Regardless of whether you have the first symptoms of a broken foot or not, it is worth seeing a specialist. He or she can help you identify a specific foot fracture.

- pain in the foot
- -the heel area
- causes of injuries
- First aid for foot fractures
- The tarsal bones
- Types of foot sprains
- ankle sprain
- metatarsal fractures
- fractures of the toes
- Causes of metatarsal fractures
- diagnosis
- How long does it take for a fracture to heal?
- Possible complications after the injury
- Bones of the lower extremity
- Skeleton of the free part of the lower limbs
- causes of injury.
- The diagnosis.
- Fifth metatarsal fracture symptoms
- causes of injury
- Which doctor should I see?
pain in the foot
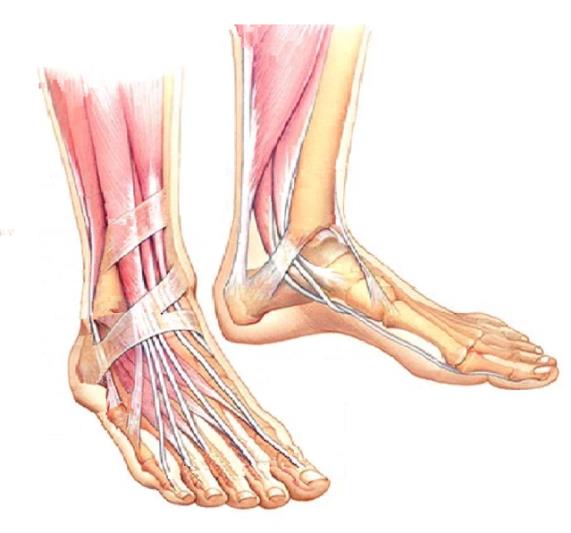
The human foot consists of 26 bones and 33 joints. The height of the instep, the arch of the foot and the shape and size of the toes vary greatly from person to person. For this reason, the foot is rightly considered a complex anatomical area and deserves its own orthopedic specialization.
'The foot hurts' is the complaint most patients come to me with. 'The foot is big so show me exactly where it hurts'. – is one of my standard answers.
The foot is used to move the body in space. As long as the foot is fine, don't pay much attention to it. However, if it hurts, you want to get rid of it immediately. In order to start the right treatment, it is important to know where the problem lies.
The foot can be divided into several areas to pinpoint the pain:
-the heel area
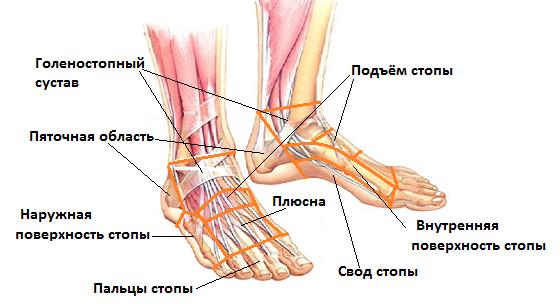
In a next step, the arch of the foot and the inner surface of the foot are examined in close proximity. A distinction is made between the inner and outer longitudinal and transverse arches of the foot. A malfunction of these anatomical formations is the cause of the vast majority of foot problems. In this section we deal with the pathology of the internal longitudinal vault, fractures of the bones that form this vault, and diseases of the joints within this vault.
causes of injuries
With these fractures, the patient is prone to acute pain, so the recovery time is long.
A fracture of the foot or leg is characterized by the following symptoms
- The leg is in an abnormal position;
- swelling of the foot and ankle;
- pain in foot and ligaments;
- The big toe appears visually smaller;
- the ankle turns red and bleeding occurs;
- Mobility is drastically reduced;
- Sudden numbness and cold feeling in the leg.
The above symptoms of a broken leg or limb are rare.
First aid for foot fractures
First, the injured person must be taken to a hospital. But before that happens, the person with the foot fracture must receive first aid.
And if loved ones are wondering how to help an injured person with a broken foot bone, they should
- Limit the person's mobility. This can be done by placing a small pillow under the broken foot.
- Apply a cold compress. Relatives of the patient can take a bag, put 2-3 ice cubes in it, wrap it in a cloth and put it on the problem area. The compress should remain on the foot for 10-15 minutes. Then take a 5 minute break and repeat the process.
- Apply a bandage, but not an airtight one.
A person with a foot fracture needs to be x-rayed, diagnosed and treated appropriately at the trauma center. The X-ray images are made in several projections. This is the only way to determine the nature of the injury.
The doctor examines the injured limb and determines the mechanism of the injury.
The tarsal bones
The five metatarsal bones (ossa metatarsalia) are the counterpart to the metacarpal bones. They connect the tarsal bones to the toe bones of the foot. Each metatarsal consists of a base, a shaft, and a head that connects to the phalanges of the toes.
The toe bones (ossa digitorum pedis) are the toe bones. Like the fingers of the hand, the toes of the foot are made up of the proximal, middle, and distal phalanges. Only the first toe, called the big toe, does not have a middle phalanx.

Lovtseva Irina Nikolaevna – doctor of venereology, experience 27 years. Discount on a visit to the doctor! All opinions about the doctor. Make an appointment online or by phone.
Diagnosis, treatment and prevention of skin diseases, minor surgical interventions in dermatology and cosmetology, laser dermatology, laser cosmetology, medical pedicure and manicure, aesthetic cosmetology, injectable cosmetology, therapeutic cosmetology with a wide range of peelings, masks, serums, creams, cosmetology in the Trichology, body cosmetology.
Types of foot sprains
ankle sprain

A complete dislocation of the foot is a relatively uncommon injury. These dislocations are always accompanied by severe damage to the ankle ligaments and a fracture of the ankle. Foot dislocations are rarely combined with other intra-articular fractures.
The foot can be dislocated outwards, inwards, backwards, forwards or upwards. External foot dislocation occurs when the foot rotates outward and to the side and is associated with an external malleolus fracture. If the patient turns the foot inwards, the foot can be dislocated internally in combination with a fracture of the inner ankle.
A posterior sprain is usually caused by a sudden, violent flexion of the foot toward the sole of the foot, or by a severe blow to the front shin. An anterior dislocation of the foot can be caused by a sharp blow to the shin from behind or by suddenly bending the foot backward violently. An upward dislocation of the foot is very rare and usually occurs as a result of a fall from a height.
The patient with a dislocated foot is disturbed by a stabbing pain in the ankle. External examination reveals significant swelling, elevation, bruising, and deformity of the ankle. It is not possible to move the joint and support the leg.
X-rays are taken in two projections to clarify the diagnosis and to identify accompanying bony injuries. Sprains of the foot with bone and ligament injuries are among the most serious injuries. Proper joint function is only possible if the correct fracture position is restored as accurately as possible.
Successful reduction of a dislocated foot depends on several conditions: thorough evaluation of the dislocation and fragment displacement, appropriate anesthesia, and a correct and consistent approach by the trauma surgeon to reduction of the foot. Fresh foot dislocations are operated on under general, local or regional anaesthesia. If necessary, muscle relaxants are used.
metatarsal fractures
Fractures in the metatarsal bones result from being hit, dropping a heavy object, or putting pressure on the foot. They cause pain and swelling in the forefoot area. Without x-rays, it is difficult to determine the exact location of the injury because the pain is diffuse. With the help of X-rays of the foot, all the necessary information about the level and type of fracture can usually be obtained. MRI and CT scans of the foot are rarely required.
Treatment of injuries without displacement or with a displacement of less than ½ the bone diameter is performed on an outpatient basis. A bandage is applied, and after 5-7 days a plaster cast is applied. Fixation is performed for 3 weeks in children under 8-10 years old and 4 weeks in elderly patients. Typically, the foot is allowed to walk again 10-12 days after the injury.
An angular displacement and a displacement of more than ½ of the bone cross-section is an indication for hospitalization. The reduction is performed under anesthesia. The child is placed on its back. An assistant holds the shin with one hand and the heel with the other. The traumatologist straightens the toe corresponding to the injured bone. At the same time, pressure is applied to the fracture site with the other hand to eliminate the angular and latitudinal shift. Then, as in the previous case, a plaster cast is applied, and after 5-7 days a bandage is put on. The duration of fixation is 5-6 weeks. The leg can be used from the 15th to the 18th day. After the cast is removed, an epiphyseal splint should be worn for 6 months.
Surgical intervention is rarely required when there is open trauma, soft tissue is trapped between the fractures, and the fragments cannot be held in place. The operation is performed under anesthesia. Metal structures, as a rule, are not used. The fragments are sutured or fixed with a needle. Further treatment is similar to dislocation injuries.
fractures of the toes
Toe fractures are most commonly caused by dropping heavy objects and are often open or involve a serious soft tissue injury. A diaphyseal injury is easy to recognize: bleeding, swelling and pain, functional impairment and a positive axial load sign. With epiphysiolysis without displacement, the symptoms can resemble a bruise; in an epiphysiolysis with displacement, the phalanx is dislocated. X-rays are helpful in making a diagnosis.
The treatment takes place in a trauma clinic. If there is no dislocation, a plaster cast is applied for 7-10 days. It is not advisable to limit yourself to a plaster cast - it causes swelling and is ineffective in mobile children. Dislocated fractures and epiphyses are reduced under local anesthesia. If the fragments cannot be securely fixed with plaster, percutaneous fixation with a needle or hypodermic needle is performed.
When fixing main phalanx fractures, the finger is flexed so that it remains in a flexed position until the needle is removed. Osteosynthesis of the middle phalanx and nail phalanx is performed in an upright position. A plaster cast is then applied, the splint is covered with a sterile cloth, and bandages are applied every 1-2 days. After 12-15 days, the child is sent for follow-up X-rays. If there are signs of callus formation, the spoke is removed.
Causes of metatarsal fractures
Depending on the pathogenetic factor, fractures are distinguished into: traumatic. Acute injuries result from dropping heavy objects on the foot, twisting the forefoot (the base of the fifth metatarsal is more commonly fractured), etc. Open fractures account for 10 % of all injuries. pathological. A number of factors - osteoporosis, arthrosis, tumors, drugs, genetic factors, unbalanced diet with a lack of minerals and vitamins - weaken bones. A small force is enough to cause a fracture. Stress-Related Injuries. Persistent foot injuries of mild to moderate intensity are seen in military personnel who do a lot of marching, ballet dancers, and athletes. The second and third metatarsals are fixed, while the first, fourth, and fifth are relatively flexible. For this reason, fourth metatarsal fractures are common. When walking and dancing, the second and third metatarsal bones are subjected to the most stress, so the risk of stress fractures in these structures is higher. neuropathy. Fractures of the metatarsals (more commonly the fifth metatarsal) occur in patients with complicated diabetes. In polyneuropathy, the sensitivity of the feet is disturbed and the affected person is no longer able to control his or her strength due to the loss of feeling.
A first metatarsal fracture is suspected when the thumb becomes swollen and deviates from its normal anatomical axis.
Symptoms of an open injury include protrusion of bony structures from the wound to the external environment, bleeding, and excruciating pain.
Stress fractures have no obvious symptoms. Initially, there is a dull, painful pain in the foot during motor activity, later also at rest. In some patients, a deformity of the foot due to stretching of the intrinsic muscles can be observed.
In patients with neuropathy, a reduction in pain is observed and the patient consults a podiatrist complaining of a change in the appearance of the foot.
diagnosis
The choice of examinations determines the correct treatment of the patient and the avoidance of complications. Depending on the clinical picture, the patient may undergo examinations:
X-ray examination – The basic examination that is carried out for foot injuries. The information about it is often insufficient. An early stress fracture is not visible on conventional radiographs, or there is a small periosteal reaction that is easily missed. Examination shows a fracture of the metatarsal bone but is not suitable for diagnosing soft tissue and ligament injuries.
computer scan Provides more information about the pathology. Indications include suspicion of a stress fracture when x-rays are inconclusive. CT scan shows burst injuries, fragmentation injuries and any bone pathologies.
MRI – is the most powerful method for evaluating complex foot injuries involving soft tissue and torn/torn ligaments. MRI shows bone marrow swelling earlier than CT. MRI is the best imaging technique for stress fractures of the foot and is useful in distinguishing synovitis from degenerative changes. Combining MRI and CT is the best way to get a complete picture of the components of the foot – tarsal bones, metatarsal bones, pontics, hard and soft tissue structures.
Ultrasonic Ultrasound is used in trauma surgery because it is easily accessible and easy to use, but it is not a diagnostic tool in its own right.
How long does it take for a fracture to heal?
Complete healing of a fracture (closed, without displacement) occurs within 8 weeks with appropriate therapy. The healing process can be slowed down by the following factors
- high severity of the fracture
- large amount of bone fragments;
- complications;
- untimely medical treatment;
- advanced age of the patient;
- presence of concomitant diseases;
- inappropriate treatment methods.
Possible complications after the injury
With a favorable prognosis and a correctly selected therapy and rehabilitation scheme, the fracture heals within a few months. At the end of the recovery period, the sufferer can return to a normal, physically active life.
Failure to comply with the above conditions can result in serious consequences. This includes:
- Persistent pain in foot;
- Arthritis;
- limb deformity;
- Longitudinal and transverse arch prolapse (flatfoot);
- formation of bony prominences;
- limited mobility of the foot.
To reduce the risk of complications, it is important to know how to provide first aid and follow the doctor's instructions for treatment and rehabilitation.
Bones of the lower extremity
The pelvis (os coxae) consists of three separate bones connected by cartilage until the age of 12-16 years: hip bone, pubic bone and ischium, which are fused together at this age.
The hip bone (os ilium) consists of two parts. The lower thickened part, the hip bone shaft (corpus ossis ilii), is involved in the formation of the hip socket. The upper, wider part is the wing of the hip bone (ala ossis ilii). It is a wide, curved plate that narrows in the middle. The wing is thickened at the periphery, fan-shaped and ends in the iliac crest (crista iliaca).
The pubic bone (os pubis) has an extended part, the body, and two branches. The body of the pubic bone (corpus ossis pubis) forms the front part of the hip socket. From it the upper branch of the pubic bone (ramussuperior ossis pubis) goes forward, with the eminentia iliopubica located along the line connecting the pubic bone with the ilium (iliopsoas).
The ischial bone (os ischii) has a thickening (corpus ossis ischii), which closes off the hip socket from below and merges into the ischial branch (ramus ossis ischu) at the front.
[2], [3], [4], [5], [6], [7]
Skeleton of the free part of the lower limbs
The femur is the longest tubular bone in the human body. It has a shaft and two ends. At the upper (proximal) end is the femoral head (Caput femoris), which connects to the pelvic bone.
The tibia consists of two bones. The tibia is medial and the fibula is lateral. Every bone has a body and two ends. The ends of the bones are thickened and have connecting surfaces to the overlying thigh bone (tibia) and to the underlying foot bones. Between the bones is the shinbone space (spatium interosseum cruris).
The tibia is the thickest bone of the shinbone. The proximal end of the bone is thickened and forms the medial and lateral condyles (condylus medialis et condylus lateralis). The upper articular surface (facies articularis superior) is directed upwards and connects with the condyles of the thigh.
The fibula is thin and has a fibula head (caput fibulae) at its upper (proximal) thickened end. On the medial side of the head is the articular surface of the head of the fibula (facies articularis cdpitas fibulae) for articulation with the tibia.
Foot (pes) is divided into 3 parts: tarsal, metatarsal and toes. The skeleton of these parts consists of the bones of the tarsus (ossa tarsi), the bones of the metatarsus (ossa metatarsalia) and the bones of the toes (ossa digitorum pedis).
causes of injury.
These injuries often occur for the following reasons:
- Roll the foot inward
- Sudden twisting of the foot
- Direct hit to the foot or toes
- An unfortunate fall or leap onto your foot from a great height
It is important to seek immediate medical attention as the consequences of a dislocated foot can be catastrophic: diseases such as arthritis or osteoarthritis may develop, the injured joint may become less mobile after healing, and there may be partial or complete muscle wasting or circulatory disorders in the limbs.
The diagnosis.
After the accident, the injured person must be taken to the trauma ward immediately and must not be able to perform any leg movements (active or passive). After admission, the doctor will conduct a thorough examination of the injured limb and take a full medical history. Only with the help of an X-ray can the trauma surgeon make an accurate diagnosis (determining the type of dislocation) and initiate appropriate treatment.
Treatment should only be performed by a qualified traumatologist.
- Reduction of a dislocated foot under local or general anesthesia
- Immobilization of the dislocated joint with a plaster cast
- Immobilization for 8 to 12 weeks (depending on the type of sprain and the severity of the injury)
- Administration of pain medication (if necessary)
- For the first few days, you should take an elevated and cold position.
- It is absolutely forbidden to lean or stand on the injured limb during treatment.
Fifth metatarsal fracture symptoms
Symptoms vary greatly depending on the type of fracture. In some cases, e.g. B. in stress fractures, the patient may confuse the symptoms with a simple bruise. It may be that there is no pain at all, and the pathology is diagnosed only on circumstantial evidence. A stress fracture of the metatarsal presents with the following symptoms:
A traumatic fracture is more pronounced. In these cases, after the injury to the bone, a characteristic crunching sound is clearly heard, which automatically indicates deformation. Pain follows almost immediately. Other symptoms of a traumatic fracture are.
- The appearance of severe swelling with hematomas after a few hours;
- misalignment of one or more fingers;
- Decreasing pain followed by an increase in pain on exertion.
An open metatarsal fracture is characterized by soft tissue tears and bleeding. This causes intense pain that is difficult to ignore. The ends of the metatarsal emerge to the surface and are easily discerned visually through the torn skin. A metatarsal fracture requires urgent treatment, even if the symptoms are very mild, as it can lead to serious complications.
causes of injury
There are two types of fractures, each caused by different factors. The stress fracture is milder and often heals spontaneously. It is caused by prolonged excessive stress on the foot. These can occur when:
In these cases, the foot is loaded over a long period of time, which leads to microfractures in the bone tissue. Traumatic fractures have more obvious causes. They are caused by external mechanical influences on the forefoot. These situations can occur when:
With the traumatic form of the pathology, a fracture of the 5th metatarsal is most common. The second most common deformities are the first and second. Jones fractures are considered particularly serious: The fifth bone is destroyed in an area with limited blood supply.
Which doctor should I see?
When the foot suffers trauma, it loses much of its cushioning properties. This means that the load is redistributed to other parts of the musculoskeletal system, which can certainly lead to new diseases. For this reason, treatment of a metatarsal fracture is crucial. The diagnosis of the disease and its treatment are carried out by:
Read more:- Cracked metatarsal.
- metatarsal bones.
- tibia and fibula.
- metatarsal and metacarpal bones.
- fibula.
- bones of the foot.
- tarsus.
- tarsal and metatarsal joints.
