Our whole life consists of movement, and movement involves the work of about 400 skeletal muscles 1 , which also make up 40-45 % of our body weight 3 . It is therefore not surprising that each of us will experience muscle pain and discomfort in different parts of the body – neck, back, lower back and limbs 1 – more than once during our lifetime.
- Neuropathy (polyneuropathy) of the lower and upper limbs: symptoms, treatment
- What are the risks associated with neuropathy?
- Causes of myofascial pain syndromes
- Classification of muscle tension syndrome
- SYNDROME OF THE SMALL BUTTOCKS (GLUTEUS MEDIUS SYNDROME)
- Sternocleidomastoid Syndrome (Myofascial Compression Neuropathy of the Sciatic Nerve in the Pelvic Area)
- iliopsoas muscle. Anatomy. pain zones.
- What is the 'hair rule'?
- Diagnosis and treatment of iliopsoas syndrome.
- Causes of muscle pain
- muscle injuries
- Muscle tonic syndrome
- Infectious muscle diseases
- fibromyalgia .
- Treatment of muscle pain
- Main causes of pain
- Additional Symptoms
- Causes of muscle cramps after exercise
- types of myalgia
- consequences and complications
- preventive measures
- diagnosis of muscle pain
- Treatment options for myalgia
Neuropathy (polyneuropathy) of the lower and upper limbs: symptoms, treatment
Neuropathy is damage and dysfunction of the nerves. The disease causes pain and muscle weakness in the affected area. Polyneuropathy occurs when multiple nerves are affected.
- Burning, stabbing pain along affected nerve;
- swelling, numbness in the legs, goose bumps, tingling;
- muscle weakness in the legs, gradual muscle wasting;
- changes in gait, difficulty walking;
- decreased or increased sensitivity. The person does not feel touches on the leg, or on the contrary, they cause pain;
- Muscle cramps and diastoles, partial paralysis.
Symptoms of lower limb polyneuropathy are common in both legs.
What are the risks associated with neuropathy?
Polyneuropathy of the lower limbs can quickly progress to a chronic form. The patient rapidly develops muscle wasting and trophic ulcers and paralysis of the leg and respiratory muscles. There is a permanent change in the gait pattern that can no longer be changed.
I would like to say a big thank you to my doctor, Marina Kimovna Koreshkova, who is a professional in her field, very attentive and positive, as if she sees through you. I had a herniated disc in my neck and my shoulder was very weak. Marina Kimovna suggested me the right treatment. Already after the first treatment I felt much better. Nice clinic and caring staff. I would like to thank everyone who was involved in my treatment. I HIGHLY RECOMMEND THIS CLINIC.
Causes of myofascial pain syndromes
Triggers cause biochemical processes in the muscle to release inflammatory mediators that cause the muscle to reflexively contract.
The main symptom of myotonic syndrome is a deep, aching vertebrogenic pain. The painful contractions associated with thickening and swelling of one or more muscles severely limit mobility. The effect on the nerve receptors causes persistent muscle soreness. This in turn increases the muscle spasm and completes the vicious cycle of spasm - swelling - pain - spasm.
Musculotendinous syndrome in the lumbosacral area is usually the result of heavy physical exertion. Tensions in the musculus sulci can cause pain in the buttocks and hip joints. If the sciatic nerve is compressed, you may experience numbness in one of the limbs.
Cervical myofascial-tonic syndrome is characterized by cervical pain, neck pain that worsens with head extension and rotation, and IV and V finger hyperesthesia.
Thoracic myofascial syndrome is characterized by pain between the shoulder blades and along the ribs. Sometimes there can be a burning and tight feeling in the chest that mimics the symptoms of heart problems.
Classification of muscle tension syndrome
There are several types of pain syndromes related to muscle tone. They are classified according to their localization:
- Anterior lumbar muscular compression syndrome: It affects the III-VI cervical vertebrae area and the upper rib. Muscle contraction compresses the subclavian artery and brachial plexus.
- Psoas muscle syndrome: compression of the sciatic nerve and inferior gluteal artery
- Facet syndrome: local pain and stiffness in the region of the vertebral arch joints. It is associated with subluxation of vertebral segments and rupture of the joint capsules. Depending on the location of the affected facet joint, the pain can radiate to the head, shoulders, chest, lumbar spine, sacrum, hips or buttocks.
In addition, the trapezius, the largest pectoral muscle (pectoralis major), the quadratus lumborum and the shoulder extensor (scapulae) are often affected. The pain syndrome can be both primary (only the tissues affected by the spasm are affected) and secondary, that is, occurring outside the area of \u200b\u200bthe injury.
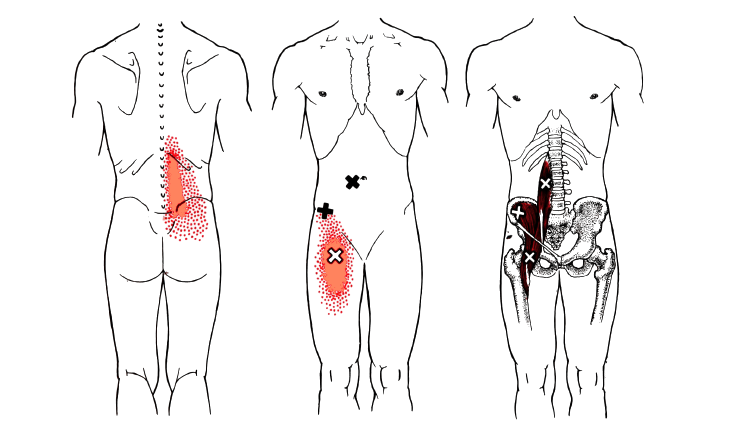
SYNDROME OF THE SMALL BUTTOCKS (GLUTEUS MEDIUS SYNDROME)
Clinically, it is manifested by pain during movements accompanied by muscle tension: getting up from a chair, crossing your legs, walking.
The pain can also spread to the entire buttocks, the back of the thigh, and the lower leg.
Tension of the medial sternocleidomastoid muscle in response to pain impulses is, according to several authors, very common, even more common than that of the sternocleidomastoid muscle.
The most common cause of overstretching of this muscle is overuse in the position, e.g. B. with a lateral curvature of the lumbar spine.
As with all muscle syndromes, the pain in gluteus medius syndrome occurs with movements that put stress on this muscle, such as bending. B. when changing body position, when walking and standing, especially when rotating the hips inwards and when placing the foot on the outside edge.
The affected buttock is comfortable to sit on, but when sitting on the healthy buttock and lying down, turning onto the healthy side, pain occurs on the affected side.
Similar to gluteus minor syndrome, the pain in the sacrum and gluteus maximus occurs when one leg is crossed over the other.
The pain in this syndrome spreads along the posterior and posterior lateral surface of the thigh.
Sternocleidomastoid Syndrome (Myofascial Compression Neuropathy of the Sciatic Nerve in the Pelvic Area)
The reflex response of the sternocleidomastoid muscle to a lesion of the lumbosacral spine is just one possible cause of this syndrome. The other causes are beyond the scope of this article.
The main complaint of sternum syndrome is dull, aching pain in the buttocks, sacroiliac and hip joints.
Pain decreases or disappears when lying down, or worsens with movements that stretch the muscle: standing, walking, adducting the leg, rotating the leg inward, squatting, standing up before standing up, throwing the leg backwards.
To avoid pain, sit with your knees apart and try not to put your foot on your leg.
As previously mentioned, pelvic myofascial pain can be caused by disorders of the internal organs, particularly the pelvic cavity (bladder, uterus, ovaries, intestines, etc.), disorders of the hip joints, and (most commonly) disorders of the lumbosacral spine.
Clinically, pelvic pain associated with spinal injuries can be divided into two syndromes:
- Local vertebral (spinal) syndrome – tension and pain in the paravertebral muscles, limitation of active movement in the lumbosacral spine, pain when touched in the projection of the lower lumbar vertebra or sacrum);
- Muscular pain syndrome includes the muscular syndromes described above.
If the above characteristics are taken into account, the diagnosis of pelvic pain can be made much easier.
If you do not live in Kaluga, you can register for an online consultation via WhatsApp: +7 (961)123-69-68.
For patients from other cities we offer affordable accommodation in apartments on spa and rehabilitation courses. For surgical procedures, we offer accommodation in a 24-hour inpatient facility.
iliopsoas muscle. Anatomy. pain zones.
There are two iliopsoas muscles - the left and the right. They are inside the body. Imagine the spine. The spine has a back that you can touch from behind and a front that faces our abdomen and specifically our internal organs. The iliopsoas muscles are now on the abdominal side of the spine. They start at the top, on the diaphragm and on the ribs, move inside the body along the entire lumbar spine and the sacrum, then exit through the pelvis on the groin to the thigh and start there in a small section on each side. Now let's put this in a slightly different perspective. In front of us is the human abdomen – the front wall of the abdomen. In the middle, below, are the intestines. Below that, deep inside, are the kidneys, and below the kidneys are the iliopsoas muscles, which lie at the front of the spine. Can you imagine that? So the iliopsoas muscles are attached with their larger side to the spine and pelvis and only a small part to the hip.
These details are very important. Once you understand how the iliopsoas muscles are organized and where they attach, it's easy to understand why they're more likely to cause lower back pain.
What is the 'hair rule'?
When you pull your hair, it's not the hair itself that hurts, but the point where the hair attaches to your head - at the root. We call this the hair principle. Similarly, when the iliopsoas muscle contracts, the pain is where the muscle is attached. As previously mentioned, most of the iliopsoas muscle is attached to the lumbosacral spine. Therefore, the pain occurs in 85 % of the patients in the area of the lumbar spine. The remaining 15 % have pain in the groin, thigh and lower abdomen where the other end of the muscle attaches.
Diagnosis and treatment of iliopsoas syndrome.
Chiropractors treat iliopsoas syndrome. However, in order to begin treatment, it is important to ensure that the pain is being caused by the muscle and not another problem. Therefore, a diagnosis is required. At this point we would like to point out the following. If it were so that as long as a person has a disease, others are not 'attached' to it, medical diagnosis would be simple and straightforward. But unfortunately it is much more complicated. Simultaneously with the iliopsoas syndrome, osteochondrosis, a herniated disc, arthrosis of the hip and a whole range of other diseases can occur. In such a situation, try to correctly identify the cause of the pain and make an accurate diagnosis. Here the muscle test is really indispensable as a diagnostic method. We can say with certainty that he is flawless in identifying sore and diseased muscles. Our doctors are very experienced in this method and are able to diagnose the iliopsoas muscle syndrome without any doubt. Once the diagnosis is established, treatment can begin.
- We find out whether your symptoms are caused by iliopsoas muscle syndrome, osteochondrosis, a herniated disc or a protrusion. We do a chiropractic muscle exam.
- The duration of the diagnosis is 30 minutes. It's a full investigation, not a 2-minute kneading tick.
- The diagnosis is made by Dr. Vlasenko AA, a doctor with 30 years of experience and an expert in the treatment of iliopsoas syndrome.
Treatment of iliopsoas syndrome consists of primary and secondary methods. The primary form of treatment for iliopsoas syndrome is gentle manual therapy; other forms of treatment are medication, physiotherapy, exercise therapy, etc. Manual therapy differs significantly from conventional manual therapy. Her name alone is the answer to the question 'What's the difference?'. she is gentle It is very similar to osteopathy and massage for hip and lumbar spine syndrome, but far superior.
Causes of muscle pain
The causes of muscle pain can be different. The most common are listed below.
muscle injuries
Muscle injuries are usually caused by physical exertion. They affect specific muscle groups and include:
- Sprains – occur as a result of a sudden sharp stretching or contraction of muscles and are characterized by muscle stiffness and pain that lasts for several days;
- Muscle overload or crepitus caused by intense training when transitioning to a new level of training, characterized by muscle soreness due to micro-injuries in the muscles.
Muscle tonic syndrome
Myofascial-tonic syndrome is prolonged muscle tension associated with painful thickening of the muscles. It is characterized by muscle spasms that occur reflexively, most often with spinal pathologies due to nerve root irritation. The syndrome occurs when:
The most common types of myofascial syndrome are the following muscles:
- front sternum;
- sternum;
- pectoralis minor;
- oblique head muscle;
- iliopsoas;
- calf muscle;
- Move.
Infectious muscle diseases
Myositis is muscle inflammation of parasitic, bacterial or viral origin, which can also occur as a complication of other diseases. Myositis can cause pain in any muscle in the body, in the upper and lower limbs and trunk. When moving, the pain is felt more clearly, and tight knots are felt in the muscles.
With purulent myositis, the pain is worse and is accompanied by:
fibromyalgia .
Fibromyalgia is symmetrical pain in muscles, ligaments and tendons that is chronic. They can be localized in a specific area:
Treatment of muscle pain
The CELT Pain Clinic uses modern methods of treating muscle pain to effectively combat the existing problem. It primarily aims to eliminate the cause. Systemic treatment minimizes (if not eliminates) pain. It includes the use of analgesics, nonsteroidal anti-inflammatory drugs, and opiates. Systemic therapy is combined with other treatment methods:
The CELT specialists recommend preventing muscle pain through a healthy and mobile lifestyle, ergonomics in the workplace and avoidance of unhealthy habits.
Main causes of pain
The main cause of external knee pain is iliopsoas syndrome.

This pathological condition is caused by increased pressure on the joint. It occurs primarily when the knee is bent frequently and with exertion.
Athletes are most commonly affected by this syndrome:
Pain on the outside of the knee can also be a symptom of many diseases and injuries, such as: B.
- tear of the meniscus;
- Hamstring bursitis - inflammation of the joint capsule of the hamstring tendon;
- gonarthrosis (arthrosis of the knee joint);
- Tendovaginitis (inflammation of the inner tendon sheath) of the semimembranosus muscle;
- Sprain, tear, or rupture of the external collateral ligament.
Causes of diseases and injuries associated with pain on the outside of the knee:
Acute pronation of the tibia when bearing the leg with a flexed or semi-flexed knee—playing football, hockey, skiing, or ice skating
More common in professional athletes due to the high daily load
For beginners due to poor technique


Gonarthrosis (degenerative disease of the knee joint)
Consequence of an injury – even 3 to 5 years later
Increased stress on the joint due to being overweight.
Age-related changes in the body – cartilage degradation accelerates with age
Metabolic disorders in which the cartilage is not sufficiently supplied with nutrients
Additional Symptoms
Various pathological conditions, in addition to pain, are accompanied by various additional symptoms.
At the time of injury, the pain is sharp and severe, and mobility of the joint is limited.
Over time, the intensity of the pain decreases, but it persists.
Slight pain on the outside of the knee, swelling
Gonarthrosis (arthrosis of the knee joint)
Affects not only the outer lateral joint, but the entire knee.
Stiffness and later restriction of movement are also annoying
Inflammation of the tendon of the semimembranosus muscle
Pain that increases when the knee bends
In the case of a sprain or tear: pain, swelling and restricted movement
In the case of a tear, in addition to the symptoms mentioned above, there is increased mobility of the knee.
Causes of muscle cramps after exercise
Sore muscles in the shoulder, lower back, neck or other parts of the body is a common occurrence during physical activity. Muscle soreness is common among novice athletes who overexert themselves just before the start. Experienced athletes who drastically change their training schedules are also prone to myalgia.
Muscle pain in these cases is caused by small tears in the muscle fibers. The microscopic wounds in the muscle fibers cause increasing pain. The body begins an intensive regeneration process: protein synthesis increases and hormones are released.
The symptoms subside after 2 to 3 weeks when the athlete gets into a rhythm and sets up a suitable training program. However, if the pain in the back and shoulder, or any other area, is stabbing and throbbing, the cause may be trauma and the athlete should see a trauma surgeon.
types of myalgia
- fibromyalgia. Occurs in ligaments and tendons and manifests itself in the back of the head, neck, and lower back. It often occurs in women due to stress and in men due to overwork at work or at the gym.
- Myositis is inflammation of muscle tissue. Occurs as a result of trauma, heavy physical exertion, or as a complication of the flu. Localized muscle pain in the legs, arms, or trunk that increases and becomes annoying with movement. The leg or arm is usually treated as an inpatient.
- polymyositis. A serious illness. It can cause severe pain in the neck and shoulders and then spread to the pelvic girdle and legs. Sometimes it leads to muscular dystrophy.
Most women suffer from sore muscles when expecting a baby. If a woman was not physically fit before pregnancy, the pain is more pronounced.
During pregnancy, the muscles can hurt in different places:
- back – due to the load from the enlarged body;
- abdomen – because of the painful stretching of the muscles;
- lower back – due to increased stress from growing body weight and natural displacement of internal organs;
- Legs - the causes of leg pain are the same - the pain is accompanied by leg cramps that appear at the beginning of sleep, at night or in the morning;
- Breasts – affected by changes in hormonal balance, increased blood circulation;
- Vaginismus – influenced by changes in venous hemodynamics, increased vascular load, decreased elasticity of muscle tissue.
consequences and complications
The consequences of injuries to the median nerve can be very serious: all three types (nerve inflammation, neuropathy, neuralgia) are common and severe, resulting in complete or partial disability in advanced cases.
With insufficient or no treatment, the patient is forced to change his profession and lifestyle.
Disabilities are not uncommon as a result of atrophy of the muscle tissue supplied by the damaged nerve. Unfortunately, many mistakes are often made in the diagnosis and treatment of this pathology.
preventive measures

In order to prevent pinching of the internal jugular nerve in time, trauma and hypothermia should be avoided.
It is worth remembering that risk groups include older people, athletes, people with obesity (metabolic problems), alcohol and drug addicts, and people with a sedentary lifestyle. You can also avoid the disease if you follow a few rules:
- Don't crouch for long (this is especially important for those who like to pick berries in the forest);
- When sitting, do not cross your legs over your head;
- Lead an active lifestyle;
- Rethink your diet (stick to healthy eating habits);
- Avoid infectious diseases (scarlet fever, HIV, tuberculosis, herpes, measles);
It is important that you seek professional help at the first sign of lesions. Most diseases can be treated conservatively at an early stage.
diagnosis of muscle pain
Determining the cause of muscle pain is not always easy. Only a doctor can understand the causes of myalgia and prescribe treatment that will help alleviate or eliminate the symptoms that plague you. To find out the cause of myalgia, your doctor will perform a comprehensive evaluation, including a neurological exam, laboratory tests, ultrasound, CT scan, and other tests 3 .

Myalgia is treated by various specialists. Depending on the cause, a traumatologist, rheumatologist, neurologist or endocrinologist can help.
Treatment options for myalgia
Treatment of myalgia includes both non-drug and pharmacological methods 5,13 . The doctor selects an individual therapy in each individual case.
One of the main goals is pain control 5,13 . When treating pain, doctors orientate themselves on the 'pain ladder' developed by the World Health Organization (WHO). She recommends the use of non-steroidal anti-inflammatory drugs (NSAIDs) such as MOTRIN® in the first phase of treatment for mild to moderate pain 6 . The drug is approved for use in adults and adolescents over 15 years of age 14 .
The active ingredient in MOTRIN®, naproxen, has an analgesic, anti-inflammatory and antipyretic effect. The drug can be used as part of a comprehensive treatment of mild to moderate myalgia syndrome associated with trauma, inflammation and musculoskeletal disorders 14 . A single dose of MOTRIN® lasts up to 12 hours 14 . The medicine can be used for up to 5 days 14 .
Consultation with a physician is necessary as symptomatic treatment and the use of painkillers are not a substitute for primary treatment of the condition 5 . If the acute pain persists, the doctor may use other methods of pain relief 13 .
Non-pharmacological treatments for myalgia include 13 :
- chiropractic treatment
- Massage;
- acupuncture
- transcutaneous electrical stimulation
- post-isometric relaxation;
- therapeutic exercises.
These therapies aim to relax tense muscles and relieve pain-causing spasms in order to break the 'vicious circle'.13 Myalgia can disrupt the rhythm of life and interfere with work.

Myalgia can disrupt the rhythm of life, work and recreation. In order to maintain your freedom of movement, you should be physically active and make sure that your muscles are not overloaded. Try to organize your workspace. If you work in a seated position, take regular breaks and move or stretch your muscles. Exercise keeps muscles toned, strengthens them and helps prevent muscle pain.
Read more:- Why does the galley muscle hurt?.
- Tibialis muscle pain.
- Which muscles hurt after running?.
- Your child's leg hurts and which doctor to see.
- Lamb Muscle Soreness.
- Ehlers-Danlo Syndrome.
- Marfan syndrome at a glance.
- Long fibula muscle.
