The patient should be taken to the hospital as soon as possible. This is best done not in a regular car, but in a special vehicle. If you suspect a dislocation, the first thing you should do is call an ambulance. While waiting for the ambulance to arrive, you can place an ice pack or a cloth soaked in cold water on the joint.

- contortion
- When should you see a doctor?
- Anatomical features of the kneecap
- Causes of Dislocation
- symptoms of dislocation
- Causes of Dislocations
- Symptoms of injury: pain and functional limitations
- restoration of joint integrity
- shin dislocations
- dislocation of the kneecap
- Types of Dislocation
- Clinical signs of joint dislocation
- Treatment of chronic and complicated hip dislocations
- Hip dislocation in children
contortion
A dislocation is a sudden shift in the joint position of a bone. The injured person feels a sharp pain in the affected area and may notice a change in the shape of the area.
Depending on the type of injury, whether it's a hip dislocation, a leg dislocation, or a shoulder dislocation, the symptoms of the problem can vary. For example, a similar hip problem at birth often results in an abnormal gait and posture, and one leg may even be shorter than the other.
However, there are general symptoms of a dislocation that may indicate that a body part has become dislocated:
- reddening of the skin on the affected area;
- Severe pain that increases when moving the dislocated limb;
- An external change in the shape or size of the joint;
- Increased swelling of the affected area;
- loss of feeling in the limb (nerve endings may be affected by this symptom);
- difficulties in performing motor activities;
- Elevated body temperature, high fever and chills.
When should you see a doctor?

If you suspect a hip or dislocated hip, you should seek professional medical help immediately. Otherwise, you risk exacerbating an already injured joint.
In the event of a dislocation, first aid should be provided. Immediately rest the joint and apply a cooling compress to reduce swelling. If the injured person is in unbearable pain, they should be given painkillers. The injured person should then be taken to a hospital for proper medical care by an experienced trauma surgeon.
At AO Medycyna (Klinikum Academik Roitberg), specialists with many years of qualifications and extensive experience are available to admit patients at any time. The multifunctional medical facility is located in the center of Moscow, on 10, 2nd Tverskaya-Yamskaya Avenue, near the Mayakovskaya, Beloruska, Tverskaya, Novoslobodskaya and Chekhov metro stations.
Anatomical features of the kneecap
The knee joint is one of the largest and most important joints in the human body. It consists of the femur, tibia and kneecap.
The patella (better known as kneecap) is a small bone located at the front and top of the knee. Their main task is to protect the knee joint from injuries and consequential damage.
The knee joint has many important functions. Without it, humans would not be able to at least stand, walk, or bend or straighten their legs.
As previously mentioned, a dislocated kneecap is an injury in which the relationship between the bones is abnormal. This dislocation is caused by hard impacts and other unfavorable factors. Read more about this below.
Causes of Dislocation
A dislocation can be caused by many different factors and a complex combination of factors. Some of the most commonly diagnosed causes of a dislocation are.
- trauma of any kind;
- Careless jumping, sudden sharp turns of the knee;
- Excessive stress on the ligaments, which can cause them to tear;
- low muscle strength in the legs;
- Abnormal structure of the lower limbs.
If any of the above triggers are present, the patient should pay special attention to preventive measures (which will be described later in this article) and try to protect the knee from injury as much as possible.
symptoms of dislocation

The symptoms of a dislocation depend on the type of dislocation. For example, a congenital dislocation of the hip is associated with gait disorders because abduction is limited, the gluteal folds are asymmetrical, and one leg is shorter than the other, leading to a limp. With a hip dislocation on both sides, the gait becomes a 'duck'.
A congenital dislocation of the knee joint is associated with severe pain, gait disorders, inflammation and stiffness. Traumatic dislocations result in swelling, stiffness, and pain in the joint.
However, if we speak of general symptoms, the following are observed.
- There is redness in the area of \u200b\u200bthe injured joint;
- severe pain that increases with every movement of the limb;
- A visual deformation of the joint is noted, since the dislocation not only changes the size of the joint, but also its shape;
- There is severe swelling in the area of the dislocation;
- Some people lose feeling in their limbs (nerve damage);
- impairment of motor function;
- Fever;
- Fever followed by chills, etc.
Causes of Dislocations
Most dislocations are caused by indirect trauma, meaning they are more likely to occur when the injury site is far from the injured joint. For example, a fall on an outstretched arm can cause a dislocated shoulder joint. A traumatic dislocation can also occur with sudden movements that exceed the joint's normal range of motion. Dislocations caused by direct trauma to the joint are much less common.
Many people are diagnosed with a dislocated joint as a result of a medical condition, such as an illness:
This type of joint injury can be not only acquired, but also congenital, as a result of malformation of the musculoskeletal system during fetal development.
Symptoms of injury: pain and functional limitations
The most noticeable symptom of a dislocation is a cracking or popping sound followed by a stabbing pain. This pain is localized directly at the site of injury. The pain is accompanied by tissue swelling, the limb looks unnatural, and the surrounding tissues may lose sensitivity. Because of the pain and the altered position of the bones, movement of the limb is severely restricted or impossible, and any attempt to move the limb increases the pain. A gradual feeling of goosebumps, paleness of the skin and bruising due to damage to the blood vessels are also typical. Depending on the site of the injury, other symptoms may also occur.

The dislocation is usually closed without tearing the skin or tissue overlying the dislocation. The swelling of the tissue is quite pronounced and the joint is immobilized. Open dislocations with ligament and muscle tears, skin injuries, wound formation and severe swelling of the surrounding tissue as well as bleeding are possible.
- Dislocations with complications in the form of intra- or extra-articular bone fractures and damage to muscle fibers, nerves or large blood vessels can occur. Paralytic dislocations lead to nerve damage and paralysis of the limb.
- A special variant is the habitual dislocation, which always affects the same joint due to a weakening of the ligaments. It can occur with light impacts, the swelling of the surrounding tissue is minimal and self-healing is possible.
restoration of joint integrity
Typical joint deformities, pain, tissue swelling, and impaired motor function caused by trauma or other injury form the basis for the diagnosis. To determine the nature of the injury, radiographs of the injured area should be taken from multiple angles to exclude associated fractures.
The dislocation should be reduced to bring the joint back to its natural position. However, this should only be done by a doctor after a thorough examination. Do not try to correct the dislocation on your own, use self-medication, compresses and various external and internal drugs. Immediately after the dislocation, the joint should be secured with a fixation bandage, a cold compress placed on the injured area and taken to the trauma ward.
In the hospital, the affected joint is first anesthetized by the doctor and then pushed back as far as possible. An immobilizing bandage is then applied to allow the injured joint to rest. Complex sprains may require surgical intervention to restore the integrity of all affected structures (ligaments, blood vessels, muscles).
The surgeon or traumatologist provides further treatment and monitoring of the patient, and in case of severe pain, painkillers, massage, exercises and physiotherapy treatment are prescribed. Surgical treatment is often used for permanent dislocations or chronic injuries. If you don't intervene or try to self-medicate, you can cause even more damage to the limb, which can lead to osteoarthritis, bone head necrosis or intra-articular fractures, ligament or vascular and nerve damage (which can lead to limb paralysis).
shin dislocations
A tibial torsion is essentially a tibial dislocation because the fibula is not part of the knee joint. At the time of dislocation, the tibia can move in different directions (forward, backward, lateral) depending on the mechanogenesis of the injury. Anterior tibial dislocation occurs most commonly with indirect trauma, when a person falls onto a hyperextended leg at the knee. Significant vertical force causes further hyperextension, stretching and tearing the capsule and ligaments of the knee and displacing the articular end of the femur posteriorly.
An anterior tibial location is less likely because of a sudden force on the posterior surface of the tibia when the leg is extended or flexed. In the posterior tibial location, the mechanism of injury is reversed. It mainly occurs when the tibia is flexed up to 90°. If the force acts in an anteroposterior direction on the tibia, a purely anterior or posterior dislocation is rarely present. There is usually an anterolateral or posterolateral dislocation of the tibia.
An anterior tibial dislocation can result in stress damage to the fibular nerve, while a posterior dislocation can damage the popliteal vessels. With a posterior dislocation of the joint edge, the tibia retracts and pinches the neurovascular bundle, sometimes even partially tearing the inner sheath or the entire popliteal artery.
Symptoms of a tibial dislocationPain, typical deformation and dysfunction of the knee joint. The limb is in a constrained posture, most often in an upright position, and is bayonet-shaped. An anterior dislocation shows a deepening of the tissue over the kneecap with an increase in the knee articular surface.
On palpation, the patella is mobile in an anterior dislocation and immobile in a posterior dislocation. Also, the direction of displacement of the articular ends of the bones, the fluctuation of the hematoma, etc. is noted. The diagnosis is clarified radiologically in two projections.
There are cases when the tibia repairs itself on the basis of mutual help, and then there are difficulties in diagnosing the nature of the knee joint injury. In these cases, only the symptoms of hemarthrosis and ligament insufficiency predominate. Contrast-enhanced arthrography is performed to determine the extent of the tear in the joint capsule. In the case of circulatory disorders or if the pulsation of the popliteal artery is questionable, a contrast-enhanced vasography or a vascular revision is indicated. Failure to detect popliteal artery damage or thrombosis following a dislocation will result in necrosis and lower extremity amputation.
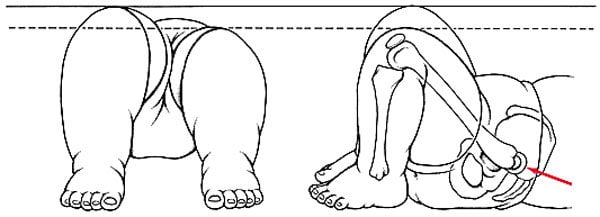
dislocation of the kneecap
Kneecap dislocation is extremely rare (0.5 %). The mechanism is different; generally it is caused by direct trauma. When a ligament is torn, the kneecap moves up, the quadriceps tendon moves down the kneecap, and the lateral aponeurosis moves laterally.
A contributing factor to patellar luxation is dysplasia of one of the condyles of the femur and a valgus or varus deformity of the knee joint.
When a patient presents with a dislocated kneecap, the diagnosis is not difficult. The position of the kneecap, the local pain, the forced half-flexed position of the limb and the loss of function are determined by visual inspection and palpation. If the patella retracts spontaneously during a lateral dislocation, the dislocation is usually not diagnosed and the patient is treated for a contusion or hemarthrosis of the knee joint that results in habitual patellar dislocation.
Treatment. Under anesthesia and with relaxed muscles, the kneecap can be easily brought back into its normal position by applying pressure with your fingers. The severed leg is then placed in a plaster cast for 3 weeks. One month after the injury, the leg can be used again. Patients with vertical and normal dislocation of the kneecap are treated surgically - ligaments or tendons are sewn to the kneecap.
Types of Dislocation
According to the classification, two types of dislocations are distinguished:
- Acute – occurs at the time of injury, which is clearly marked;
- Chronic (habitual) – this is a recurring dislocation that develops joint instability.
According to the localization, the following types of dislocations can be distinguished:
- Hand and upper limb dislocations – collarbone, shoulder joint, elbow and hand, fingers;
- Dislocations of the lower limbs – hip joint (hip dislocation), knee joint, kneecap (patella), ankle joint (with ankle involvement), foot;
- cranial dislocations affecting the lower jaw (temporomandibular joint dislocation);
- vertebral dislocations.
Clinical signs of joint dislocation
The clinical signs of a dislocation can be as follows
- severe pain in the injured area;
- swelling of soft tissues;
- bleeding into the skin and subcutaneous tissue (bruising);
- visually noticeable disruption of the shape of the joint
- inability to perform voluntary movements in the joint;
- restriction of passive movements and a springy feeling;
- Cracking noise at the time of injury
- Pallor and cooling of the skin below the injured joint (persistent and caused by pressure on the supplying arteries)
- Numbness of the skin and paresthesia (these symptoms are also not permanent and are related to the compression of the main nerve trunk).
Treatment of chronic and complicated hip dislocations
If medical personnel cannot repair the dislocation using a closed procedure, an open reduction of the hip dislocation is attempted. During surgery, the doctor makes an incision to gain access to the joint. He manually repositions the femoral head and stitches the wound. Torn ligaments, massive soft tissue injuries and long-lasting dislocations also require an operation.
Even timely and appropriate treatment of injuries does not always result in a full recovery. In some patients, damage to the articular cartilage can cause deforming osteoarthritis to develop over time. This disease causes severe pain when walking and hip deformity. The only way to fix the problem is to replace the joint with an artificial joint replacement.
Hip dislocation in children
Hip dysplasia is a very common musculoskeletal pathology in children, accounting for about 3 % of all orthopedic diseases. It is caused by abnormal formation of the joint during the fetal period. Statistically, unilateral dislocations are seven times more common than bilateral dislocations and are five times more common in girls than in boys.
50 % of all cases of hip dysplasia occur in infants born in the tummy route. The type of obstetric care and the mechanism of delivery itself, on the contrary, do not affect the occurrence of the pathology. This is confirmed by the presence of hip deformities in children born by cesarean section.
The group of hip dysplasias in children includes the anteversion of the hip, the subluxation, the dislocation and the radiographically immature hip. The disease is usually diagnosed in early childhood during a routine examination by a pediatrician and orthopedist. Sometimes the pathology is diagnosed much later, when the child begins to walk.
Traumatologist of the highest category Sumin AI:
- Visible shortening of the affected limb;
- Asymmetric position of the buttocks, thighs and popliteal creases;
- external rotation of the limbs, especially noticeable during sleep;
- Characteristic crunching in the leg;
- inability to straighten the limb bent at the hip more than 70-90 degrees;
- Displacement of the femoral head on palpation.
In children older than 1 year, the congenital anomaly manifests itself as an unsteady gait and limping. The child has a curvature of the lumbar spine. Sick children usually start walking later than healthy children.
The treatment of hip dislocations and subluxations in children begins in the first few weeks of life. To combat pathology, wide wings, pavlik stirrups and special therapeutic splints are used. In parallel, the child is prescribed physiotherapy, massage and therapeutic exercises. If conservative therapy fails, open reduction with arthroplasty is performed.
Read more:- Diagram of a joint with and without a dislocation.
- Dislocation of a bone in a joint.
- How do you treat a sprained ankle?.
- The lateral dislocation is.
- Sprained or dislocated ankle how to identify.
- Treated subluxation of the ankle.
- tearing of the joint capsule.
- Torn ligaments in leg.
