The first step is a comprehensive anamnesis (medical history), the clarification of typical risk factors such as smoking, diabetes and a physical examination.
- Valgus deformity of the first toe
- signs
- indications.
- contraindications.
- Prevention of complications depending on the degree of amputation (disarticulation) of the lower limbs
- keywords
- COMMON APPROACHES FOR CHOOSING THE REDUCTION LEVEL
- Therapeutic gymnastics
- washing the foot
- AD * Related products
- Effects of amputation
- Postoperative treatment and prosthetics after disarticulation
- accompanying symptoms
- level of amputation
- Hand, elbow and shoulder amputations
- Leg, foot and lower leg amputations
- preservation of the amputation
- rehabilitation period
- species
- causes
- costs of the services.
- opinions of doctors
Valgus deformity of the first toe
Valgus deformity of the first toe – This is a condition in which the first toe deviates outward, the metatarsophalangeal joint of the first toe becomes arthritic, and the other toes become deformed.
Underlying the development of a valgus deformity of the first toe is a congenital weakness of the connective tissue that contributes to the development of transverse flatfoot. Other factors include obesity, endocrine disorders, osteoporosis and foot trauma. A key factor in the development of a valgus deformity of the first toe is uncomfortable footwear, including 'model shoes' with narrow toes and high heels.
signs
The valgus deformity of the first toe is expressed as follows:
There is a gradual outward deviation of the big toe as a result of progressive transverse flatfoot. The head of the first metatarsal has an exophthalmos often referred to as a 'bunion'. As the first toe deviates outward, the remaining toes (often toes 2 and 3) deform and are referred to as hammer toes because of the characteristic changes. The disease is associated with increasing leg fatigue, pain in the feet and ankles, and the occurrence of plantar fasciitis and ingrown toenails. Patients have difficulty fitting shoes. The foot deformity eventually leads to compromised blood supply and innervation of the forefoot, which in turn contributes to the development of osteoarthritis of the small ankles.
 | Among the diagnostic methods, the most important are plantography (detection of transverse flatfoot using footprints) and radiological examination (x-rays in direct and lateral projection). |
indications.
There are three main indications for disarticulation (amputation) of a body part, namely:
- gangrene
- Fatal diseases (eg, pandactylitis, which progresses to wet gangrene and can lead to high amputation, grade IV frostbite, malignant tumors, etc.).
- 'Invalid' diseases, ie those that lead to a complete loss of function (e.g. as a result of chronic arthrosis) or impair function (e.g. severe neuropathic pain).
Prior to an amputation, the physician must ensure that the patient's underlying conditions have been compensated for (ie 'reverse what is reversible'). In the case of impending amputation, this step includes measures such as checking blood sugar levels and performing revascularization for severe macrovascular lesions to avoid ischemia.
The method of toe amputation (evisceration or amputation) and the level of amputation (partial or total phalanx or metatarsal) depend on many circumstances but are primarily determined by the degree of disease and the anatomy of the lesion. With any amputation, the amount of postoperative loss of function is usually directly proportional to the amount of tissue removed. The big toe is considered the most important of the fingers in terms of function. However, the amputation of the big toe can be carried out with a small loss of function.
contraindications.
The main contraindication for amputation is. An indistinct demarcation line, The main contraindication to foot amputation is an abnormal demarcation line separating healthy skin from dead tissue. In this case, the surgeon does not know how high the amputation should be because the area with adequate blood supply has not been identified.
In general, amputation of a limb is contraindicated if it would result in impairment of quality and duration of life (situations where a person's life is at stake should not be considered). However, this contraindication does not apply to amputation of the nose.
Prevention of complications depending on the degree of amputation (disarticulation) of the lower limbs
In the second half of the last century, the degree of limb amputation was standardized according to the principle of the greatest possible functionality of the stump prosthesis system. Modern developments in surgical techniques and the level of prosthetic and orthopedic devices have rendered the previously developed systems obsolete. However, the most common complications and the resulting limitations in prosthetic functionality can still be observed today. This article analyzes the possible variants of complications associated with the degree of residual limb shortening, ways to prevent and eliminate them, and provides an overall assessment of the impact of residual limb length on statodynamic function at different levels.
keywords
Introduction. Restoring the function of the upper and lower limbs after their loss after amputation from an orthopedic point of view (for the upper limb - maximum functionality, for the lower limb - maximum possible support and locomotion) remains a topical problem to this day. Stump support depends on the resilience of the residual limb to unnatural loads, the extent of joint movement, the strength of each muscle group of the residual limb, the strength, control and endurance of the entire prosthetic residual limb, the musculature of the adjacent limbs and trunk, and the degree of biomechanical reproduction of the prosthetic duct depends entirely on the length of the severed segment [1, 2]. However, there are difficulties with amputations of the lower limbs: in the resection of individual 'problematic' levels, a number of conditions must be met in order to achieve success. Otherwise, there is a high probability of a dysfunctional 'non-functional' stump and consequent multiple/repeated surgical procedures [1,3].
COMMON APPROACHES FOR CHOOSING THE REDUCTION LEVEL
The unification of the procedure for selecting the amputation level began in the 19th century. So far, the height of the limb stump was determined solely by the tissue change. The term 'amputation level' refers to the length of separation of the bony segment. Various proposals have been made in the medical community at different times to facilitate subsequent fitting and use of the prosthesis depending on the level of limb bluntness [4].
At present, all previously proposed amputation schemes are considered irrelevant and should not be used in practice. However, there are still 2 main guidelines for recommending amputation levels:
- Due to the modern technical possibilities of surgical treatment and prosthetics, the choice of the level of amputation (disarticulation) should follow the principle established by NI Pirogov: 'amputate as low as possible';
- The choice of amputation level must be as favorable as possible for the success of an early prosthesis fitting.
Therapeutic gymnastics
To maintain muscle tone in the leg, knee and ankle flexion and extension exercises are started immediately after the operation. Maximum immobilization of the toes is maintained in the first postoperative weeks.

Toe exercises are started 4 weeks after the operation. The gymnastics for the toes ensures sufficient mobility after the operation.
Gymnastics should be performed only on the operated toes, for 10 minutes twice a day, until you can walk in ordinary shoes. When doing gymnastics, remove the bandage or spacer from the first toe and the adhesive patch from toes 2 through 5 and put them back on after the gymnastics.
The big toe must not be loaded after the immobilisation of the metatarsophalangeal joint.
washing the foot
The operated foot can be washed after the wound has healed. If the toe is fixed with metal spokes, wait until the metal spokes are removed.

If the toes have metal spokes attached, wait until the metal spokes are removed. Until then, protect your foot with a waterproof sleeve when you wash it. Before you come to the practice, order a product from the online shop that protects against moisture. The most suitable is the reusable waterproof foot bandage, www.limboproducts.co.uk.
The foot can also be covered with a waterproof pouch while washing by tying the neck tightly around the shin with tape. This method is less reliable compared to the above, and the bandage on the wound can get wet. If the bandage accidentally gets a little wet let it dry, if it gets very wet change the bandage and go to the nurse for that.
AD * Related products
Innovation and exclusivity through the development, design and manufacture of state-of-the-art foot care devices. Technology that combines orthopedic, artistic elements with other elements that can be replaced cosmetically and anatomically, in many cases also improving the functionality of the entire foot or depending on the missing part. Specific care for patients with amputations, deformities, partial or total deformities of one or both feet. Injuries that can result from trauma, are congenital, or as a result of diseases such as diabetes or cancer.
Useful prostheses for different types of partial foot amputations due to traumatic causes, genetic causes or diseases such as diabetes. Amputations such as transmetatarsal amputation * Lisfranc amputation or tarsal amputation * Chopart amputation or transarticular amputation * Syme amputation or ankle extrusion. Exclusive and specialized devices based on a technology that combines orthopedic elements, artistic elements and other elements that can be replaced cosmetically and anatomically, and in many cases also improve the functionality of the whole.
In 1840 Dr. James Syme of Edinburgh performed the cleft ankle amputation, crossing the tibia and fibula directly over their articular surfaces.
and distally fixed the heel tissue so that the end of the residual limb is able to support most or all of the body weight.
This procedure is used to treat serious injuries, infections, or deformities in the foot.
The amputee benefits from the increased resilience of the residual limb and the longer length of the residual limb.
better control of the prosthesis. The disadvantages are the risk of poor healing and spur formation and the unsightly convex shape of the residual limb.
Effects of amputation
From a conceptual perspective, it is important to keep in mind that the goal of amputation is not to improve the function of the operated limb, but rather to improve the patient's quality of life.
Amputations not only affect quality of life and mental health, but also life expectancy. It has been calculated that the mortality rate after major amputation ranges from 20 to 50 % in the following three years and reaches 70 % after five years.
The negative impact on the quality of life of amputees is significant and is referred to as the morbidity profile, which is greater the closer the amputation is.
It is known that the energy expenditure required for walking increases with the degree of amputation the closer the amputation is.
However, it should be noted that modern sub- and supracondylar prostheses have completely reversed this effect.
It is known that patients with comorbidities have higher basal energy expenditure and thus lower energy reserves, which translates into lower remaining energy for carrying out daily activities. This can even prevent the patient from getting used to the lower limb prosthesis, which entails a subsequent rehabilitation period.
This is a good reason to try to preserve limb length and not deprive the patient of a greater energy reserve when dealing with patients with generalized weakness and unlikely to succeed in the difficult adjustment and rehabilitation period complete, such as after a sub- or supraspinatus amputation.
Amputations may have a vascular trigger, be associated with complications of neuroarthropathy, or, more commonly, both. Chronic ulcers that are incurable or complicated by septic processes that cannot be treated with antibiotics will almost always occur in the sequence of events. However, indications still vary widely between centers and in some cases are imprecise.
In the Toursarkissian study, of 113 amputees (75 of whom had % diabetes), only 65 %s were alive at 10 months, and 17 %s required contralateral limb amputation at follow-up. Another Texas study reported a cumulative reamputation rate of up to 60.7 % over 5 years in 277 patients with diabetes. Patients who were independent in activities of daily living (ADL) before the amputation returned to their former independence more often with minor amputations than with major amputations (93 versus 61 %). Patients with minor amputations were able to walk earlier and longer. While large amputations have a higher mortality rate, small amputations have the same re-amputation rate and greater rehabilitation potential.
A patient with an amputation has a 30-50% higher risk of another amputation in the next 5 years.
Postoperative treatment and prosthetics after disarticulation
Treatment during the recovery period after surgery follows general principles of surgery. Once the sutures are removed, the patient is treated with physiotherapy and physical therapy. The residual limb is bandaged to achieve rapid regression and swelling. The patient must move both the sound limb and the bandaged joint symmetrically to get the feel of the phantom. This enables better functional results with the prosthesis. If the patient does not develop movement in the area of the removed limb, contractures in the joint of the missing limb segment may occur.
After surgery, the stump appears as a skin-covered area with scarring. The skin of the posterior surface of the thigh lies on it and is adapted to the pressure.
The prosthesis after disarticulation consists of a canvas or leather pelvic sheath. The pelvic component is hinged to the acetabulum. Modern hip joint designs allow the patient to sit and move relatively efficiently.
Express prosthetics is a method of prosthetics immediately after the removal of the limb, which is done directly on the operating table. This type of prosthesis is most commonly used after elective surgeries. For the first few days after the operation, the patient can walk around with the limb and only put limited weight on it. In this case the patient does not lose the sense of walking and 'grounding' when the limb is removed. This allows the patient to get used to the prosthesis more quickly.
Hip disarticulation is an operation used in the most extreme cases, when other treatments cannot help the patient, when limb preservation is impossible or even life-threatening.
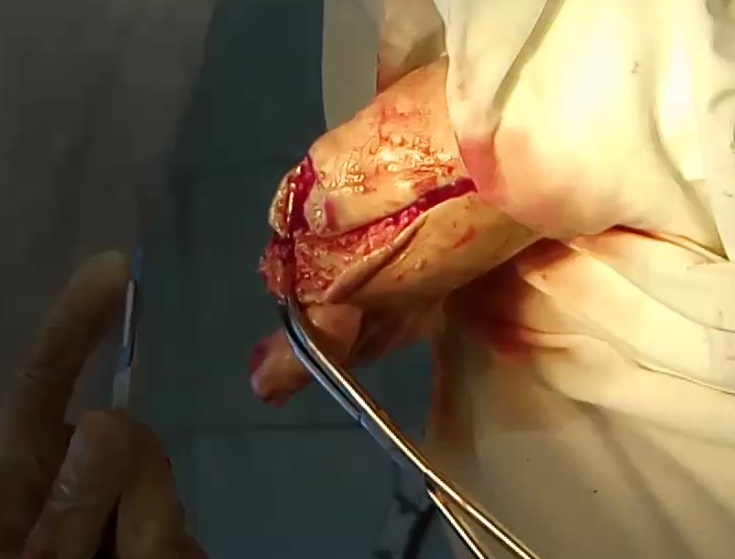
Unlike amputation, disarticulation is performed along the articular talus, the gap between the head of the bone and the level of the joint cavity. After severing the muscles and ligaments, the surgeon gains direct access to the joint and removes the head of the limb from the joint cavity using the Petrovsky or Faraber method. This creates a stump in place of the removed limb, to which a prosthesis can then be fitted.
accompanying symptoms
Accompanying symptoms associated with an amputation are damage to the arm or leg that does not heal or only with difficulty, as well as persistent pain. Amputation is unavoidable if these symptoms occur not only under stress but also at rest.
Severe infection leading to amputation is often accompanied by symptoms such as fever, chills, and fatigue.
After an amputation, if the wound heals well, no other side effects should occur apart from the loss of function due to the loss of the amputated body part. However, since amputations are often necessary in patients with a weakened immune system (e.g. diabetics) and poor circulation, wound healing problems often occur, especially in the case of extensive amputations. Pain in the area of the residual limb is particularly common. In some cases, the patients also complain about so-called phantom pains. This means that the patient feels pain or other discomfort (e.g. itching) in the amputated part of the body.
level of amputation
It is currently possible to clearly determine the amputation level using the so-called 'amputation level'. Amputation charts that divide the limb into vital, non-vital, and obstructive parts are considered obsolete and not used.
When determining amputation height and shape, the strength of the residual limb for attachment of a prosthesis should be considered.
Hand, elbow and shoulder amputations
The highest form of upper limb amputation is through the shoulder edge, ie between the shoulder blade and the torso.
Such an amputation is usually caused by malignant tumors and leads to significant cosmetic and functional limitations. Disarticulation of the shoulder joint, ie amputation of the shoulder at the level of the humerus, has the same effect.
In the case of an amputation at the level of the humerus, the doctor must ensure that there is enough space for an artificial elbow at the level of the amputation.
Disarticulation (amputation) at the level of the elbow joint is difficult in itself, since the bony prominences create painful pressure points in the socket area of the residual limb.
In the area of the wrist, not only the resilience but also the residual limb length, the sensitivity, the joint mobility and the possible types of grips have to be considered.
Leg, foot and lower leg amputations
Resilience is different on the lower limbs than on the upper limbs.
In the case of tarsal and metatarsal amputations, the doctor must ensure that there is enough intact foot skin, subcutaneous fat tissue and short flexor muscles to close the residual limb and scar the extensor side of the foot so that they are not loaded, otherwise painful pressure points can develop there .
In diabetic foot syndrome with necrosis (gangrene) or diabetic microangiopathy (capillary disease), border zone amputation is performed along the anatomical lines of the metatarsal bones.
preservation of the amputation
The most common operations are limb transplants (reconnection of the proximally amputated hand to the wrist or reconnection of the proximally amputated lower limb to the ankle) and their segments – foot, hand, finger. Hand and finger transplants are the most common in medical practice. But the nose, penis, scalp, auricle and others can also be replanted. When transporting a traumatized person to the hospital, it is important to ensure that the severed segment is preserved and viable. To do this, the amputee must be properly preserved (the main preservation method is to cool the amputee to +4°C; the amputee is placed in a plastic bag, which is placed in a bag with ice (snow) mixed with water). Each severed segment has a certain survival time in which replantation is possible (e.g. the survival time in hours at +4°C is: for fingers – 16, for hand – 12, for shoulder, forearm, das Shin and foot – 6).
- Primary surgical treatment of wounds (goal – removal of all damaged tissue and appropriate limb shortening, removal of foreign bodies from the wound)
- Bone skeleton reconstruction (alignment of bone fragments for better fusion, use of different immobilizing structures)
- Vascular reconstruction of the transplanted limb (anastomosis of vessels under the microscope, plastic replacement of veins and arteries possible)
- Reconstruction of the tendon-muscle apparatus (the most important and responsible stage of the operation, on which the functional result largely depends)
- Nerve reconstruction (the goal is the primary repair of the nerve)
- Skin regeneration (no stretching of the skin is allowed)
After the operation, bandages are applied and the necessary conditions for immobilization of the limb are met.
rehabilitation period
A correct and professional care of the patient during the postoperative period is essential for a good outcome of the limb transplant. After the operation, the patient is transferred to the intensive care unit. The main goal after surgery is to prevent the numerous possible complications that can occur in this category of patients. The patient is constantly monitored by the doctors, including checking the basic vital parameters (blood pressure, ECG, pulse, blood chemistry, etc.) and the circulatory status of the replanted limb. Replantation treatment is a comprehensive concept and includes: medication, physical therapy, massage, occupational therapy, electrical muscle stimulation, laser therapy, physical therapy, hydrokinesis therapy and much more.
Properly performed replantation restores mobility, sensitivity and the ability to resume previous activities with the damaged limb.
Statistically, regeneration of fully amputated fingers is achieved in 70-75 % of cases, while partial amputation occurs in 90 % of cases.
Our specialists will contact you shortly
Subscribe to the NCC #2 (Central Clinical Hospital of the Russian Academy of Sciences) Telegram channel to stay up to date with our news.
species
A mobile deformity occurs when the fingers are still mobile and positioning is possible. Over time, it develops into a permanent deformity. In this case, the fingers cannot be formed normally.
The main symptom of toe deformity is pain syndrome. The discomfort occurs in different places (from the toe to the ankle) depending on the distribution of the load when the compensating mechanisms are activated.
Typically, patients primarily experience pain on the dorsal surface near the proximal interphalangeal joint, caused by excessive shoe pressure on the deformed toe.
The metatarsophalangeal joint of the big toe is affected by the increased pressure. The redistribution of the load pressure causes pain in the entire foot and in the ankle area.
In patients with claw deformity, the fat pad is often shifted towards the toes. It is normally located under the metatarsophalangeal joint of the big toe and serves as a natural shock absorber. In a clawed deformity, the thickening shifts forward toward the toes, increasing the load on the forefoot.
With a fixed claw deformity, patients usually experience persistent blistering. The excessive keratinization and thickening of the skin is a protective mechanism and is caused by excessive pressure on unadapted areas. Commonly, calluses form on the back of the toes, on the balls of them, and around the prominence of the metatarsophalangeal joint.
Microcirculation disorders can cause ulcer-like defects. Ulcerations form on the skin that do not heal over time.
causes
Claw deformity often occurs against a background of foot deformity (valgus or transverse flatfoot) resulting from abnormal load distribution and consequent dysfunction of the flexor and extensor muscles. Triggers can be:
- wearing uncomfortable or poor quality footwear;
- Peculiarities of foot anatomy;
- genetic predisposition;
- Trauma to toes and feet (bruises, dislocations, fractures);
- Inflammatory lesions of the metatarsophalangeal joint;
- Rheumatoid arthritis;
- metabolic diseases;
- diabetes mellitus;
- disorders of the peripheral nervous system;
- high vault.
The predisposition to toe deformity is increased in older people due to chronic diseases, as well as the natural decrease in the functioning of joints, tendons and muscles.
costs of the services.
- Familiarization with the patient's clinical foot condition and medical history
- Clinical examination
- Symptoms of the pathology
- Review of blood tests, X-rays, CT and MRI scans
- diagnosis of the disease
- Prescribing the most appropriate method of treatment
investigation and advice
- Examination and planoscopy
- production of orthoses
- consumables
- Advice on preventive measures
- Post-operative follow-up care
- X-ray, MRI and CT findings
- Advice on rehabilitation
- Intra-articular injection of hyaluronic acid (if necessary)
- removal of the threads
opinions of doctors
These are real people's opinions, taken from the doctor's website on prodoctorov.ru
My name is Elena Vorobyeva. I had hip surgery in August 2021. In February 2022 I came for another check-up. The doctor said that everything was absolutely fine.
I went to Denis Sergeyevich for advice on knee replacement. He had previously been diagnosed with osteoarthritis of the knee at the same clinic and recommended surgery. Physician .
My grandmother (91 years old) had a complicated dislocated shoulder fracture. Nobody wanted to help her and it was scary sending my grandmother to the hospital with burns. Several doctors said they couldn't help her. from.
I, Mitropolevsky Tatiana Valentinovna, born in 1949, underwent surgery for a cemented total left hip arthroplasty. The first similar operation on the right joint.
I live in the Rostov region. For the last two years I was very worried about the pain in my hip joint, nothing was working anymore and I decided to have an endoprosthesis put in. On the advice of a surgeon in Rostov, I decided to do this procedure.
For over a year I had intermittent, wandering pelvic pain that was aggravated by sitting or lying on my side. I went through all the doctors of gynaecology, urology, proctology, neurology, etc.
I went to the doctor with severe pain in my hip joint, I could hardly walk. Denis Sergeevich carefully examined the patient, made a diagnosis, and then began manipulation.
dr Yakushev Denis Sergeevich is an orthopedist and traumatologist, but he is also a doctor and a man of stature. dr Yakushev operated on my mother's right hip joint in 2016. The operation was an emergency.
I really liked everything about it! The doctor thoroughly explained everything and explained the situation. Clear and understandable! He was very accommodating and professional! It was a pleasure speaking with him. I recommend him to 100%!!!
I want to thank Denis Yakushev very much! I went to him for a torn biceps tendon. Diagnosis was made very quickly and surgery was scheduled immediately. The operation was performed by .
Read more:- The reamputation is.
- Indications for amputation.
- Life after a leg amputation.
- blunt.
- disarticulation is.
- Limb amputation.
- prosthetic legs.
- acetabulum.
