to move and feel. Support is not possible. The ankle joint is swollen and sometimes the skin in this area turns blue or purple. A severe sprain causes deformation of the joint area and some outward extension of the foot.
X-rays of the ankle joint allow a definitive diagnosis. For fractures without dislocation, a comparative X-ray of both joints is taken. In difficult cases, the child is referred for a CT or MRI scan of the ankle.
If there is no dislocation, the child is placed in a plaster cast for 3 weeks. In osteoepiphyseal cases with a dislocation combined with a fibula injury, reduction is performed under general anesthesia. The fracture is then immobilized with a plaster cast and X-rays are taken. A follow-up examination will be carried out 4-6 days later. The duration of immobilization is 3-4 weeks.
Children with nondisplacement fractures are treated on an outpatient basis by a pediatric trauma surgeon. In the event of a dislocation, hospitalization is possible.
Ankle fractures are more common in adolescents. As a rule, the fracture does not shift. The clinical presentation of nondisplacement fractures is mild. There is some swelling and pain, and support is somewhat limited.
Fractures with displacement result in severe swelling and a more or less noticeable deformity. The pain is severe. Support is not possible.
Radiological examination provides an opportunity not only to confirm the diagnosis, but also to assess the degree of displacement of the fragment. A CT or MRI scan of the joint is rarely required, usually for non-dislocation fractures.
Injuries without dislocation are treated in a trauma center. Your child will receive a plaster cast for 2-3 weeks and then physiotherapy and physical therapy.
Symptoms of a broken bone
The patient complains of acute pain. The shinbone is deformed: shortened, twisted (the foot points inwards or outwards in relation to the knee joint), bent at an angle. Crepitus and abnormal mobility can be observed at the injury site. Supporting and moving is not possible. Swelling increases over time: there may be no swelling immediately after the injury, but the lower leg swells and bruising forms on the skin. An open injury involves a wound on the lower leg in which bone fragments may be visible.
The diagnosis is confirmed by an x-ray of the lower leg. Examination of the radiographs makes it possible to determine the number of fractures and the type of displacement, the presence or absence of an accompanying fibula fracture and the involvement of the ankle and knee joints. In some cases (usually joint damage), the patient may be referred for a CT scan of the joint. If nerve or vascular damage is suspected, a consultation with a vascular surgeon, neurologist or neurosurgeon is indicated.
Treatment of a tibia fracture
Before hospitalization, painkillers are administered and the shinbone is immobilized with a splint or other suitable aids (e.g. two boards). The lower part of the splint should cover the ankle and the upper part should reach the upper third of the thigh. For open fractures, foreign bodies and larger debris are removed from the skin around the wound and the wound is covered with a sterile dressing. If bleeding is severe, a tourniquet is applied to the thigh. If traumatic shock is present (can develop with multiple and simultaneous injuries), anti-shock measures are taken.
Inpatient treatment depends on the severity and type of injury and can be conservative or surgical. In the case of stable shinbone fractures without dislocation (very rare), a plaster cast can be used to immobilize the shinbone. In other cases, skeletal traction is required. A splint is inserted through the heel bone and the leg is supported on the splint. The average initial weight of an adult is 4-7 kg and depends on body weight, muscle development and the type and nature of the fracture displacement. The weight can then be reduced or increased as needed.
There are two other options. Conservative treatment involves maintaining skeletal traction for 4 weeks and achieving normal alignment of the fracture. As soon as radiological signs of callus formation appear, traction is removed and the leg is placed in a plaster cast for another 2.5 months. In the initial stages, the patient is prescribed painkillers. Physiotherapy and physical rehabilitation are indicated for the duration of treatment. After the plaster cast is removed, rehabilitation is carried out.
Indications for surgical treatment are multiple fractures with displacement, in which the correct alignment of the fractures cannot be restored by conservative methods. In addition, surgical treatment serves to resuscitate the patient early and prevent the development of post-traumatic contractures. In most cases, the operation is performed a week or more after the patient is admitted to the hospital. By this time, the patient's condition has usually returned to normal, the swelling of the limb has decreased, and doctors have time to conduct a comprehensive examination to determine whether there are any contraindications to surgical intervention. In the preoperative period, the patient undergoes skeletal traction.
signs of injury
The tibia is tubular and hollow inside. The connective tissue cells are arranged in layers and form a compact skeleton. This anatomical structure makes the bone less susceptible to compression and tension, but it is susceptible to twisting and bending. During mechanical trauma, when a force is applied to part of the bone, a fracture can occur. Complications in the form of splinting, displacement and resulting soft tissue damage are not uncommon. A fracture of the tibia has the following symptoms
- Severe pain at the site of the injury, which may radiate to the thigh and ankle;
- inability to strike foot;
- Restriction of movement of any limb;
- swelling and bruising;
- In case of dislocation, deformation of the leg;
- Characteristic crunching at the time of injury and due to friction of the fragments;
- Abnormal mobility of the bone.
With an open fracture there is also the risk of high blood loss and infection. Connective tissue, bone fragments, damaged ligaments and vessels may be visible in the wound.
Causes of tibia fracture
For anatomical reasons, the connective tissue of the human leg can withstand very high loads and mechanical stress. But these also have their limits: competitive sports, trauma at work or at home as well as debilitating illnesses can lead to fractures. The tibia loses its integrity under these conditions:
- Vertical impact;
- excessive pressure;
- twisting of the bone;
- Fracture due to dislocation;
- contact with a hard rib;
- Kick the knee or foot.
A fractured tibia is a particularly dangerous injury for older people. The age-related changes in the body impair the coordination of movements, lead to a deterioration in the biochemical composition of connective tissue and a loss of bone strength. Therefore, even a small impact can cause a fracture that takes much longer to heal than in people of younger ages.
Which doctor should I see?
The faster the injured person receives first aid, the faster the main symptoms of the disease - pain, swelling, inflammation - disappear. It is important to see a specialist, especially if you have complicated injuries. A displaced tibia fracture can be repaired by a doctor:
Causes of tibia fractures in children.
The integrity of the bone can be compromised by direct pressure on the shinbone with a blunt or sharp object or by indirect pressure, such as with a hand. B. in the event of a fall with your foot pulled up, can be affected. Such situations can occur both in everyday life (at home, in kindergarten, at school, while walking) and during sports. The bones of the lower limbs are also often injured in various traffic accidents and falls from heights, coupled with injuries to other parts of the musculoskeletal system and internal organs.
The symptoms of the injury largely depend on its location. With a fracture of the upper part of the shinbone, the child feels pain when bending the knee and walking. The knee swells and hurts when pressure is applied, but the function of the limb is reasonably intact. Similar symptoms occur with embedded fractures.
Injuries to the middle third of the tibia are accompanied by noticeable symptoms that cannot be ignored. Immediately at the time of injury, severe pain occurs, which increases with movement and when attempting to stand on the leg. Swelling and subcutaneous bleeding occur quickly. There is a pronounced deformation of the leg with displacement of bone fragments, and the sensation of the injury site is often accompanied by a crunch (crepitation) of the bone fragments. Accompanying nerve damage leads to numbness in the limb.
The injury to the lower part of the shinbone usually occurs when the foot is turned upward. It is difficult to distinguish the fracture from torn ligaments or other ankle injuries. There is swelling of the area, a gradually growing subcutaneous hematoma, and severe pain.
First aid
If the lower limb is injured, it must be immobilized with a suitable splint or the injured limb must be wrapped around the other leg. A cold compress should be applied to the injured leg and the child should be taken to the clinic. Depending on the child's age, painkillers may be given.
After examining and clarifying the circumstances of the injury, the doctor will order an X-ray of the injured leg. In some cases, an additional CT or MRI scan is necessary to better visualize the injury site. If there is suspicion of damage to the large vessels or nerves, a vascular surgeon, neurologist or neurosurgeon is consulted.

Causes of lower back pain
traumatic injuries
A lower leg bruise most often occurs after a blow, less often after a fall. There is a short-term, severe acute pain that quickly subsides and becomes a dull, aching, mild to moderate pain. There will be swelling and bruising at the site of the bruise. The support is maintained, but movement is somewhat restricted due to the pain. Claudication is occasionally observed.
A hematoma is similar to a bruise in its formation mechanism and clinical symptoms, but the pain is of a compressive, pumping nature, due to the accumulation of blood in the soft tissues. It differs from a bruise in that it has a dense, limited swelling or area of fluctuation that persists over a long period of time. Bruises usually occur on the skin.
An injury to the Achilles tendon is accompanied by acute pain similar to that of a blow or cut on the back of the lower leg, just above the ankle joint. The examination reveals swelling, pain when palpated and a feeling of pressure on the Achilles tendon. Soleus flexion of the foot is not possible with a complete tear and is limited with a partial tear. The grip is significantly impaired.
Shin fractures are caused by high-energy impacts: a fall from a height, a collision with a car, an accident at work. They manifest themselves as explosive pain, which then subsides somewhat but remains very intense. A crunching sound is heard at the time of injury. The following types of injuries are possible:
- Fracture of the tibia. Occurs as a result of an impact, sprain or fall. Usually associated with a fracture of the fibula. Accompanied by unbearable pain, displacement of fragments, significant swelling, deformation of the limb, extensive bruising, crepitus, pathological mobility. Support is not possible and the movement is extremely painful.
- Isolated fracture of the fibula. Caused by a direct blow. Symptoms include local swelling and bruising at the injury site. The pain is moderate and increases quickly when the fracture site is palpated. If the fracture line is in an area not covered by muscle, a step is noted. The supporting function of the limb is only slightly impaired.
diagnosis
Patients with pain in the lower extremity are initially referred to an orthopedic traumatologist. If necessary, patients are referred to surgeons, neurologists and other specialists. The examination plan includes:
- anamnese. The doctor determines when and under what circumstances the pain first appeared, establishes the connection of the pain syndrome with external factors, identifies other complaints and examines the patient's life history.
- Physical examination. The specialist assesses the condition of the limbs, detects swelling, congestion and other pathological changes. If vascular disease is suspected, pulsation in the arteries of the foot is examined, and if neurological symptoms occur, a neurological examination is required.
- X-ray examination of the lower limbs. This is the primary examination for hard tissue lesions. It is indicated in the differential diagnosis of some soft tissue anomalies. It shows fractures, changes in bone structure, periosteal hypertrophy and other changes.
- Computed tomography and magnetic resonance imaging. They are carried out in the final stages of the diagnostic search when radiological findings are unclear in order to clarify the conservative or surgical treatment plan. They allow precise localization of the pathological focus and determine its size, structure and configuration.
- ULTRASONIC EXAMINATION. Doppler and duplex examinations are carried out for vascular diseases. These techniques offer the opportunity to assess the condition of the vascular bed and the speed of blood flow and to detect areas of vascular occlusion or dilatation.
- Electrophysiological studies. Electromyography, electroneurography and electroneuromyography are performed for pain of neurological origin to determine the degree of damage to nerve trunks and to study the condition of muscles and nerves.
- laboratory tests. To assess the severity of inflammatory processes, to examine the body for systemic pathologies.

Symptoms of a displaced tibia fracture
If the integrity of the bone is compromised, serious complications can occur. These include splinting, fractures, dislocations and open injuries. The degree of damage to the surrounding soft tissues - muscles, ligaments, blood vessels, nerve fibers - is also important. During a dislocation, the external shape of the limb becomes noticeable - bone fragments can deviate from their axis, cross each other, change the angle of inclination. It is not uncommon for this type of lower leg fracture to be open - sharp hard tissue can pierce the muscle and skin. Regardless, the injury can be recognized by the following symptoms
- Severe, stabbing pain at the site of injury, sometimes radiating to the foot and thigh;
- Inability to step on the foot and move it freely;
- Severe swelling and bruising;
- Abnormal bone mobility;
- visualization of a tibial deformity;
- Protrusion of nodules under the skin;
- Crunching at the time of injury and when moving the leg.
Depending on the angle and force with which the bone was abused, several types of injuries can be distinguished. These differ in the number of fragments and the axis of injury. These types include fractures of the tibia:
The accompanying symptom is an increase in local or general fever. In response to the pain, weakness, dizziness, chills, nausea and, less commonly, vomiting may occur. In open trauma, the focus is on bones and connective tissue.
causes of injury
Thanks to the elastin and collagen fibers, the bones are able to withstand high loads, but these reserves are also limited. Most commonly, injuries occur due to sudden mechanical impact on a small area of the lower limbs. A fracture can also occur if the bone is held in place by an object or rigid footwear such as ice skates or ski boots. Injuries can occur under the following conditions:
- in case of a fall;
- severe vertical impact;
- twisting of the bone;
- negative pressure;
- through fracture and bending;
- due to strong impact;
- Landing on a flat tire.
An open fracture of the tibia is possible both as a result of the formation of bone fragments and as a result of additional soft tissue injuries - for example, as a result of an impact in a car accident. Competitive athletes and people who work in difficult jobs are particularly at risk. This injury also occurs in children as a result of falls and active play.
Which doctor treats a stress fracture?
The overall severity of the fracture helps prevent those affected from delaying a visit to the hospital. Timely treatment can help relieve pain and discomfort as quickly as possible and support the healing process. Your doctor can help you manage the problem:
Treatment of a fractured tibia
Treatment of a fracture depends on the severity of the injury and the general condition of the patient. The prognosis is determined by timely medical care and excellent anastomosis of bone fragments. Delayed and inadequate treatment can lead to adverse consequences in the form of permanent post-traumatic deformity and impaired leg function.
Conservative treatment
Conservative treatment is only possible for fractures that have not shifted or where adequate closed reduction can be achieved. Another indication is that surgical treatment is not possible (severe general condition, unsatisfactory condition of the soft tissue in the area of injury, refusal of the patient). Closed reduction of the fracture is performed under anesthesia with the application of a plaster cast (if necessary). Immobilization lasts a total of up to 8-12 weeks, depending on the type of fracture and regular X-ray checks.
Surgical treatment – surgery for a fractured tibia
The operation of tibial fractures is carried out on the basis of the following indications:
The main surgical treatment for tibial fractures is open reduction and internal fixation. The operation includes the following steps:
- restoration of bone integrity;
- Restoration of joint block (if the joint is damaged);
- bone grafting into the defect;
- Fixation of the joint block to the intact bone segment.
If there is significant bone fragmentation and obvious soft tissue damage, anatomical repositioning of the articular surface may be dangerous and/or impossible. In these cases, an external ring-shaped fixator, e.g. B. an Ilizarov device can be used for definitive treatment of the fracture. For some relatively simple types of tibia fractures, intramedullary osteosynthesis may be used for immobilization.
prophylaxis
Fracture prevention primarily consists of avoiding injuries. The risk of bone fractures increases in winter. That's why it's important to learn how to fall correctly (grouping). Wearing protective equipment is mandatory when working at heights.
Rehabilitation after a fracture of the tibia includes the following measures:
- Physiotherapeutic exercises to build muscles and joints;
- Physiotherapy to improve the functional status of the soft tissue and bone compartments;
- stimulating massage to improve muscle condition.
- fibula.
- Why the shin hurts.
- What is the connection between the femur and tibia?.
- Pain in short fibula when walking.
- ankle-shin.
- function of the fibula.
- The lateral ankle is.
- Fracture of the lateral condyle.
