Most calcaneus fractures result from high-energy trauma, e.g. B. by an accident or a fall from a great height. Sports injuries, particularly snowboarding injuries, are another, but less common, cause of ankle bone injuries.

- RU2431449C1 - Procedure for surgical access to the heel bone - Google Patents
- Pictures
- Diagnosis
- differential diagnosis
- Development
- Because the ankles originally
- diagnosis
- Surgery for aseptic necrosis of the heel bone
- surgical treatment
- pain management
- Do I really need rehabilitation?
- When can rehabilitation begin?
- X-ray examination
- CT and MRI
- CLASSIFICATION OF OSTEOCHONDRIAL DEFECTS OF THE ANKLE BONE.
- CONSERVATIVE TREATMENT
- SURGICAL TREATMENT OPTIONS
- etiology
- Clinical Features
- Anatomy of the ankle
- Treatment of dissecting osteochondritis of the heel bone
- The tarsal bones
- Proximal row of tarsal bones
- talus
- Latin terms from this lesson:
RU2431449C1 - Procedure for surgical access to the heel bone - Google Patents
Publication number RU2431449C1 RU2431449C1 RU2010120733/14A RU2010120733A RU2431449C1 RU 2431449 C1 RU 2431449 C1 RU 2431449C1 RU 2010120733/14 A RU2 Authority RU Russia tags Talar osteotomy ankle posteromedial anteromedial state of the art 2010-. 05- 24 Application number RU2010120733/14A Other languages English ( de ) Inventors Gennady Mikhaylovich Kavalsky (RU) Gennady Mikhaylovich Kavalsky Andrey Roaldovich Drogin (RU) Andrey Roaldovich Drogin Anatoly Dmitrievich Chensky (RU) Ruslan Akhmadovich Bakir. (EN) Ruslan Akhmadovich Bakir Yuri Mikhailovich Kashurnikov (RU) State Educational Institution of Higher Professional Education First Moscow State Medical University named after IM Sechenov М. Priority Date (The priority date is an assumption and does not constitute a legal conclusion. Google has not conducted a legal analysis and does not guarantee the accuracy of the date provided). 2010-05-24 Submission date 2010-05-24 Publication date 2011-10-20 2010-05-24 Submission by IM Sechenov First Moscow State Medical University of Higher Professional Education of the Ministry of Health and Social Development of the Russian Federation (IM Sechenov First Moscow State Medical University of the Ministry of Health and Social Development of the Russian Federation) submitted to the Critical State Educational Institution of Higher Professional Education. 2010-05-24 Priority to RU2010120733/14A Priority Critical patent/RU2431449C1/ru 2011-10-20 Application granted Critical 2011-10-20 Publication RU2431449C1 Publication Critical patent/RU2431449C1/ru
Pictures
The invention belongs to the field of medicine, in particular traumatology and orthopaedics, and can be used to perform a surgical approach to the waist. In this case, an osteotomy is performed in two planes. One level of the osteotomy runs through the medial malleolus. The second plane is at an angle of 60° to 90° to the first plane and includes the medial portion of the anterior or posterior edge of the distal articular surface of the tibia. This is due to the need to visualize either the antero-medial or posterior aspect of the talus or the entire talus. Use of the present invention allows for a comprehensive view of the talus, including the antero-medial and posterior-medial aspects and the entire talus. 2II
Diagnosis
List of the main and additional diagnostic measures:
Outpatient primary (mandatory) diagnostic tests:
– X-ray of the foot or ankle in two projections (straight and lateral).
Additional outpatient diagnostic tests (if indicated):
– CT scan of the talus;
- OAC;
- TAC; OAB;
– ECG;
– microreaction;
- blood glucose test, if indicated;
- determination of the clotting time;
- Determination of bleeding time;
– Blood chemistry: total bilirubin, ALT, AST, urea, creatinine, total protein.
Minimum list of examinations to be performed upon admission to a planned hospital: According to the internal regulations of the hospital, taking into account the current regulation of the competent health authority.
Basic (mandatory) diagnostic tests performed at the inpatient level:
- OAK;
– X-ray of the ankle or foot in two projections (anterior and lateral).
Additional in-hospital diagnostic tests (if indicated):
- OAM;
– X-ray of the foot in oblique projection;
– CT scan of the talus
– determination of blood group;
- determination of the Rh factor;
– microreaction;
- blood glucose determination as indicated;
- determination of the clotting time;
- Determination of bleeding time;
– ECG;
– Blood chemistry: total bilirubin ALT, AST, urea, creatinine, total protein.
Diagnostic measures carried out in the emergency phase:
– Collection of complaints and anamnesis, physical examination.
Diagnostic criteria for diagnosis:
Complaints.(a) pain in the foot or
– pain in the foot and ankle;
– dysfunction of the lower limbs;
– Presence of open fracture wounds.
differential diagnosis
Treatment goals:
– elimination of displacement of bone fragments;
– Restoration of limb function.
Treatment tactics:
Conservative treatment is indicated for fractures without displacement and fractures with displacement but satisfactory alignment of the fragments. For fractures with displacement, a fracture block, closed one-stage manual reduction of the fragments, a plaster splint, and a control radiograph should be used. If the control x-ray still shows displaced fractures, surgical treatment is indicated.
Non-surgical treatment:
Scheme depending on the severity of the disease – 1, 2, 3.
Diet – Table 15.
Depending on the pathology that exists at the same time, other types of diets are prescribed.
Pharmacological treatment:
Table 1. Medications for heel bone fractures
| № | medication | dosage | duration of use | level of evidence |
| block preparation | ||||
| 1 | procaine | |||
Other types of treatment: [7].
Other types of treatment performed on an outpatient basis:
– novocaine blockade at the fracture site;
– Closed manual reduction of the fracture in one step for displaced fractures;
– applying a plaster cast;
– Orthopedic aids and splints.
Other inpatient treatment:
– novocaine blockade of the fracture site;
– Closed reduction for displaced fractures;
- Plaster cast;
– Orthopedic devices and splints.
Other treatments in the emergency medical phase: splinting
Development
In the 7th to 8th intrauterine month, an ossification center develops in the ankle.

From left to right: fracture of the femoral neck, shaft and posterior process of the ankle bone
The ankle bone is not well supplied with blood. Because of this, a broken bone may take longer to heal than most other bones. A person with a broken ankle bone may not be able to walk without crutches for several months and may need to wear a cast or shoe.
Ankle bone injuries can be difficult to detect, and fractures of the transverse processes in particular can be hidden radiographically. If a heel bone fracture is not recognized and treated appropriately, it can lead to complications and long-term damage. A 2015 review found that isolated calcaneus fractures may be more common than previously thought.
A fracture of the ankle bone is often associated with a dislocation that is best visualized by computed tomography. When a talus fracture is associated with a dislocation, restoring joint and axis alignment is essential to optimizing ankle and hindfoot function.
Because the ankles originally
Dice were originally made from the talus of ungulates, leading to the nickname 'dice' for dice. They are also known as 'fists' and are roughly four-sided. Modern Mongolians still use such dice as shagai for games and divination, each piece having a symbolic meaning.
The tibia appears to have arisen from the fusion of three separate bones on the feet of primitive amphibians: the tibia, which articulates with the tibia, the intermediate piece between the base of the tibia and the fibula, and the fourth medial bone, which is in the middle of the tarsus lies. In modern amphibians, these bones are still partially separated, so they do not have a true talus. The ankle bone forms a much more flexible joint in mammals than in reptiles. This is most evident in cloven-hoofed mammals, in which the distal surface of the bone has a smooth keel that allows the foot greater range of motion, thereby increasing running speed.
diagnosis
Examination for suspected aseptic necrosis of the talus of the ankle begins with a visual examination. The doctor assesses the condition of the skin and the alignment of the foot and gently palpates the foot. Instrumental examinations can confirm the diagnosis:
Also, a series of basic laboratory tests are performed to determine the patient's general health, identify any inflammatory processes in the body, and assess the hematopoietic system.
Take advantage of this unique opportunity for a free consultation on your planned treatment. Continue reading.

Surgery for aseptic necrosis of the heel bone
The treatment depends entirely on the severity of the disease. In stages 3 to 4 of aseptic necrosis with severe damage to the integrity of the plate, conservative management is not indicated and surgical intervention is indicated.
Aseptic necrosis is quite a complex pathology, and the choice of surgical treatment in the later stages is limited to two optimal methods.
- endoprosthetics. With this technique, the damaged areas of the plate are fully or partially replaced with a biocompatible artificial material.
- arthrodesis. With this technique, the damaged area is fixed in a fixed position.
For minor lesions, osteochondral autoplasty, tunneling of the necrotic area, and alloplasty are possible.
surgical treatment
With displaced fragments, only internal stabilization achieves the best results and avoids the risk of future complications.
Open reduction and internal fixation. In this operation, the bone fragments are first returned to their normal anatomical position, and then fixed with special screws or metal plates and screws.


(Left) An x-ray shows a fracture of the talus. (Right) The bone fragments have been fixed with screws.
Bone tissue has a very high ability to regenerate. However, the more severe the injury, the longer the healing time can be. After the operation, the foot and ankle are immobilized for 2-8 weeks, depending on the type of injury and the expected potential for regeneration. During the treatment, the doctor will most likely take some x-rays to make sure the healing process is going according to plan.
pain management
You will experience some level of pain after the operation. This is an essential part of the healing process. The doctor and nurse will do everything they can to relieve the pain and speed up your recovery.
Many experts recommend starting foot and ankle movement as early as possible, based on the pain felt. In patients who have undergone surgery, it is usually recommended to start exercise once the wound has healed. With conservative treatment, regaining mobility of the foot and ankle usually begins once immobilization is removed.
Do I really need rehabilitation?
The greatest danger with a talus fracture is the high risk of late complications. Unpleasant results after injury are due to a poor treatment regimen and the lack of timely, competent rehabilitation.
- Compartment syndrome (increased tissue pressure in the fascial space)
- lack of bone healing
- persistent pain
- Post traumatic arthritis
- deformed arthritis
- Foot deformity (heel flare, flat feet)
- osteonecrosis
- Significant restriction of mobility
When can rehabilitation begin?
If the fracture is treated conservatively, rehabilitation begins the day after the injury. Early comprehensive rehabilitation is recommended for patients who have undergone osteosynthesis surgery. This depends on the type of injury, the severity of the condition, and the reconstruction technique used.
Complete healing of the ankle bone takes 3-6 months. In particularly severe cases, the recovery time can take up to a year.
X-ray examination
Routine x-rays include plain and lateral x-rays of both ankles. X-rays may show a detached bone fragment. In the early stages of the disease, the area of damage can be so small that it is not visible on x-rays. Sometimes, over time, the lesions are only visible on the x-ray.

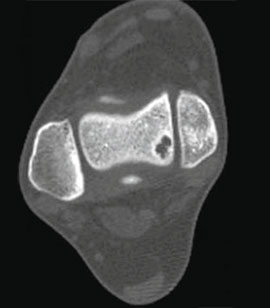
CT and MRI
However, computed tomography (CT) is preferred for preoperative planning. A CT scan includes a 0.5mm image with a 3D reconstruction of the affected joint. MRI is helpful in diagnosing associated soft tissue injuries (muscles, ligaments, and tendons).


CLASSIFICATION OF OSTEOCHONDRIAL DEFECTS OF THE ANKLE BONE.
Stage I: mild compression fracture.
Stage III: complete detachment of the fragment with dislocation.
CONSERVATIVE TREATMENT
Asymptomatic or minimal damage is treated conservatively: rest, ice, temporary weight-bearing, and orthotics for unstable joints.
SURGICAL TREATMENT OPTIONS
Several surgical techniques are available for the treatment of osteochondral injuries of the ankle. They are all usually based on one of the following principles:
- Bone marrow debridement and stimulation (microfracture, abrasion chondroplasty, perforation); New articular cartilage grows by releasing stem cells from the medullary canal into the defect area.
- reattachment of the detached cartilage fragment to the talar block if large;
- stimulation of articular cartilage formation by implantation of endogenous chondrocytes;
- Relocation of cartilage from the knee joint (mosaic chondroplasty) or replacement of the defect with artificial cartilage.
etiology
In 1865, the surgeon Munro was the first to describe the presence of free particles in the joint that should not normally be present there. He discovered the blood cells in the ankle joint, observed the patient and described what happened at that time very precisely. The term dissecting osteochondritis corpus callosum was given in 1888 by another doctor who observed her knee joint.
The exact origin of the disease has not yet been clarified. The disease often develops as a result of trauma. However, there are also patients who have not suffered trauma to the ankle but have abnormal blood cells.
The medial aspect of the talus is primarily affected by frequent, repetitive trauma. Various endocrine disorders, microemulsification and growth peculiarities of the body may also play a role.
The hip block area is also most commonly damaged by trauma. This happens e.g. B. in supination, which must be combined with internal rotation and forced flexion.
Involvement of the medial portion of the talar block is also possible with external rotation.
Clinical Features
Symptoms of the disease are similar in both children and adult patients. In the beginning, when the disease is just beginning to develop, the sufferer does not pay attention to small changes in their mood.
As the disease progresses, symptoms in the ankle joint appear first. These are worse when walking, making sudden movements and being in awkward positions. As dissecting osteochondritis progresses, the symptoms increase in duration and intensity, becoming distressing with little or no exertion. In some cases, there is swelling of the affected joint and pain when palpating the problem area.
Necrotic bone tissue gradually detaches from the main bone mass. These particles are called 'joint mice'. When a detachment occurs, the sufferer complains of a grinding sensation with movement, a feeling as if the joint is 'stuck' in the middle of an activity.
In some patients, the joint becomes blocked due to the presence of joint mice. When this happens, the joint becomes 'pinched' and the ability to move in any direction is lost. This is accompanied by an acute attack of pain that is difficult to ignore.
Anatomy of the ankle
The talus is part of the foot and ankle. Fractures occur in the upper part of the ankle bone and are rarely diagnosed in other parts.
The upper part of the ankle bone is covered with cartilage. This cartilage is very thin, no more than 3 mm. However, it is completely flat, which is necessary to reduce friction.
When the ankle bone is broken, the ligaments in that part of the joint are usually stretched as well.
When the cartilage and bone are severely damaged. This can cause bone and cartilage fragments to tear off. This in turn leads to a 'joint mouse' developing in the joint cavity.
The consequence of this condition is impaired blood circulation and necrosis, which begins in the dislocated part.
It is clear that ankle injuries require prompt and appropriate treatment.
The general symptomatology of the pathology resembles that of a sprained ligament.
There is always severe pain, which increases when the sufferer puts weight on the injured leg.
The joint may be swollen. There are no other specific symptoms.
The diagnosis of osteochondritis talus dissection can only be confirmed by an x-ray of the joint.
If there is a foreign body in the joint, a cracking sound can be heard during movements and the patient may complain of stiffness.
After a conversation with the patient and a detailed anamnesis, the orthopedist examines the painful leg and feels it. He then refers the patient to an X-ray examination.
If the specialist is not sure about the diagnosis, he can also recommend an MRI or CT scan.
He may order an additional MRI or CT scan.
Treatment of dissecting osteochondritis of the heel bone
There are two ways to treat the problem: conservative and surgical.
In the acute phase, the joint is immobilized with a rigid plaster cast for 1-1.5 months.
During this time, the patient is dependent on crutches to move around.
Cold compresses are recommended for 3-4 days to relieve pain and swelling.
In addition, the affected limb must be elevated.
The doctor also prescribes a course of nonsteroidal anti-inflammatory drugs.
Surgical intervention is indicated when general symptoms persist for several months.
Surgical intervention is required even if a mouse is in the joint cavity.
It must be removed and tunneling (small channels drilled into the bone tissue) performed.
Over time, these ducts become filled with tissue and blood vessels to improve blood supply.
Scar tissue is formed in place of the detached cartilage to cover the defects.
In Israel, such an operation can be performed by arthroscopy. If arthroscopy is not possible, an arthrotomy, i.e. opening the joint, is necessary.
In dissecting osteochondritis of the talus, the sutures are removed after about two weeks.
After the operation, the patient has to walk on crutches for about a month to relieve the joint.
It is important to train the operated part of the body with special exercises.
Physiotherapeutic treatments are also required during the rehabilitation period.
The tarsal bones
There are seven cheekbones arranged in two rows - proximal and distal. These two series are very different, that's for sure. In this photo I have highlighted the proximal row of tarsal bones in yellow and the distal row in blue.
Proximal row of tarsal bones
The proximal row of tarsal bones is made up of just two bones: the talus and the heel. The maximum weight of the entire body rests on these two bones, which is why they are very hard and strong.
talus
The talus is a bone that articulates with four bones – the top of the tibia and fibula connect to it, the bottom connects to the heel bone, and the front connects to the scapula.
If you think of a bone as something long and oblong with two articulating surfaces at the ends, forget that cliché for this lesson. The talus is a small rod made entirely of articular surfaces.
This is its position in the foot (side view):
The talus can also be found as part of the foot skeleton when viewed from the medial side:
The talus consists of. the body (corpus talus), the neck (Collum tali) and Head (caput tali). In this drawing, the corpus tali is shown in blue, the neck in yellow, and the head in orange.
Latin terms from this lesson:
- pes;
- Tarsus;
- metatarsus;
- ossa digitorum;
- talus;
- corpus tali;
- collum tali;
- caput tali;
- Facies superior ossis tali;
- trochlea tali;
- facies malleolaris medialis;
- facies malleolaris lateralis;
- Processus lateralis tali;
- medial tubercle;
- Tiberculum laterale;
- Sulcus tendinis musculi flexoris hallucis longi;
- Sacies articularis calcanea posterior;
- sulcus tali;
- facies articularis navicularis;
- tuber calcanei;
- facies articularis cuboidea;
- Facies articularis talaris posterior;
- facies articularis talaris media;
- Facies articularis talaris anterior.
I'll cover the other bones of the foot in the next lesson so my articles don't get too long. At the end of this lesson, I want to draw your attention to the fact that all the bones of the foot are very dense and have many surfaces that connect to each other.
As you study the anatomy of each bone, pay special attention to the articular surfaces and to which surfaces of other bones they are connected. This is the most important thing you should know about this topic.
Read more:- Anatomy of the pelvic bones.
- metatarsal bones.
- Displacement fracture of the heel bone.
- Fracture of the heel bone.
- pelvic bones.
- Anatomy of the heel bone.
- fibula.
- Fracture of the calcaneus of the foot.


