Interestingly, when you search for these two terms in various even authoritative dictionaries, you will find that some of them do not refer to the leg, but only to the forearm (e.g.: Pronunciation: in medicine, the movement of the forearm in which the palm of the hand is brought up to the back of the hand... Treccani online dictionary ); most likely it is a purely sporting allusion, based on an analogy to the movement of the hand; unfortunately, dictionaries and encyclopedias have made little progress in updating the...
- biomechanics of the shoulder
- Static structures and mechanoreceptors
- Pronation of the foot - pronation of the foot
- types of
- Neutral pronation
- overpronation
- The most important movements and functions of the round pronator.
- The muscle and adjacent landmarks (muscle topography).
- Diagnostic tests for the round pronator.
- Variations of exercises for the pronator quadratus.
- Diagnosis of forearm muscle pain
- Treatment of muscle pain in the forearm
- Neutral pronation
- hypopronation
- neuron
- peripheral nerves
- Motor fibers (neurons)
- shoulder and forearm
- forearm muscles
- Human Forearm Muscles Anatomy Information:
- Which doctors should you visit for an examination of the forearm muscles:
- Pronation and supination: what does it mean?
- Peculiarities of gait and footwear
- overpronation
- Excessive supination
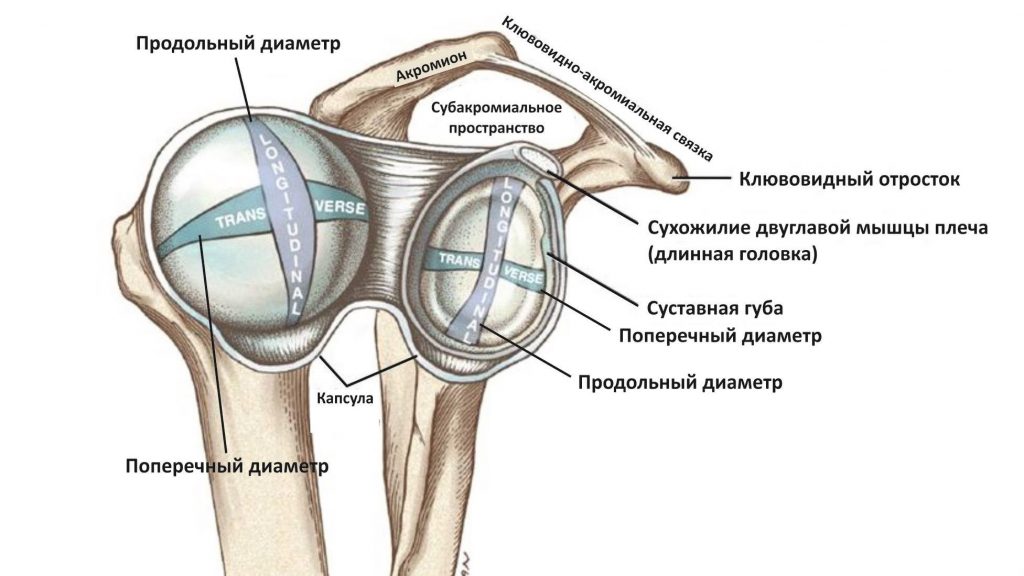
biomechanics of the shoulder
The shoulder region is known to be one of the most difficult regions to assess and rehabilitate. Because of the numerous joints involved in the movement of the shoulder, the term 'shoulder complex' is appropriate. In order to effectively rehabilitate shoulder injuries, one must understand the functional anatomy that underlies the biomechanics of the shoulder complex.
The shoulder complex consists of 3 physiological joints and one 'floating' joint:
When assessing the shoulder-clavicular joint, the contribution of the sternoclavicular and rib-vertebral joints should also be considered.
The LHS is the only point of attachment of the upper limbs to the axial skeleton. The LGS involves a sliding movement of the scapula along the trunk and does not involve bony fixation. The PLS is of particular interest in understanding the mechanism of shoulder joint injuries because of its osteological predisposition to instability.
The shoulder joint is formed by the humeral head (convex surface) and the socket of the scapula (concave surface). Due to the relatively large surface area of the humeral head in relation to the acetabulum, this joint has limited bony congruence and is therefore highly dependent on the surrounding soft tissues, which do not provide adequate structural support.
In addition, it was calculated that only 25 % of the surface of the humeral head articulates with the glenoid cavity. The surrounding passive structures (labrum, joint capsule, and ligaments) and active structures (muscles and associated tendons) work together to maintain the dynamic stability of the PLS.
- Rotation (flexion and extension).
- Sliding down (during adduction).
- Gliding upwards (with adduction).
- Backward slide (during internal rotation).
- Gliding forward (during external rotation).
Static structures and mechanoreceptors
In addition to the intricate network of ligamentous structures that connect adjacent bones, the importance of the surrounding musculature cannot be overstated. Active muscle contractions are essential to maintaining stability in the shoulder complex.
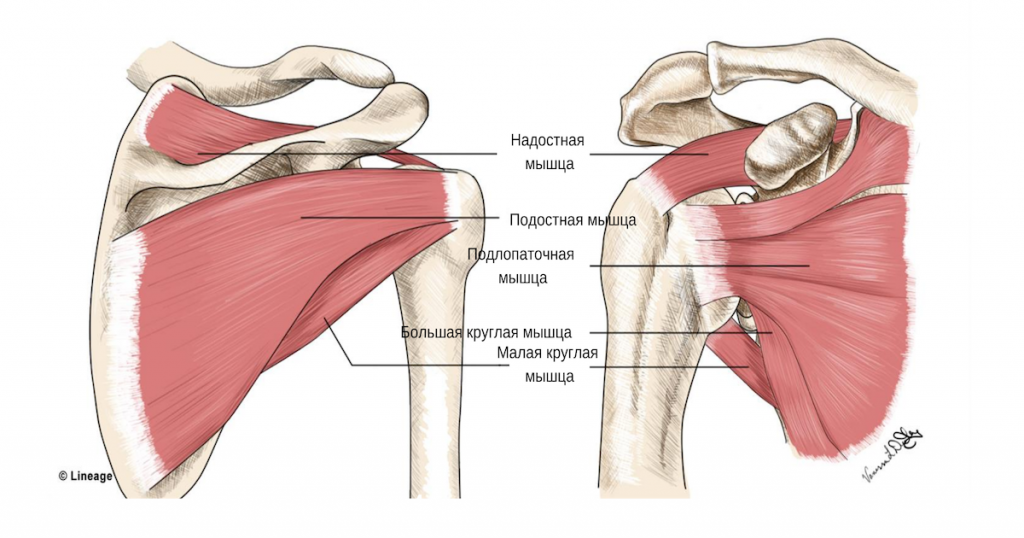
The muscles of the shoulder complex can be divided into global shoulder motors and finely tuned stabilizers of the individual joints. Larger muscles such as the trapezius, scapula, pectoralis major, deltoid, serratus, dorsalis, rhomboid, sphincter greater, biceps, pectoralis major, and The triceps are responsible for a variety of shoulder movements. They provide the gross movements of the upper quadrant.
The shoulder-stabilizing muscles, the supraspinatus, glenoid, subscapularis, and popliteus, are part of the rotator cuff muscles and insert at the humeral head in the humeral fossa. Together they act as dynamic stabilizers of the PLS joint, maintaining the central position of the humeral head in the joint fossa under both static and dynamic conditions. It has been suggested that the tendons of the rotator cuff muscles are connected to the ligaments and synovial membrane, so contraction of these muscles may provide additional stabilization of the PLS by strengthening static structures during movement.
Synchronized contractions of the rotator cuff muscles center the humeral head during movement. This avoids physical damage to the tissues (located primarily anterior and superior to the PLS) associated with shoulder injuries and pain. As previously mentioned, due to their anatomical location in the subacromial space, the rotator cuff tendons are particularly susceptible to compression, abnormal friction, and eventual entrapment during active activities. Proper alignment of the humeral head is important for proper PPS movement and daily activities.
Pronation of the foot - pronation of the foot
Pronation is a natural movement of the foot that occurs when the foot strikes the ground while running or walking. It consists of three cardinal plane components: subtalar extension, ankle dorsiflexion, and forefoot abduction; these three different movements of the foot take place simultaneously during the pronation phase. Pronation is a normal, desirable, and necessary part of the gait cycle. Pronation is the first half of the stance phase, while supination initiates the progression phase as the heel begins to lift off the ground.

Illustration of the pronation and supination of the foot from an anatomy textbook
- 1 types
- 1.1 Neutral pronation
- 1.2 Excessive pronation
- 1.2.1 Causes
- 1.2.2 Consequences
- 1.2.3 Prevention / Treatment
- 1.2.3.1 Orthopedic measures
- 1.2.3.2 Type of footwear
- 1.2.3.3 Tape
- 1.2.3.4 Shoe lacing
- 1.2.3.5 Barefoot Walking
types of
The normal biomechanics of the foot absorb and control events throughout the gait cycle, with the foot being flexible (pronation) and rigid (supination) at different stages of the gait cycle. Plantar eversion, ankle dorsiflexion, and forefoot abduction occur when weight is applied to the foot. Pronation should not occur after the last stages of midfoot alignment, as the normal foot must then supine in preparation for pronation.
Abnormal pronation occurs when the foot bottoms out when it should be supinating, or excessive pronation during the normal phase of pronation. About four degrees of pronation and supination are required for the foot to move forward correctly. In the neutral position, the foot is neither pronated nor supinated. If the foot pronates or supines during the support phase of the gait cycle when it should be in the neutral position, there may be a biomechanical problem.
To simplify the selection of corrective shoes, three types of pronation are distinguished: neutral pronation, overpronation and underpronation.
Neutral pronation
Some pronation, also known as eversion, is natural with normal body movement. Neutral pronation is when the foot experiences normal, healthy pronation rather than excessive or insufficient pronation. With a healthy movement, a larger area of the toes is involved in the push-off than with an unhealthy movement. In neutral pronation, body weight is distributed relatively evenly across all toes, with slightly more loading on the big toe and second toe, which are better able to carry heavier loads.
overpronation

overpronation
People who overpronate tend to push off almost exclusively from the big toe and second toe. As a result, the footprint is not evenly distributed across the foot and the ankle has difficulty stabilizing the rest of the body. It also creates an unnatural angle between the foot and ankle, and the foot sticks out unnaturally. Even people with normal pronation often have an angle between the foot and ankle, but it's not as great as in people who buckle too quickly. With normal pronation, the weight of the body is evenly distributed throughout the foot.
The most important movements and functions of the round pronator.
- Elbow Flexion - is the auxiliary muscle in this movement;
- Pronation of the forearm – pulls the radius inward so that its head rotates around the proximal part of the ulna at the proximal joint of the radius bone.
The muscle and adjacent landmarks (muscle topography).
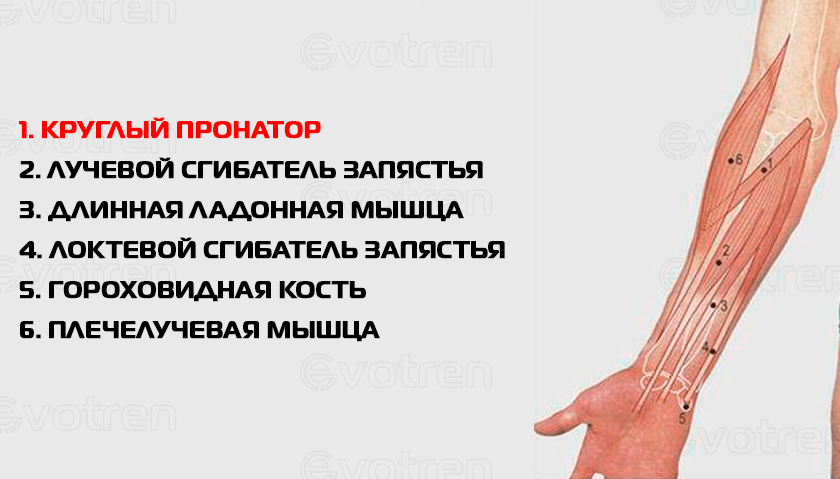
The peripheral pronator is overlaid by the aponeurosis of the biceps brachioradialis muscle and the brachioradialis muscle.
At the same time, it partially overlays the radial flexor of the wrist.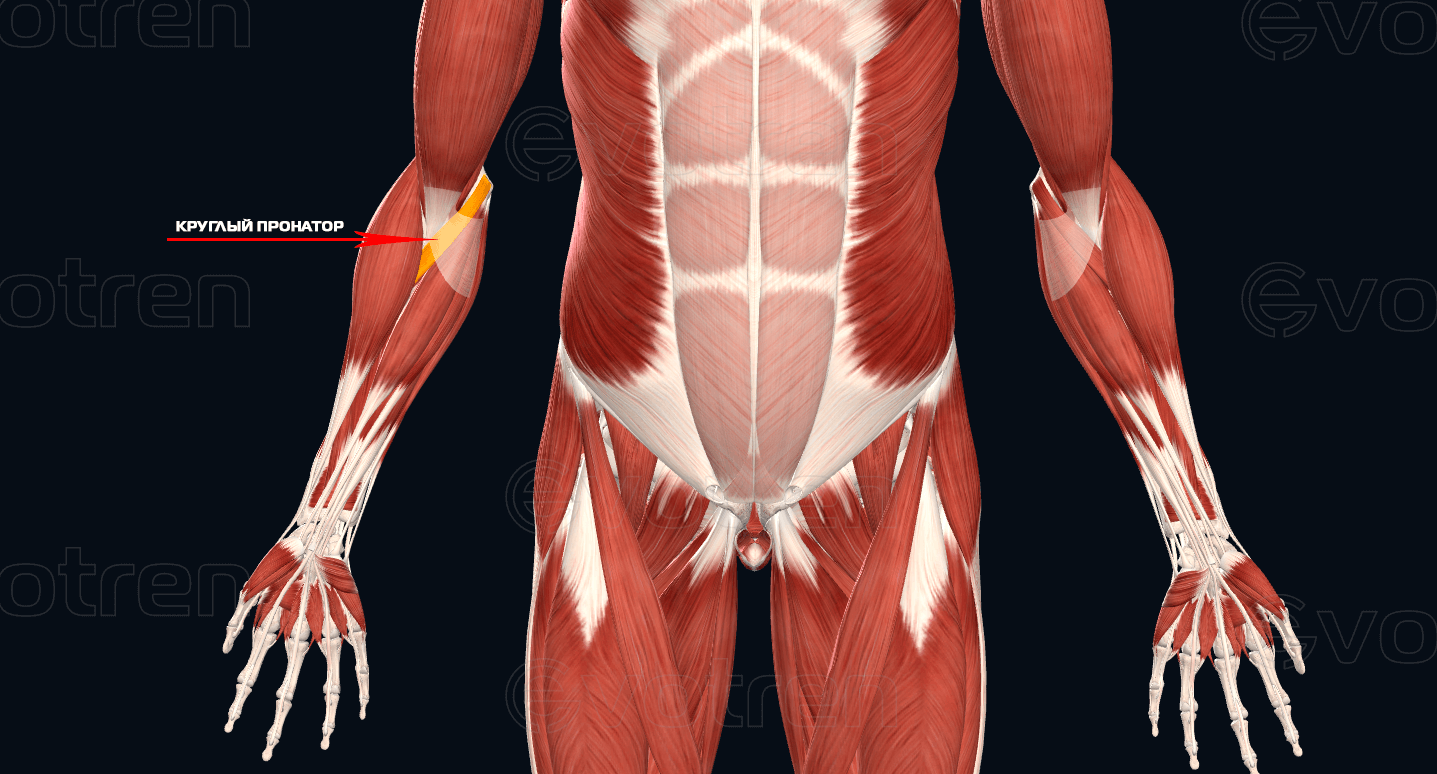
Diagnostic tests for the round pronator.
The video below shows a variation of the chiropractic muscle test to analyze the round pronator.
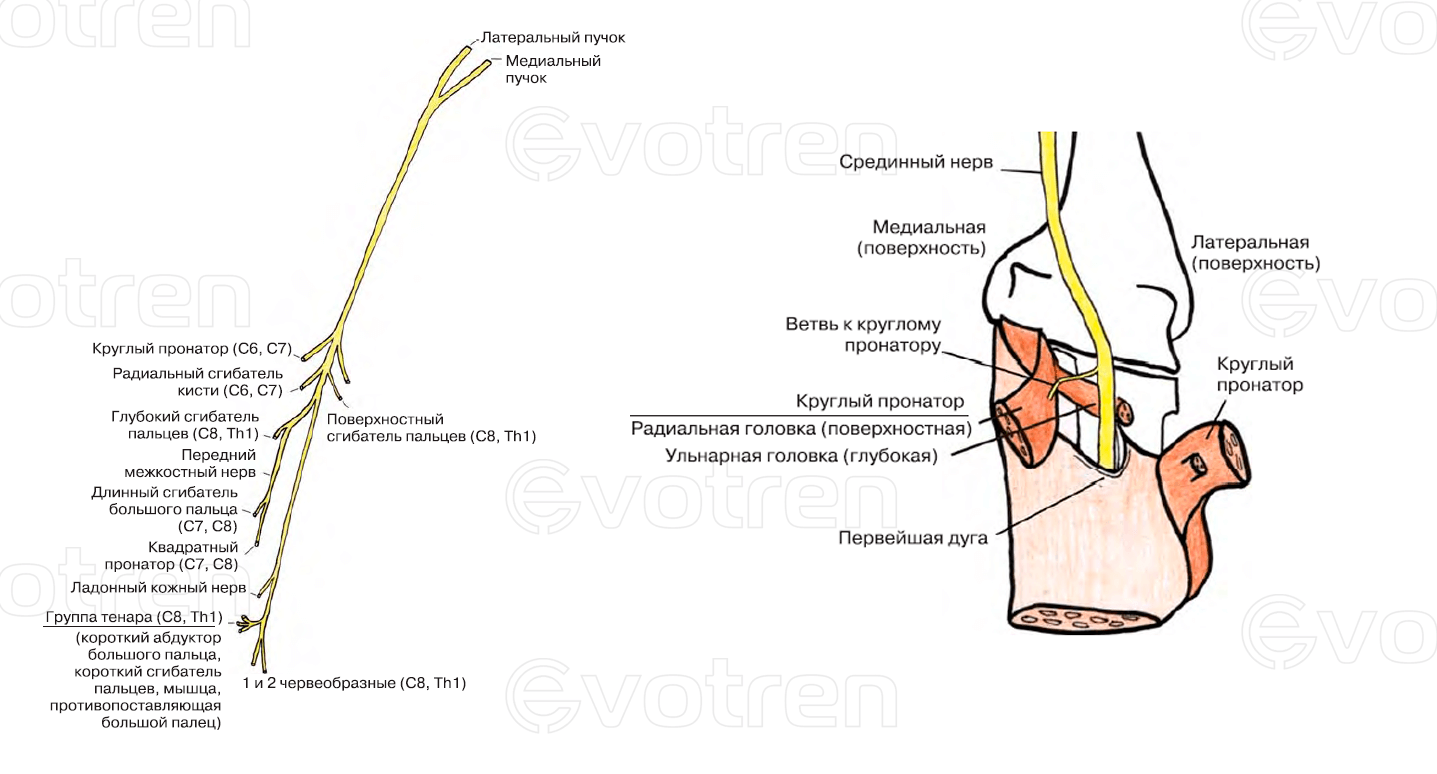
Symptoms:
- pain in the projection of the round pronator;
- Nausea and pain in the declining fingers, thumb, index finger, middle finger and half of the ring finger;
- Paresis (neurological weakness and atrophy):
—- Muscles directly innervated from the median nerve to the origin of the anterior intercostal nerve:
- radial flexors of the hand (m. Flexor carpi radialis);
- M. palmaris longus (M. palmaris longus);
- Superficial finger flexor (m. Flexor digitorum superficialis)
—- Muscles innervated by the anterior interosseous nerve (N. interosseus anterior):
- deep flexor muscle of second and third toe (m. Flexor digitorum profundus II and III);
- long flexor muscle of the thumb (m. long finger flexor (flexor pollicis longus));
- Pronator quadratus (m. pronator quadratus);
Variations of exercises for the pronator quadratus.
Starting position: standing. The forearm is bent at the elbow joint. We take a rubber band, attached at one end to a wall bar or other stable support, perpendicular to the forearm and parallel to the floor. Then we turn the hand inward, as if wrapping the rubber band around the fist. The round pronator performs a concentric contraction. Slowly return to the starting position. During this phase, the round pronator works in an eccentric position.
A similar variation can be done with a block trainer. The starting position is standing. The forearm is strongly flexed at an angle of less than 90 degrees against the humerus. Place your shoulder and elbow sideways against a firm surface. For example on the back of a standing bench. Lock the device to the top and side of the working arm. Hold the grip and rotate it evenly while simultaneously bending and pronating your wrist. The circular pronator works in concentric mode. As you return to the starting position, work eccentrically.
Starting position: standing. The forearm is bent at an angle of about 90 degrees or slightly less. The elbow can rest against the body. The wrist grips a strap or strong band, at the end of which a moderate weight (pancake, weight) is attached. The hand is directed upwards, ie in a supinated position. A penetrating motion is then made with the hand, causing the band to wrap around the fist like a fist and lifting the weight vertically upwards. The pronator is circular and again performs a concentric contraction. Once under control, he works eccentrically.
The starting position is the forearm, with the entire elbow resting on a horizontal surface (pliobox, bench, table). A small weight can be used as a device by turning it upside down. This can also be a dumbbell with one-sided plates or a barbell. Grasp the handle of the inverted kettlebell, dumbbell, or body bar at one end and stand in an upright position, leaning outward against your full fall. The hand is supinated and the circular pronator is forced to work in an eccentric phase. When the projectile returns to its original (vertical) position, the circular pronator contracts concentrically.
This exercise can be performed in a more complicated version, if the device is moved to both sides. In this case, the pronators and supinators work sequentially and alternately.Diagnosis of forearm muscle pain
Due to the non-specificity of the symptoms, the diagnosis of forearm muscle pain must primarily be made through differential diagnosis. A traumatic injury to the arm—dislocation, fracture—is the easiest to diagnose because the symptoms are obvious and X-rays confirm the injury.
Unfortunately, there is no diagnostic standard for the forearm, no 'red flag pain system', so the doctor has to rely on his own experience and use all possibilities to determine the cause of the symptom.
First of all, cardiovascular disease - angina pectoris, myocardial infarction - is excluded, especially if the patient complains of pain in the left arm. In addition, a radicular syndrome must be ruled out or confirmed, in which the forearm pain may be secondary.
The most important examination methods in the diagnosis of forearm pain are as follows:
- Questioning of the patient, including inquiring about triggering occupational factors, in order to determine a possible radicular syndrome. In addition, the characteristics of the pain - intensity, sensation, location, duration, dependence on postural changes and arm movements noticed by the patient - are examined.
- Visual inspection of the patient's upper body, examining not only the painful forearm but also the other arm.
- Assessment and examination of the neurological condition, palpation of the sore arm, spinal sections.
- Examination of rotational movements – at the elbow and wrist.
- X-ray examination of the spine. Examination of the cervical spine with functional tests.
- To clarify the diagnosis, a CT or MRI scan may be ordered to determine the nature of the compression lesions (hernia, protrusion).
- Electromyography, which examines the bioelectric potential of muscle tissue and its conductivity (speed of pain signal conduction).
The diagnosis of forearm muscle pain directly depends on the clinical symptoms and their specificity. Therefore, the doctor often performs various motor tests that are particularly effective in detecting tunnel syndrome, epicondylitis, tendinitis, and rheumatic joint diseases.
Treatment of muscle pain in the forearm
Usually, forearm pain caused by a simple strain after exercise or a single physical activity goes away spontaneously and without medical intervention. However, more serious diseases often go undetected for a long time and are therefore not treated appropriately. This greatly complicates the management of myalgia because once the symptom is relieved, the pain diminishes and the condition becomes chronic.
Usually, the patient presents to the health center when the symptom worsens, so the doctor's first job is to treat the pain.
Forearm muscle pain treatment, standard steps:
- Pain treatment with various options, from local anesthesia to local anesthesia through injections.
- Local corticosteroid injections into trigger points (in MFBS – myofascial syndrome) are possible.
- immobilisation of the arm. The forearm is immobilized, less often orthoses, bandages, splints and bandages are used. Splinting is only carried out if there is a corresponding indication.
- Non-steroidal anti-inflammatory drugs can be prescribed only if there are signs of an inflammatory process - purulent tendinitis, myositis, phlegmon, etc.
- Prescribing myorelaxants to relieve spasms.
- Massage with warming or anesthetic drugs.
- applied therapy.
- Use of local physiotherapeutic treatments, usually electrophoresis.
- kinesitherapy.
- Operations are rarely performed, only with neoplastic processes, fractures with displacement, tendon and muscle tears.
Rehabilitation measures such as therapeutic exercises are not suitable for the forearm, rather its injuries are treated with immobilization and measures to eliminate the etiological cause of the pain.
Neutral pronation
The foot is turned inward by about 15 % and is in full contact with the ground, allowing it to easily support body weight. The arch of the foot ensures optimal distribution of the impact load on the ground. At the end of the run, the entire forefoot is pushed off evenly.
One of the most common forms of pronation. Hyperpronation is a trait you have, and as you get older, you become more susceptible to a number of sports injuries due to this trait.
Hyperpronation is excessive flattening or inward rolling of the foot, which reduces the longitudinal arch of the foot. Excessive pronation is bad for cushioning. The ligaments are constantly in a tense, stretched position.
The running cycle starts with landing on the inside of the heel. The foot flexes inward more than the ideal 15 %. The foot and ankle are in constant discomfort as the body stabilizes and cushioning is less effective. The big toe and second toe in particular push off in the last phase of the stride. You carry the greatest burden. Overpronation leads to extra strain, muscle strain, and dangerous side effects.
In dorsiflexion, the ankle, knee, and hip rotate inward medially. Hyperpronation is excessive pronation. This increases the load on the musculoskeletal system. Excessive movement of the foot leads to calluses on the big toe and lateral bony surface and injuries - runner's knee, medial tibial syndrome, plantar fasciitis and Achilles tendinitis.
A customized orthopedic insole can help ensure that you no longer have any discomfort when running or walking. However, it is important to remember that only a combination of these measures can solve the problem. You need to be aware that while pronation can influence some injuries, it is not the sole factor in causing them.
hypopronation
The most important feature of hypopronation is the lack of foot deviation. The foot is tilted outwards at the ankle. The impact load is not distributed efficiently enough and the musculoskeletal system suffers. The main burden rests on the little toes. The trainee wears himself out unnecessarily on the outside.
To prevent excessive supination, you should do additional stretching and strengthening exercises for the calf muscles, cameloids, hamstrings, and other leg muscles. Wearing the right running shoes and replacing worn shoes will also help prevent injuries. Choose running shoes with added medial support.
A range of therapeutic, holistic treatments can be used to prevent and treat foot problems. All exercises can be done at home. If you do them regularly, you will see a marked improvement.
Begin by warming up and stretching the calf muscles. First, stand on tiptoe, as high as you can, and walk on tiptoe for a few minutes without letting your heels touch the floor.
Then put your foot on the edge. This is a movement designed to correct a deformed foot. The ankle should be rotated in the opposite direction of the curve, with the toes pointing in. The exercise should last a few minutes and can be done with rest breaks.
The next step is to take a small object, e.g. B. a ball to take in hand. Place the ball between your knees and walk around in this position for a few minutes.
neuron
neuron – is the structural unit of our nervous system whose main function is to transmit information from one part of the body to another. To transmit information, the neuron is stimulated and then generates a nerve impulse. Neurons are also involved in processing and storing information. However, we will not cover this topic.

neuron – is a highly specialized cell. It consists of a body and a long process, the axon (Figure 1).
The axon can be up to a meter or more in length. The body contains many small branches - dendrites. Via these processors, a neuron receives information from other neurons and transmits it via the axon to another neuron or to the organ it controls (muscle in our case).
peripheral nerves
Skeletal muscles are supplied by one or more peripheral nerves. With a few exceptions (facial nerve and hyoid nerve), all peripheral nerves are mixed. A mixed peripheral nerve includes:
- motor fibers (neurons);
- sensory fibers (neurons);
- autonomic fibers (neurons).
When considering the structure of skeletal muscle, it was pointed out that the peripheral nerves have canals in the perimysium. Peripheral nerves reach the muscle fibers through these channels.
Motor fibers (neurons)
Motor neurons (motoneurons) transmit information from the CNS to the muscle. The bodies of motor neurons are located in the anterior horns of the spinal cord. The axons of the motor neurons reach the muscle as part of the peripheral nerve.
Motor neurons are divided into two types: α motor neurons (alpha motor neurons) and γ motor neurons (gamma motor neurons).
- α motor neurons innervate the muscle fibers. Impulses from the central nervous system (CNS) are transmitted to the muscle fiber via α-motor neurons and cause excitation (contraction) of the muscle fiber.
- γ motor neurons innervate the muscle spindles (muscle receptors). These motoneurons innervate specific muscle fibers (intrafusal) located within the muscle spindles. By tensing and relaxing the intrafusal fibers, the sensitivity of the receptor - the muscle spindle - is changed. This allows for more 'precise' control of movement. Swedish neurophysiologist Ragnar Granit was awarded the Nobel Prize for discovering this mechanism.
A α motor neuron innervates (i.e., branches) a large number of muscle fibers. Sometimes there are more than 2,000 muscle fibers per axon. Such a system, made up of a single neuron and the muscle fibers it innervates, is called a motor unit (MU). This concept was introduced to physiology by Nobel Prize winner Charles Scott Sherrington in the early 20th century. The specifics of the structure and function of the MU will be discussed later in this article.
shoulder and forearm
The common understanding of the position of the shoulders creates confusion from the very beginning of the study of human anatomy. What everyone is used to calling a shoulder is called the shoulder crown or shoulder girdle in medicine. So where is the shoulder and where is the forearm? The shoulder is the area of the upper extremity from the shoulder to the elbow joint, through which the upper arm bone is connected to the bones of the forearm.
The shoulder is connected to the radial bone via the lateral part of the articular surface, which is shaped like a sphere. This is the head of the humerus head. The shoulder blade (scapula) connects to the elbow from the medial part and forms the humeral block. The coronoid process and the ulnar process enter the block from the front and from the back, respectively. Above the pulley are the pits into which the processes enter when the elbow is flexed or extended.
forearm muscles
We have already established where the forearm is located in the human body. Now let's take a closer look at what muscles are involved in this part of the upper limbs. Depending on the movements performed, the muscles of the forearm can be divided into:
- Supinators: They allow the bar to move outwards;
- Flexors and extensors of the fingers.
- Pronators: They move the bar inwards;
- flexors and extensors of the fingers;
These muscle groups fall into two main categories based on their location: anterior and posterior.
Human Forearm Muscles Anatomy Information:
In terms of function. forearm muscles. The muscles of the forearm are divided into flexors and extensors, with some flexing and extending the entire hand and others straightening and lengthening the fingers. In addition, there are pronators and supinators, which cause corresponding movements of the radius bone. All of these muscles are divided into two groups based on their location: the anterior, consisting of flexors and pronators, and the posterior, consisting of extensors and supinators. Each group consists of a superficial layer and a deep layer.

The superficial layer of the anterior group originates from the medial epicondyle of the humerus, the same layer of the posterior group originates from the lateral epicondyle.

The main part of the deep layer of both groups is not attached to the epicondyle, but originates from the forearm bone and the intercostal membrane. The terminal insertions of the flexors and extensors of the hand are at the base of the metacarpal, and the same muscles attach to the phalanges of the fingers, except for the long extensor of the thumb, which inserts at the first metacarpal. The pronators and supinators attach to the radius bone. The muscles of the forearm are made up of fleshy portions near the shoulder, while merging into long tendons near the hand, giving the forearm the shape of a cone that is flattened front to back.

Which doctors should you visit for an examination of the forearm muscles:
Are you worried about anything? Would you like to learn more about your forearm muscles or have an examination carried out? You can. make an appointment with your doctor – Clinic Eurolaboratory is always there for you! The best doctors will examine you, advise you, provide the necessary care and diagnose the problem. You can also doctor at home. clinic Eurolaboratory is open for you around the clock.
How to contact the clinic:
The phone number of our clinic in Kiev is: (+38 044) 206-20-00 (multichannel). The clinic secretariat will find a suitable day and time for you to visit the doctor. Our coordinates and directions can be found here. For more information about all of the clinic's services, visit their own website.If you have been examined before Bring the results with you to your doctor for a consultation. If you have not yet had any examinations carried out, we will carry out the necessary work in our clinic or with our colleagues in other clinics.
It is important that you take a very close look at your general health. There are many diseases that do not manifest themselves in our body at first, but, unfortunately, are treated too late. It is enough if you go to the doctor several times a year to be examined by a doctor several times a yearnot only to prevent a bad illness, but also to keep the body and the organism as a whole healthy.
If you want to see a doctor, you can find and read answers to your questions on the Internet Self Care Tips. If you are interested in opinions about clinics and doctors, try to find the information you need on a forum. You can also go to the medical portal EurocoolSign up to keep up to date with the latest forearm muscle news and information, sent automatically to your inbox.
Pronation and supination: what does it mean?
Let's take a look at some of the terms used by kinesiologists and their explanations. Rotation, pronation and supination are types of movement of limbs and shoulder joints in kinesiology.
Pronation is an inward twisting motion of the upper or lower limbs. This can involve movement of the hand, forearm, and humerus. It can also involve movement of the foot, shinbone, or hipbone.
Let's take the arm as an example. Extending your arm forward so your thumb is up and then rotating your arm inward 90 degrees so your hand is level is called pronation. This type of twist is performed by a muscle group called the pronators.
Supination is performed in the same way by the supinator muscles. Only in this case the side edge is turned outwards (rotated) in the opposite direction.
Let's take a closer look at what it is - pronation of the foot? Regardless of this, the foot can also be pronated. In this case, it is necessary to turn it by lowering the medial part (inwards, towards the central axis line of the body). This activates the pronator muscles of the lower limbs. When the foot pronates, the long and short fibula muscles are engaged.
In supination, the lateral portion of the foot is rotated outward (away from the midline of the body) with the lower or upper limbs. The principle is the same as in pronation, except that the movement is in the opposite direction. It's performed by the supinator muscle group: the long thumb extensor and the tibialis anterior.
The supinated dumbbell raise is performed with the hand rotated outward. The supinators are trained: the short supinator and the biceps muscle of the arm (biceps). The bicep muscle gets stronger when the elbow is bent to 90 degrees. Forearm rotation in supination is performed, for example, when working with a screwdriver or turning on a faucet.
Raising the biceps in supination in this way works additional muscles and stabilizes and strengthens the forearm. This is especially important when arm wrestling.
Peculiarities of gait and footwear
Many people notice that some people walk with a clubfoot, ie they brace themselves poorly and their feet fall inwards. Or a 'Chaplin' gait indicates a weakness in the pronators. It should be noted that these muscle groups are antagonists. Antagonists are biomechanically opposite groups that balance each other out by keeping the limbs in a central position.
Pronation and supination affect the upper limbs and differ significantly from the same lower limb movements. This is due to the structure and mobility of the joint and tendon structures. There are three ways to position your foot when walking or running:
- Normal pronation. This is easily recognized by a footprint on wet sand or a wet foot on paper or the ground. The footprint is typically arched outwards. There is no depression in the sole of the foot, which should be understood as normal pronation of the foot.
- hyperpronation. In this case, the person stands with one foot inward, which is characteristic of flat feet. Such a foot is wide, has little flex, and the instep is minimal or non-existent. In this case, the sole of the shoe is worn on the inside (especially on the heel). The inward 'tilted' foot twists the rest of the leg in the chain, causing rotation of the knee joint and femur trochanter. This leads to signs of wear on the joint surfaces. A severe pronation of the foot is essentially a flat foot.
- hypopronation. This is a weakening of the pronators and an outward rotation of the foot. The gait of people with hypopronation is also peculiar: it's like throwing their socks out. The outside of the sole of the shoe disappears, especially the heel. The knee joint is also rotated, leading to pathology, and the femur is also slightly rotated outward.
People with pronation disorders should see a podiatrist or kinesiotherapist and find the best footwear for them. The sole should not be too thin and the heel should be reinforced and have a small heel. In the case of hypopronation, doctors often recommend wearing special orthoses and insoles called supinators.
overpronation
overpronation ( overpronation ) causes the foot to continue rotating after striking the ground instead of starting the pushing phase. This creates excessive tension in the foot, shin, and knee and can cause pain in those areas. People who walk this way experience excessive wear on the inside of the shoe, which tilts inward when standing on a flat surface. Knee joints and flat feet can cause this problem.
What can be done to correct excessive pronation? It is advisable to wear shoes with a straight shape or with a slightly emphasized curve. A special shoe that has high walking stability, with a high-density sole and other anti-perforation properties is ideal. The level of wear on the shoe should be checked to see if progress is being made. Since this abnormal parameter leads to muscle tension and stiffness, stretching treatment should be performed.
Excessive supination
Excessive supination (and Sweating) leads to insufficient rotation of the foot after striking the ground. This creates excessive tension in the foot and can cause iliopsoas syndrome, Achilles tendinitis, or plantar fasciitis.
Runners with very pronounced foot curvature and heavily strained Achilles tendons are prone to this problem. The shoes are increasingly worn outwards; when standing on a flat surface, they tilt outward.
To correct problems caused by excessive supination, shoes should be worn that are appropriate for the problem, perhaps even in a way that allows the foot more freedom of movement. The flexibility of the inner midsole area of the shoe is also important. Affected runners should do targeted stretching exercises for their calves, hamstrings, quadriceps, and lumbar spine.
- Pronator - what does that mean?.
- The pronator is in anatomy.
- pronator and supinator muscles.
- pronation and supination.
- What is pronation and supination?.
- pronator to.
- How to determine the type of pronation.
- pronation.

