In emergency procedures, intubation or endotracheal anesthesia is performed. In elective procedures, general or local anesthesia is used.

- Amputation; disarticulation
- amputation methods.
- is reamputation.
- Further information
- Limb Rescue Center from Gangrene
- QUESTIONS AND ANSWERS
- A reamputation is…
- More information on the topic
- Premature residual limb pain
- Gangrene Limb Rescue Center
- QUESTIONS AND ANSWERS
- amputation techniques
- single flap
- Two-sided stump
- Guillotine (one-shot technique)
- Two-stage surgery
- Three-stage tapered circular amputations.
- Postoperative Complications.
- phantom pain
- Psychological care
- types of amputation
- initial prosthetics
- is reamputation
- Types of amputation cuts
- Guillotine amputation
- Advantages of our clinic
- Further management after tibial amputation
- Advantages of our clinic
- Postoperative pain
- ischemia of the stump
- causes
- diagnosis
Amputation; disarticulation
An amputation is the segmental removal of a limb. Severing the limb at the level of the joint is called disarticulation or disarticulation. These operations should be considered as a complete surgical treatment of the patient. They are carried out when other treatments are ineffective or impossible.
1. Traumatic limb damage: extensive crushing of a segment with non-viable tissue, detachment of a limb segment when it cannot be reimplanted or its absence does not appreciably impair limb function (distal phalanges, fingers IV-V, etc.). After a traumatic avulsion, primary surgical treatment of the wound with the creation of a stump is performed.
2. Post-traumatic toxemia, which is untreatable and life-threatening.
3. Acute purulent processes on the limbs (anaerobic infection, sepsis).
4. chronic purulent processes of the limbs, which are debilitating and carry the risk of amyloidosis of internal organs (kidneys) or neoplastic fistulas (about 10 % of patients with chronic osteomyelitis), trophic ulcers.
5) thrombosis and embolism when blood flow cannot be restored or when there is evidence of degenerative necrosis of limb tissues.
6. the gangrene of sections of the limbs due to vascular insufficiency (arteritis, diabetes mellitus), frostbite, burns of the fourth degree (sometimes with arteritis, amputation is performed before the appearance of tissue necrosis due to severe ischemic pain that exhausts the patient).
7. Malignant tumors of bones and joints.
8. Irreversible congenital and acquired orthopedic deformities when the appropriate prosthetic function of the limb is markedly improved after amputation.
If, in view of the severity of the operation and the associated great responsibility, there are doubts as to whether an amputation should be carried out, this should be decided by a council. Before the operation, the patient is informed about the reasons for and the necessity of the amputation and about the prosthetics and his social rehabilitation. If the patient does not agree to the amputation and there are absolute indications that it will be necessary, the relatives should be informed about the possible consequences.
amputation methods.
1. Guillotine amputation: severing of the entire tissue of the limb, including the bone, at the same level. This is an old amputation method from before the introduction of anesthesia. It is no longer used today because the wound abscesses and takes a long time to heal, the soft tissue shrinks and the bone is still protruding even after the wound has healed, so that another amputation is required (repeat amputation).
2. Periprosthetic amputation, which differs from guillotine amputation in that the wound is sutured and the bone closed. Using the three-stage circular amputation method according to NI Pyrogov (skin and fascia cut at one level, muscle slightly higher and bone even higher), the edges of the skin are sutured without tension, the scar is mobile but large, and the wound heals with secondary tension. In most cases, such residual limbs are not suitable for prostheses.
3 The clavicle amputation technique is the most rational and commonly used technique. Advantages: the dissection is performed in such a way that the surgical scar cannot be inserted into the prosthesis and the wound can heal in better conditions. Reconstructive interventions are not necessary after using this technique.
A distinction is made between a closed and an open collarbone amputation. In the case of a closed amputation, the wound is sewn up after the operation. It is used in elective surgeries when there is no risk of abscess formation. Classic fasciocutaneous flaps are applied to shape the residual limb to its normal shape.
The open flap method is used for all open trauma where there is a risk of infection and purulent inflammation.
After the amputation, the wound is closed or the stumps are only connected with individual guiding sutures. Once the wound has 'settled', repeat sutures are placed.
4. fasciomyoplastic amputation; it is used to improve cross-sectional bone coverage and to maintain physiological muscle tone and strength. The most common amputation (by calendar) is the transfemoral amputation. This type of amputation gives the patient the opportunity to undergo prosthetic fitting and regain function when the time comes.
is reamputation.
Limb rescue
with technologically advanced methods
- Vascular and cardiac diseases
- Dry gangrene
- critical ischemia
- Diabetic foot
- Atherosclerosis and its treatment
- Obliterating arteritis
- Arterial thrombosis and embolism
- Popliteal artery aneurysm
- Removal and dissolution of thrombi
- Carotid Artery Surgery
- Aorto-femoral bypass surgery
- Carotid artery stenting
- Microsurgical shunts on the lower leg and foot
- angioplasty and stenting
- amputations due to gangrene
- High risk surgery
- Treatment of ulcers and bedsores
- Clinical examination
- ultrasound examination
- Computed Tomography
- Subtractive angiography
Further information
Hand and body strengthening exercises are best started before the amputation. They promote the skills needed to move from bed to wheelchair, go to the toilet, and maintain fitness for learning to walk, which is done with or without prostheses.

Limb Rescue Center from Gangrene
Moscow region, Klin city, Pobieda street, pos. 2
QUESTIONS AND ANSWERS
My husband is going to have his hip amputated, they say there's no chance.
The answer: This is our profile. Please send us photos of your foot and a discharge form to [email protected] and we will try to help you.
Hello, I'm on hemodialysis, my fistula was sewn up incorrectly, there was a bandage and the toe couldn't be saved, gangrene set in. It was possible to restore blood flow, but I was sent home to St. Petersburg to wait until he amputated on his own. Now he is gone.
Answer: Yes, we can solve everything. The cost of treatment is 190 rubles.
Hello, my mother is 79 and they had 2 toes amputated but the gangrene has spread to half of the foot, the doctors say she needs an amputation above the knee. She's already had vascular surgery, but she didn't make it to the knee.
Answer: Send a photo of the foot and the data of the vascular examination to [email protected]. Maybe we can save the leg from amputation.
Feasibility of a reconstructive operation on the left renal arteries with evidence of fine-spotted hemorrhagic erosions on endoscopic examination.
Could you tell me in which cases the shunt closes so soon after surgery and what are the next steps? Will another operation be required? Thank you very much for your answer
Answer: If the shunt recurs, blood flow must be restored.
Hello, can you please advise me. 3 months ago I had bypass surgery on my leg. After the operation I felt better. My leg is cold again and hurts like before. What can be the reason?
A reamputation is…
Limb rescue
With technologically advanced methods.- vascular and heart diseases
- Dry gangrene
- Critical cerebral ischemia
- Diabetic foot
- Atherosclerosis and its treatment
- Obliterative arteritis
- Arterial thrombosis and embolism
- Popliteal artery aneurysm
- Removal and dissolution of thrombi
- Carotid artery surgery
- Aortic Femoral Bypass Surgery
- Carotid artery stenting
- Microsurgical shunts on the lower leg and foot
- angioplasty and stenting
- amputations due to gangrene
- High risk surgery
- Treatment of ulcers and bedsores
- Clinical examination
- ultrasound examination
- Computed Tomography
- Subtractive angiography
More information on the topic
Premature residual limb pain

Gangrene Limb Rescue Center
Moscow Region, Klin, 2 Pobedy Street
QUESTIONS AND ANSWERS
My husband is going to have his hip amputated, no chance they say... Burger's disease, he's in terrible pain, gangrene in his foot.
Answer: This is our profile. Please send photos of your foot and discharge to [email protected], we will try to help you.
Good morning, I'm on hemodialysis, the fistula was sewn up incorrectly, there was a theft, they couldn't save my toe, gangrene happened. They managed to restore blood flow, but in St. Petersburg they sent me home to wait for spontaneous amputation. Now it's gone.
Reply: Yes, we can solve everything. The cost of treatment is 190 rubles.
Hello, my mother is 79 years old and they had 2 toes amputated but the gangrene has spread to half of her foot, the doctors say she needs an amputation above the knee. She's already had vascular surgery, but she didn't make it to the knee.
Answer: Send a photo of the foot and the data of the vascular examination to [email protected], maybe the foot can be saved from amputation.
There is a possibility of reconstructive surgery on the left renal arteries with signs of small-point hemorrhagic erosions on endoscopic examination.
Could you tell me in which cases the shunt closes so soon after surgery and what are the next steps? Will another operation be required? Thank you very much for your answer
Answer: Blood flow must be restored if the condition recurs.
3 months ago I had bypass surgery on my leg. After the operation I felt better. Now my leg is cold again and hurts like before. What can be the reason?
Answer: It could be a closed shunt.
Hello, I have a closed aortic femoral bifurcation prosthesis, the operation was performed on 03/28/2017, can the prosthesis be replaced?
amputation techniques
Depending on the technique of external tissue cutting, operations are divided into two types - lobectomy and circumferential surgery.
single flap
After excising the damaged portion of the limb, the sawbone is closed with a flap of tissue made up of fascia, skin, and tissue. The edge of the stump resulting from the operation has the shape of a torpedo or a tongue.
During surgery, the surgeon 'cuts out' the soft tissue fragments leaving the scarring on the outside of the residual limb to which the prosthesis will be attached.
Two-sided stump
After the amputation, the open wound is closed with two soft tissue flaps cut from opposite sides of the leg. When calculating the required flap length, the following factors are taken into account:
In contrast to the surgical method described above, the two-lobe operation is more labor-intensive. Due to this method of closure of the ball bone, complications are rare.
Guillotine (one-shot technique)
During the operation, the soft tissue at hip level is loosened in a circular motion and the bone is sawn off. This amputation technique is more commonly used in emergency surgery patients, which may be related to:
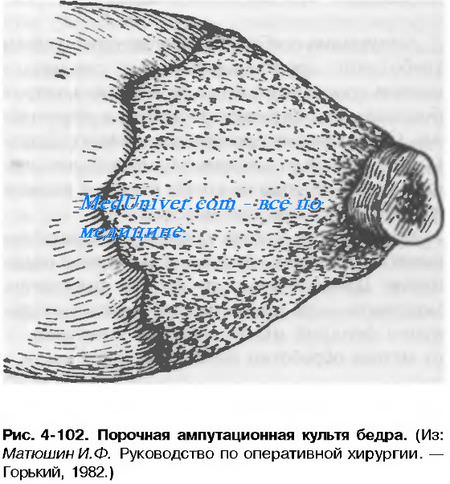
A significant disadvantage of one-stage surgery is the formation of an abnormally shaped, pointed stump, in which case secondary surgery is indicated.
Two-stage surgery
Removal of the injured part of the limb and filing of the bone is a two-step process:
- Dissection of the skin, subcutaneous tissue, and muscle mantle with subsequent displacement proximal to the limb.
- Severing the muscle fibers along the edge of the stretched tissue and sawing through the bone.
A major disadvantage is the formation of skin folds on the residual limb, which later have to be surgically removed.
Three-stage tapered circular amputations.
Amputations are performed in areas of the leg where there is only one bone. The three-stage Pirogov amputation is carried out in several stages:
Postoperative Complications.
Approximately 23 % patients experience one of the following complications during the rehabilitation period:
- soft tissue necrotization;
- pre-infarction status;
- hospital-acquired pneumonia;
- bacterial wound inflammation;
- recurrence of chronic gastrointestinal diseases;
- thrombosis of blood vessels;
- cerebral circulatory disorders.
Patients receive antibiotic therapy and physical therapy to prevent adverse effects. Massage, breathing exercises and physical therapy reduce the risk of lung disease and soft tissue congestion.
phantom pain
The pain that occurs with an amputated limb is called phantom limb pain. Its true cause is unknown and therefore there are no etiotropic or pathogenetic methods of its treatment. Typical manifestations of pathology are:
Antidepressants and tranquilizers are used to relieve symptoms. They reduce the severity of symptoms and prevent patients from developing depression. The use of limb development and exercises with a prosthesis is indicated to speed up the elimination of the postoperative complication.
Psychological care
Well-organized psychological care before and after the operation accelerates acceptance and getting used to the prosthesis. Timely support and attention from relatives shortens the rehabilitation period and has a positive effect on the patient's psycho-emotional well-being.
A positive attitude reduces the likelihood that the missing limb will hurt and other postoperative complications will occur. Experts believe that this is due to the lack of factors that negatively affect the functioning of the nervous system. During recovery, it is advisable to follow the doctor's orders and not to think about impairments.
types of amputation
- Emergency amputation 'guillotine. It is performed on vital signs when the border of the dead tissue cannot be accurately determined. In this case, the leg is simply crossed over the visible lesions. Once the inflammation has subsided (5-10 days), another amputation is performed to create a stump for a later prosthesis.
- Primary' amputation. This type of amputation is performed when blood flow to the lower limbs cannot be restored. Thanks to the development of microsurgery in our clinic, this type of amputation is very rarely performed, since in the vast majority of cases it is possible to restore blood circulation in the affected limb or lower leg.
- Secondary amputation performed after vascular reconstruction, usually at a lower level, or when vascular reconstruction surgery has failed. Since the leg does not grow back, attempts should always be made to save it, but these attempts are not always successful. In our clinic, vascular surgical interventions are often carried out in a targeted manner in order to avoid amputations.
1. Express shaping of the residual limb by bandaging with a special bandage or elastic sleeve - 3 days
2. Preparation of a temporary prosthesis on day 4 with a special residual limb support bandage and a mechanical device from Ortho-Cosmos.
3. Physical fitness and gait training with a temporary prosthesis by a qualified instructor.
4. Stanislav Milov, surgeon and head of the rehabilitation center (+7 967 213 20 18) is responsible for wound care and removal of the sutures on days 12 to 14 after the amputation.
5 Once the sutures are removed, we can take the patient to Ortho-Kosmos for a consultation and to measure the initial prosthesis.
initial prosthetics
Amputation does not mean helplessness for people who have a strong heart. The advanced prosthesis manufacturers of the 21st century are well acquainted with the possibilities of restoring walking function at a high level. Our partner, Ortho-Cosmos, is one of the leading prosthesis manufacturers in Russia. Our clinic helps patients learn to walk with a temporary prosthesis within a few days or weeks after the amputation.

Using the prosthesis, learning to walk and climbing stairs requires agile, flexible muscles. Pain, inactivity, and the trauma that caused the amputation weaken the muscles, requiring them to be strengthened before a prosthesis can be fitted. To start, each exercise should be done 10 times in two or three sets per day. Avoid holding your breath during exercises.
is reamputation
Indications for secondary amputations: extensive soft tissue injuries with bone fractures complicated by anaerobic infection; extensive purulent complications of long bone fractures with ineffective conservative treatment; purulent arthritis in injuries or when the inflammatory process started from the bony epiphyses, with the phenomena of intoxication and sepsis; repeated arterial bleeding from large vessels in large purulent wounds, development of sepsis and exhaustion of the injured person, ineffective conservative treatment; Necrosis of the limb as a result of obliteration or ligation of the main arterial trunks; Grade IV frostbite after necrectomy or rejection of necrophilic areas.
As can be seen from the list of indications above Indications for secondary amputationAs can be seen from this list of indications for secondary amputation, in each of them the development of infection is mentioned in one way or another. Amputation is only indicated when all options for combating the infection have been exhausted.
In peacetime are amputations is most commonly performed in arterial damage due to atherosclerosis and obliterative arteritis, as well as in cases of traffic accidents.
amputation Amputation consists of 4 main steps: transection of the skin and soft tissues; cutting of the bone; Prepare the wound, tie off the vessels, cut the nerves and close the wound.
Types of amputation cuts
Amputations are divided into circular and lobular amputations. Amputations are divided into circular and lobular amputations. Circular amputations Circumferential amputations are often performed on limbs where the soft tissue evenly surrounds the bone on all sides.
Circumferential amputations are divided into guillotine amputations, single stage, double stage and triple stage amputations.
Guillotine amputation
In a guillotine amputation All soft tissue and bone are cut through in one plane without the skin being pulled back beforehand.
Advantages of our clinic
At the Innovative Vascular Center, tibial amputation is the method of choice when a lower limb needs to be shortened, as we believe there will be minimal impairment of limb function. If the patient is potentially mobile and able to walk with a prosthesis, we aim to preserve the knee joint.
In order to have good practical results in lower limb amputations, our clinic has developed a technique to assess blood flow at the level of the amputation, and we apply methods of restoring blood flow through the femoral arteries to ensure good blood flow in the upper third of the lower limb to ensure.
Pirogov's reconstructive amputation technique, in which the residual limb is preserved with the help of the heel bone, is widely used in our clinic. This technique enables the patient to walk on their leg without a prosthesis.
For wet gangrene, we use the two-stage amputation technique. In the first phase we perform a guillotine amputation of the lower third of the tibia and once the inflammation has subsided we shape and close the residual limb. With this method we were able to avoid postoperative suppuration complications in the residual limb and maintain the maximum length of the residual limb.
Further management after tibial amputation
The vascular surgeon of our clinic treats the patient from the amputation to the fitting of the prosthesis. After discharge, we take the patient to a rehabilitation center for mobilization with lifting on crutches and walking, followed by a temporary adjustment of the prosthesis. For early prosthetics, we have established a cooperation with the prosthesis manufacturer Ortho-Kosmos, so that our patients receive temporary prostheses to learn to walk.
After rehabilitation, the patient must undergo ultrasound examination of the arteries and controls at a vascular surgeon in the clinic every six months. If residual circulatory disorders are found in the limbs, we recommend hospitalization and vascular revascularization.
Advantages of our clinic
The Innovative Vascular Center is unique in restoring blood flow to the limb in gangrene, which is why we rarely perform large amputations at the upper third of the thigh. The decision to amputate is made solely by a consortium of physicians after a thorough assessment of the perfusion and viability of the limb segment. If the limb segment is beyond salvage, we perform perfusion repairs and amputations at the lowest possible level.
In our clinic, the preferred surgical technique is the gritty amputation of the thigh with preservation of the kneecap. With these amputations, the patient can use lightweight prostheses and has a better quality of life. A gritty stump is good because the skin of the stump is not injured by bone chips, and trophic ulcers or ulcers never develop. The skin over the kneecap is the strongest and thickest. The Gritti Stump can be supported without risk of injury. The quality of the residual limb allows for maximum recovery and mobility. Other clinics rarely use this type of amputation because they don't want to complicate the operation or don't have experience in reconstructive plastic surgery.
Postoperative pain
A typical and unavoidable cause of pain is a surgical procedure that causes tissue trauma. With correct treatment, this pain subsides relatively quickly once the wound has healed. This process can take between three and six months.
Improper handling of the nerve trunks during surgery, along with accumulation of fluid at the surgical site, leads to skin infection. Another cause is the storage of the residual limb in the vagina. This creates a moist environment that is very conducive to the spread of bacteria and fungi. In addition to abscesses, inflammation and an unpleasant odor, those affected often develop fever and subfebrile conditions. The infection can lead to laceration of the wound, so these patients need urgent treatment.

Medical treatment in such cases consists of cleaning the injured part of the body, as well as using antibiotics such as Diclofenac and Analgin. In some cases, additional surgery is required. Wearing a prosthesis in the presence of an infection is strictly prohibited.
ischemia of the stump
Ischemia is defined as a localized reduction in blood supply. These problems are caused by a narrowing or complete blockage of the arterial lumen. This situation is caused by the amputation of a limb in an area with poor circulation. This indicates an abnormal level during surgery. The wound does not heal and gangrene develops. All this is accompanied by very severe pain in the stump. The only cure in such a case is another amputation.
The sensation of a phantom stump in the operated patient is a harmless and even desirable phenomenon. It is called telescoping. This sensory abnormality helps the brain interpret information about the location of tendons, joints, and muscles. The patient feels the missing limb, but it appears to have shrunk significantly. This anomaly can persist for up to six months after surgery. However, these sensations are not to be confused with phantom pains.
Such a problem is not associated with tissue injury and therefore cannot always be treated by conventional means. The very term 'phantom' suggests that pain is occurring in a limb that is not there. In most cases, this phenomenon occurs in the first days after the operation. In some cases, however, it can last for months or even years. Affected patients describe the phantom pain with the following words: burning, tingling and pulsating.
The occurrence of this process in humans is associated with the formation of neuroblastoma. These are dense, rounded growths located in areas of nerve tissue growth. The cause of phantom limb pain in the later stages of rehabilitation is related to poor residual limb care and wearing a prosthesis. If symptoms occur, a doctor should also be consulted. FBS is diagnosed by several specialists - a surgeon, a neurologist and a trauma surgeon. There is a scale that determines the intensity of the patient's pain.
causes
Traumatic amputations are most common at work. However, in recent decades, due to the widespread use of power tools in the home, there has been an increase in traumatic limb amputations in the home (mostly while working in the countryside), usually affecting one or more fingers and less commonly the hand. Limb amputation can be caused by railroad trauma (being run over by the wheels of a streetcar or train) or by dropping a large load and having the limb entangled by moving machinery.
The limb is completely or partially severed from the body. Scale or proximal limb tears can occur with heavy falling loads and railroad injuries. With partial tears, the limb in the area of the injury and below resembles a misshapen sack with crushed contents. The wound is usually very dirty. Extensive lacerations and scalp injuries are also characteristic of tears caused by moving machinery; in some cases the amputated limb is divided into several fragments.
In guillotine amputations, the stump is flat. As a rule, traumatic amputations are accompanied by heavy bleeding. Exceptions are splint injuries and crushing of the limb with a heavy object (in these cases there is little or no bleeding due to the compression of the injured vessels). The general condition of the patient is moderate to severe. There is increasing restlessness, paleness of the skin, drop in blood pressure, accelerated breathing and heart rate. Unconsciousness may occur.
diagnosis
An initial diagnosis is not difficult to make. An X-ray of the residual limb is taken to assess the proximal limb and rule out fractures above the traumatic amputation. If there are other injuries, various examinations are ordered: X-rays of the affected body parts and limbs, laparoscopy, echoencephalography, etc. Laboratory tests are performed to determine the degree of blood loss and the general condition of the body. Preoperative preparation includes an EKG, chest X-ray, and other investigations.
At the first-aid stage, the action of the traumatic factor should be stopped as soon as possible (relief of the limbs, turning off the rotating mechanism, etc.). If necessary, resuscitation measures should be carried out: indirect cardiac massage and mouth-to-mouth resuscitation. In the event of bleeding, measures to stop the bleeding should be taken immediately. A pressure bandage is applied to the residual limb. If the bandage becomes saturated with blood quickly, it should be removed and another bandage applied. The limb is elevated above heart level and immobilized with splints or improvised materials (boards, cardboard, rolled-up magazines, etc.).
If the bleeding cannot be stopped with a tight bandage, a tourniquet is placed on the middle third of the thigh or arm. In highly traumatic amputations of the thigh or shoulder, bleeding cannot be stopped with a pressure bandage; in these cases, pressure is applied to the artery in the groin or armpit. Regardless of the condition of the amputated limb, the doctor must determine if it can be re-anastomosed. If the limb is partially severed, the distal limb is carefully placed on a splint and bandaged together with the proximal limb, taking care not to damage the preserved areas and not to disturb the contact between the proximal and distal parts.
In a total amputation, the severed portion is wrapped in dry, sterile gauze or a clean cloth and placed in two plastic bags (one inside the other). The bags are tied, placed in a plastic container, and the container is covered with cold water or ice packs. A piece of paper with the date and time of the injury is tied to the knot of the bag. Never treat the amputated fragment with alcohol or other disinfectants, do not soak it, do not place it in water or on ice - this can lead to tissue damage, weeping or cold injuries.
- Indications for amputation.
- blunt.
- What to do with amputated limbs?.
- The toe formation.
- Life after a leg amputation.
- acetabulum.
- prosthetic legs.
- Limb amputation.
