Where can I have the MRI scan recommended by my doctor?
- Chronic instability of the kneecap
- Causes of chronic kneecap instability
- Clinical anatomy of the synovial membrane
- keywords
- Structural features of the knee Structure of the knee joint | Magazine article.
- Magnetic resonance imaging in the diagnosis of trauma.
- X-ray and magnetic resonance imaging.
- Treatment principles for delaminating osteochondritis of the femoral condyles
- Does Fabella really cause osteoarthritis?
- Why it's coming back
- Highlights
- Symptoms and signs of sesamoiditis
- Treatment of menisitis (sesamoiditis)
- Features of treatment
- Conservative techniques
- Surgical Techniques
- forecast
- Big toe metatarsophalangeal joints
- bones of the fingers
- What is bone tissue?
- Stages of formation of normal hand bones
- Muscular structure of the hand
- Summary
Chronic instability of the kneecap
The kneecap is commonly referred to as the 'kneecap'. It is a well-known bulging bone that is visible when the knee is flexed and extended.
Medically speaking, the kneecap is the largest sesamoid bone, that is, the bone that lies in the thicker part of the tendon. The sesamoid bones increase the grip of the muscle and act like a block. The tendon in which the kneecap is located is formed by the union of the 4 muscles of the front thigh (quadriceps). When extended, the kneecap lies over the talus articularis and when flexed, it fits into the notch between the two condyles of the thigh.
This area of the knee joint is also called the patellofemoral joint (or patellofemoral joint, from the Latin terms patella, kneecap, and femur, thigh bone).
The kneecap is covered with a thick layer of cartilage, which is the thickest layer of cartilage in the human body, to ensure perfect gliding during movement.
If the kneecap does not lie properly in the notch and is not properly aligned when the leg is flexed, it is referred to as kneecap instability - an impairment of the joint's supporting function, which clinically manifests itself as instability and dislocation.
Such conditions are successfully corrected by the doctors of the International Center ON CLINIC through minimally invasive arthroscopic procedures.
Causes of chronic kneecap instability
The kneecap is held in a stable position by muscles and two ligaments called patellar cushions. One prevents it from moving inwards, the other prevents it from moving outwards. Normally their grip is balanced and the kneecap sits squarely inward. When balance is disturbed, the kneecap tends to move outward.
The following causes can lead to kneecap instability:
- torn or dislocated ligaments;
- muscle weakness;
- dysplasia of the femoral condyles;
- abnormal shape of the limbs;
- X-shaped or valgus curvature of the tibia;
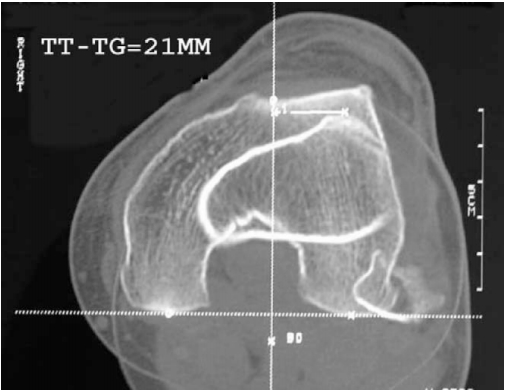
- External position of the tibial tubercle, to which the patellar ligament attaches;
- hyperextension of the knee joint;
- Internal rotation of the tibia, e.g. B. as a result of flat feet;
- dysplasia of the kneecap;
- weakness or hyperextension of the patellar attachment;
- dysplasia of the distal part of the thigh;
- Valgus deformity of the knee joints;
- Deforming gonarthrosis;
- Fractures and fractures of the femoral and tibial heads.
Generally, it is a combination of factors rather than a single factor that leads to kneecap instability.
Trauma is a common cause of kneecap instability:
- Anterior cruciate ligament tear, with or without meniscus tear;
- tear of the retaining ligaments;
- Torn posterior cruciate ligament, usually in combination with other injuries;
If there are repeated episodes of kneecap dislocation, one can speak of chronic kneecap instability. This pathology is usually caused by misdiagnosis of the primary external dislocation of the kneecap and/or incorrect treatment tactics.
Clinical anatomy of the synovial membrane
Kubeko, AV Clinical anatomy of the synovial membrane / AV Kubeko, LA Davydova. – Text: direct // Young Scientist. – 2022. – № 41 (436). – C. 219-222. – URL: https://moluch.ru/archive/436/95461/ (access date: 03/22/2023).
Knowledge of the peculiarities of the structure of the osteochondral system of the knee joint plays an important role in the correct diagnosis and further treatment of the disease.
Keywords: Sesamoid bone, fabella, knee joint, hamstrings, fabella topography.
The aim of this study was to detect the sesamoid bone (fabella) and determine its shape, size and prevalence in the Belarusian population depending on age and gender.
Sesamoid bones are small bones located in the thickness of tendons passing through a joint and usually lying on the surface of other bones. Sesamoid bones are round or disc-shaped and vary in size between 0.3 and 4.5 cm. The largest and most durable sesamoid bone in the human body is the kneecap (patella) in the knee joint, but another sesamoid bone, the fabella, is becoming increasingly common and covers the knee joint from behind.
The word Fabella is derived from the Latin diminutive faba', which means bean, cap'. The presence of the sesamoid fabella in humans is highly variable and, according to the literature, can occur in 10-30 % of the population. [1]
According to the literature, the main function of the labrum is to stabilize the medial condyle of the femur and the labral complex, which consists of the plantar and calf muscles as well as the arch, labellofibular, labellopliteal and oblique tendons. (2) (Fig. 1) In four-legged mammals, the lip is thought to play a similar role to the patella by redirecting the tensile forces of the knee joint from one point to another. In bipedal mammals, the labia does not touch the back of the flexed knee, so its role in redirecting forces is less.
keywords
Structural Features Knee Structure of the knee joint | Magazine article.
Good mobility Knee Knee is important for standing, walking and running.
Knee joint – The connection between the femur and the shinbone bone.
Outside and inside laterally Bands prevent excessive mobility of the knee from side to side.
Knee jointarticular cartilage, lateral cartilage, joint space, X-ray picture.
Magnetic resonance imaging in the diagnosis of trauma.
A retrospective analysis of 89 MRI and X-RAYS-Investigations Knee joint
X-ray Knee X-rays of the knee joint X-rays of the knee joint laterally view over
Knee of the jointArticular cartilage, lateral cartilage, joint space, X-ray picture
conservative treatment, femur femurArticular cartilage, patient, lesion, treatment.
X-ray and magnetic resonance imaging.
osteophytes X-ray picture and in the MRI, osteophytes were seen as marginal bulges of the articular surfaces Bone(Illustration 1). Osteophytes in X-ray picture were in the medial and lateral area in 40(59.7%), in the MRI in 67(100%) and 57(85%) joints noted.
Treatment principles for delaminating osteochondritis of the femoral condyles
Other locations are much rarer: 19% contact surface of the medial femoral condyle, 17% lateral femoral condyle .7% medial side of medial femoral condyle .7% Patellofemoral joint joint.
Does Fabella really cause osteoarthritis?
There is no clear answer to this question. One can speculate that Fabella weakens the friction within the knee joint and redistributes the load to the muscles and tendons, causing more wear and tear on the cartilage tissue than usual. There is no conclusive research on whether this is the case or not. But there is more to it.
Fabella is thought to interfere with knee replacement surgery and prevent this surgical procedure from being completed and effective. Another unpleasant 'bonus' is pain and discomfort.
The presence of fabella in the body prevents knee replacement surgery from being performed.
Why it's coming back
Scientists suspect that Fabella evolved in the opposite direction due to modern humans' eating habits. We consume high-calorie foods and people are overweight - orthopedists often recommend weight loss. The shin bones have become longer and the calf muscles have become larger. This increased the load on the knee joints. They became more active and came under more pressure. The inflammation of the sesamoid bone below the knee progressed and with it the pain.
Modern orthopedic surgeons, constantly looking for the causes and mechanisms of arthrosis in the knee, are interested in studying Labelli. They are convinced that it can help in the treatment of various knee diseases in the future. Meanwhile, statistics are being compiled on the geographical and gender preference of this bone and its presence in one or both knees is being studied. Time will tell whether this will shed light on the problems in treating osteoarthritis.
Highlights
Dancers, runners, and people with arched feet, who wear high-heeled shoes, or have bunions are prone to pain in the sesamoid bone under the head of the first metatarsal toe.
The diagnosis is made based on clinical findings; infection is ruled out by analyzing synovial fluid if the joint is swollen, and a fracture is diagnosed by x-ray.
The patient is prescribed new shoes with a thick sole and orthopedic insoles to reduce pressure on the sesamoid bones.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
Symptoms and signs of sesamoiditis
The pain in sesamoiditis occurs below the head of the first metatarsal bone; The pain usually worsens when standing or wearing soft, thin-soled shoes or high heels. When inflammation occurs, there is occasionally moderate swelling and local fever, and more rarely, redness that may spread medially and appear to involve the metatarsophalangeal joint of the big toe. A fracture of the sesamoid bone also causes pain, moderate swelling, and possibly inflammation.
When the foot and thumb are dorsiflexed, the heads of the metatarsals should be examined and palpated separately. The sesamoid bones are painful, especially on the tibial side. Hyperkeratosis, which can manifest as calluses or skin hypertrophy, can also cause pain.
If inflammation and circumferential swelling develop in the metatarsophalangeal joint area, LP may be necessary to rule out gout and infectious arthritis.
Radiological examination is indicated if fractures, osteoarthritis and sesamoid displacements are suspected. Sesamoid bones, separated into fragments by spacers made of cartilage or fibrous tissue, may show signs of fracture on x-ray. If the X-ray image is not meaningful, an MRI examination is necessary.
Treatment of menisitis (sesamoiditis)
For patients with sesamoiditis, it may be enough to avoid wearing the shoes that cause pain. If symptoms of sesamoiditis persist, it is advisable to wear thick-soled shoes and orthopedic shoes that reduce pressure on the sesamoid bone. For non-dislocation fractures, conservative treatment with immobilization of the joint may be effective (flat, sturdy orthopedic shoes can be used).
Non-steroidal anti-inflammatory drugs (NSAIDs) and corticosteroid injections with local anesthesia may be effective (see 'therapies'). Recommendations for the use of corticosteroid injections Use of corticosteroid injections ). Surgical removal of the sesamoid bone is indicated when conservative treatment has failed, but there is conflicting evidence regarding its effectiveness, as surgical intervention can cause biomechanical and movement disorders of the foot. If inflammation is present, conservative treatment in the form of a combination of local glucocorticoid injection and anesthesia is indicated.
Features of treatment
Conservative techniques
In general, problems caused by patellar tilt/subluxation are treated with conservative methods that rely primarily on performing specific exercises that rebalance the extensor muscles.
The so-called taping is also considered effective in relieving pain in the knee area and balancing the kneecap outwards.
However, it should be noted that in some cases, despite the effectiveness of conservative procedures, surgery is required.
Surgical Techniques
The surgical techniques are based on the arthroscopic introduction of a video camera, which allows a detailed view and assessment of the kneecap and all other components of the knee joint from the inside.
If only the kneecap is dislocated, the oblique part of the broad muscle and the entire lateral ligament are severed.
Schematic representation of arthroscopic dissection of the outer edge of the kneecap.
This is a rudimentary description of the basic and most common surgical procedure to correct kneecap subluxation and/or tilting. However, as a rule, there are several variants of the same clinical situation, requiring an individual approach to their elimination.
forecast
In the vast majority of clinical situations, treatment of the subluxation/tilt produces a favorable outcome. With the right approach and an appropriate conservative and/or surgical treatment strategy, there is a high probability of complete healing and recovery of the patient with the possibility of a relatively quick return to an active lifestyle and sports.
Of course, the intensity of rehabilitation measures must be gradually increased to avoid re-traumatization of the previously injured area of the knee.
Big toe metatarsophalangeal joints
The big toe joint consists of five bones. The metacarpal of the first finger is shorter than the others, but massive. The second metacarpal is the longest. The length of the following bones decreases towards the ulnar edge of the hand. Each metacarpal bone has a base, a shaft, and a head.
The bases of the metacarpals are connected to the carpal bones. The bases of the first and fifth metacarpals have saddle-shaped articular surfaces, while the others have flat articular surfaces. The heads of the metacarpals have a hemispherical articular surface and are connected to the proximal phalanges of the fingers.
bones of the fingers
Each finger consists of three phalanges: the proximal, the middle and the distal. With the exception of the first finger, there are only two phalanges: the proximal and the distal. The proximal phalanges are the longest and the distal phalanges are the shortest. Each phalanx has a central part, the body, and two ends, the proximal and the distal. At the proximal end is the base of the phalanx, at the distal end is the head of the phalanx. Each end of the phalanx has articular surfaces that are connected to neighboring bones.
In addition to these bones, the hand has sesamoid bones, which are located in the thickness of the tendon between the metacarpal bone of the thumb and its proximal phalanx. There is also a non-permanent sesamoid bone between the metacarpal bone and the basal phalanx of the second and fifth fingers. The sesamoid bones are usually located on the palmar surface, but occasionally occur on the posterior surface. The pea also belongs to the sesamoid bones. All sesamoid bones, as well as all their appendages, increase the strength of the arms of the muscles attached to them.
Literature used: Medical Atlas. Human anatomy. Bilich 2012.
What is bone tissue?
Bone tissue is the mineralized connective tissue that makes up bones. It performs important functions such as protecting soft tissues, storing calcium and phosphate, and participating in movement. Bones are not lifeless organs. They are extremely dynamic structures in which the process of bone formation and breakdown occurs constantly. In addition, recent research shows that bones influence the activity of other organs and systems. In addition to their musculoskeletal function, they also have an endocrine function, which is due to the release of biologically active substances from some of their cellular components. Bone tissue consists of three types of cells: osteoblasts, osteoclasts and osteocytes.
- Osteoblastscome from mesenchymal stem cells. Their main function is their involvement in bone formation and mineralization. They are cubic cells that make up 4-6 % of the cellular components of the bone. Their morphological features are similar to protein-synthesizing cells - they have a well-developed endoplasmic reticulum and a Golgi apparatus. Osteoblasts have membrane receptors for parathyroid hormone, which is secreted by the parathyroid glands.
- Osteoclasts– are large multinucleated cells that develop from monocyte precursors. They carry out bone resorption.
- Osteocytes– Flat cells with numerous growths and connections between them. They are densely distributed in the bone matrix, originate from osteoblasts and account for 90-95 % of bone cells. Osteocytes are among the longest-lived cells, with a lifespan of up to 25 years. After mechanical stimulation, osteocytes produce several secondary mediators such as ATP, nitric oxide, Ca 2+ and prostaglandins (PGE2 and PGI2), which influence bone physiology.
Bone formation occurs through activated osteoblasts. They synthesize components of the extracellular matrix – type I collagen, glucosaminoglycans, protoglycans, osteocalcin, osteonectin and sialoprotein. Osteoblasts are rich in alkaline phosphatase. Collagen is secreted in the form of collagen monomers, which quickly polymerize into collagen fibers. The collagen fibers form an organic matrix in which calcium salts are stored. This is how osteoid tissue is formed. Once some osteoblasts have formed, they become embedded in it and become osteocytes. Calcium salts initially deposit as amorphous (non-crystalline) components, which then form hydroxyapatite crystals through substitution and addition of atoms, resorption and deposition. These processes form the initial mineralization. Complete mineralization occurs after a few months. Then the osteoblasts stop their secretory activity and transform into osteocytes. Normal plasma calcium and phosphate concentrations are required for normal mineralization. This process depends on the active form of vitamin D3. Parathyroid hormone reduces collagen formation by osteoblasts, and cortisol inhibits the maturation of preosteoblasts and their transformation into mature osteoblasts. Exercise stimulates osteoblast activity and bone calcification. Some calcium salts remain in an amorphous state (without a crystal structure). This is important because these salts are used in ECT to quickly extract calcium from bone. They represent exchangeable calcium (0.5-1.0 %), which is always in equilibrium with Ca 2+ in the ECT. Calcium metabolism is involved in rapid buffering mechanisms to maintain a constant plasma concentration of this mineral. The osteocytes are connected to each other by a series of outgrowths that attach them to the bone surface and also to the osteoblasts. They are arranged in concentric layers in the bone matrix. This arrangement creates the conditions for Ca 2+ transport from the interior of the bone to the bone surface and from there into the ECT. This transport by osteocytes is called osteocytic osteolysis. It leads to the removal of calcium from the newly formed crystals and does not result in a reduction in bone mass. Osteocytes are associated with rapid changes in plasma calcium concentration. They have osteolytic properties associated with short-term bone remodeling. Osteoclasts are large multinucleated cells with numerous mitochondria, lysosomes and a well-developed Golgi apparatus. They are rich in acid phosphatase. Bone resorption occurs on the surface of its coagulated membrane. The osteoclasts secrete organic anions (citrate), which increase the solubility of the mineral phase, and citrate. They realize the intercellular transport of calcium and sodium. Their lysosomes contain proteolytic enzymes that, when released, affect the organic matrix and the acids released from the mitochondria - citric and lactic acid. Extracellular matrix components are degraded by extracellular collagenases, proteoglycanases and proteolytic cathepsins. The resorption processes of the bone matrix lead to the destruction of the matrix, the reduction of bone mass and the release of calcium. Bone resorption by osteoclasts is associated with long-term bone remodeling. Bone tissue is characterized by high functional activity. At any given time, approximately 20 % of bone mass is undergoing a repair process, known as remodeling. It is a process of continuous bone resorption followed by new matrix formation and mineralization. Bone mass increases during the growth period as the formation processes predominate. The balance between formation and resorption stabilizes bone mass until the age of 50. Afterwards, resorption predominates and the total bone mass slowly decreases. Remodeling maintains normal bone and tooth strength. The rate of resorption and remodeling is high in childhood and much lower in old age. This is because bones are less brittle in childhood than in adulthood.
Stages of formation of normal hand bones
The bones of the wrist, metacarpals and phalanges make up the skeleton of the hand. These bony structures are connected to each other by various joints. The long and short muscles of the hand are connected to the bony structures of the wrist by tendons and enable the unique movements of the fingers and the hand as a whole. In addition to these three main bone groups, the hand skeleton also contains sesamoid bones.
The carpus is located between the distal edge of the pronator quadratus and the carpal joints. The carpus is arcuate – concave at the front and convex at the back. Its bony structures include the distal ends of the radial and ulnar bones and the eight carpal bones, which form two rows of four bones each, with the navicular bone serving biomechanically as a link between the two rows. The proximal row consists of the scaphoid, crescent, and triangular bones, which run inward and outward. This row connects proximally to the distal part of the radius bone and to the triangular fibrocartilage complex and forms the carpal and carpometacarpal joints. The distal to proximal carpal row fuses with the distal carpal row to form the medial carpal joint. The carpal bone is located in front of the other three proximal carpal bones and is a sesamoid bone. It forms one of the attachment points for the flexor carpi ulnaris tendon, which acts as the ulnar stabilizer of the hand. In the same order (from outside to inside), the distal row consists of the large polygonal bone (trapezoidal bone), the small polygonal bone (trapezoidal bone), the parietal bone and the hook bone. The carpal bones are held together by ligaments. The bones of the distal carpal row are more evenly distributed than those of the proximal carpal row, especially in the area of their distal connection with the metacarpals.
Muscular structure of the hand
The muscular skeleton of the hand is divided into two large groups - the shoulder and the free upper extremity.
The shoulder crown consists of the following muscles:
- Deltoid muscle.
- Adductors.
- Subacromial.
- Small circular muscle.
- Large circular muscle.
- Sublumbar.
Structure of the muscle
The muscles of the arm form the free top:
- Shoulder blade.
- Forearm.
- Poor.
The muscles of the forearm.
Summary
The human body is a very complex system, and each organ, bone or muscle has a specific place and function. The bones of the hand are a part of the body that consists of many joints that allow it to move and lift objects in various ways.
Thanks to evolutionary changes, the human hand has acquired unique abilities that are incomparable to those of other primates. The peculiarity of the structure of the hand has given humans an advantage over the animal world.
Read more:- Sesamoid bone of the hock.
- Sesame legs of the hock.
- What is the connection between the femur and tibia?.
- structure of the toes.
- The lateral dislocation is.
- metatarsal and metacarpal bones.
- Dislocation of a bone in a joint.
- Bones of the tarsal bone of the hand.
