1. anterior to the bladder and then at the pubic symphysis (lig. pubovesicale, lig. vesicouterinum); the main ligaments (lig. cardinal) lie on the lateral pelvic walls;

- Internal genitalia (genitalia interna).
- uterus
- Anatomy of the inguinal ligament
- Origin and location of the inguinal ligament
- Position
- Structure of the inguinal canal
- epidemiology
- risk factors and groups
- Clinical criteria for diagnosis
- symptoms, course
- pathology
- surgery
- Peculiarities of the treatment
- Costs
- Causes of Bouchard Nodules
- Stages of Geberden nodules on the fingers
- Treatment of vocal cord nodules
- prognosis and prevention
- Material and methods.
- discussion
Internal genitalia (genitalia interna).
The internal genitalia include the vagina, uterus and its appendages, fallopian tubes, and ovaries (Fig. 2.2).
The vagina (vagina s. colpos) extends from the genital cleft to the uterus and passes through the urogenital and pelvic diaphragm areas with a posterior upward slope (Fig. 2.3). The vagina is about 10 cm long. It is mainly located in the pelvic cavity, where it ends in an anastomosis with the cervix. The front and back walls of the vagina are usually joined together at the bottom and are H-shaped in cross section. The top part is called the vaginal arch because the lumen forms pockets or arches around the vaginal part of the cervix. Because the vagina is at a 90° angle to the uterus, the posterior wall is much longer than the anterior and the posterior vault is deeper than the anterior and lateral vaults. The lateral wall of the vagina attaches to the cardiac ligament of the uterus and the diaphragm of the pelvis. The wall consists mainly of smooth muscle and dense connective tissue with numerous elastic fibers. The outer layer contains connective tissue with arteries, nerves and nerve plexuses. The mucosa has transverse and longitudinal folds. The front and rear longitudinal folds are called fold columns. The superficial squamous epithelium undergoes cyclic changes corresponding to the menstrual cycle.
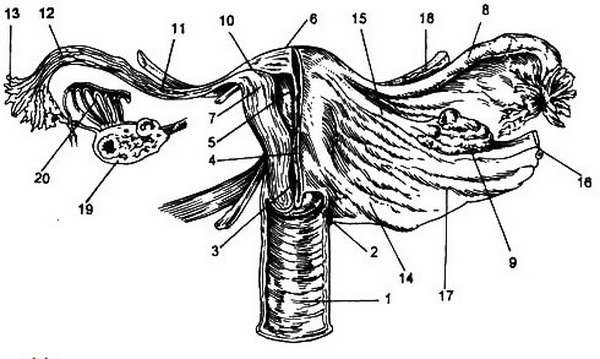
1 – sheath; 2 – vaginal part of the cervix; 3 – cervical canal; 4 - isthmus; 5 – uterine cavity; 6 - fundus; 7 – uterine wall; 8 – fallopian tube; 9 - ovary; 10 – interstitial part of fallopian tube; 11 – isthmic part of the fallopian tube; 12 – ampullary part of the fallopian tube; 13 – fimbriae of the fallopian tube; 14—ligamentum sacrouteri; 15 – ovarian ligament; 16 – ovarian ligament; 17 - broad ligament; 18 - circular ligament; 19—Transverse section of ovary with follicles and corpus luteum; 20— fallopian tubes.
uterus
The womb (uterus) is located at or near the midline of the pelvis outside of pregnancy, between the bladder at the front and the rectum at the back (see Figure 2.3). The uterus is inverted pear-shaped with thick muscular walls and a triangular lumen that is narrow in the sagittal plane and wide in the frontal plane. The uterus is divided into the shaft, fundus, cervix and isthmus. The vaginal line of attachment divides the cervix into vaginal and supravaginal segments. Outside of pregnancy, the arched floor of the uterus is forward and the body forms an obtuse angle with the vagina (leaning forward) and curves forward. The anterior surface of the body of the uterus is flat and abuts the apex of the bladder. The posterior surface is curved and faces the rectum from above and behind.
The cervix is directed downward and backward and is in contact with the posterior wall of the vagina. The ureters come relatively close to the cervix, directly to its side.
The body of the uterus, including the fundus, is covered by the peritoneum. Anteriorly, at the level of the isthmus, the peritoneum curves and extends to the top of the bladder, forming a shallow vesicoureteral recess. In the posterior part, the peritoneum extends forward and upward, enclosing the isthmus, the supravaginal part of the cervix, and the posterior fornix of the vagina before merging with the anterior surface of the rectum and forming a deep recto-urethral cavity. The corpus uteri has an average length of 5 cm. The total length of the body and cervix is about 2.5 cm and its diameter is 2 cm. The ratio between the length of the body and the length of the cervix depends on age and the number of births and is on average 2:1.
The uterine wall consists of a thin outer layer of the peritoneum - the serous membrane (perimetry) -, a thick intermediate layer of smooth muscle and connective tissue - the myometrium - and the inner lining (endometrium). The lining of the uterus contains many muscle fibers that decrease in number as you get closer to the cervix. The cervix is made up of equal parts muscle and connective tissue. The arrangement of muscle fibers in the uterine wall is complex, having evolved from contiguous portions of the endocervical (Mullerian) ducts. The outer layer of the myometrium contains mainly vertical fibers that run transversely in the upper part and connect to the outer longitudinal muscle layer of the fallopian tubes. The middle layer covers most of the uterine wall and is made up of a network of spiral muscle fibers that connect to the inner circular muscle layer of each fallopian tube. Bundles of smooth muscle fibers in the supporting ligaments intertwine and connect to this layer. The inner layer consists of circular fibers that can act as a sphincter in the isthmus and at the opening of the fallopian tubes.
Anatomy of the inguinal ligament
The inguinal ligament is a band that stretches between two elements of the pelvic bone, the pubic tubercle and the anterior superior iliac spine. This chord arch looks like a 11 to 13.5 cm long groove. This part of the body is paired. The umbilical ligament includes the ligament itself and the insertion of the iliotibialis, which runs deeper but in the same direction. A very narrow gap is formed between the two.

Under the tendon arch pass the iliopsoas muscle and the neurovascular bundle with the femoral nerve, iliac artery, and iliac vein. There is also the femoral fascia, a tunnel through which the femoral vessels and lymph nodes pass.
Density and tension are signs of a normal phallopelvic band. Occasionally there is stretching of this ligament. In men, the ligaments in the groin area are damaged by physical activity that puts tremendous pressure on the perineum. Inguinal ligament strains in women mostly occur during pregnancy. This leads to swelling, bruising and redness. Groin pain in both sexes can also be caused by inflammation of the lymph nodes in the groin. In this case, the area of \u200b\u200bthe inguinal ligaments is increased.
The inguinal ligaments found in the groin area of men and women have some differences. Statistically, the inguinal ligaments are more prone to injury in men while they are stronger in women because they are better reinforced by layers of muscle and tendon.
Origin and location of the inguinal ligament
The origin of the arch is the tendon edge of the external oblique muscle of the abdomen. The external oblique muscle is a muscle of the anterior abdominal wall that terminates in a white-silver tendon or aponeurosis composed of collagen and elastic fibers. They give stability to the entire abdomen. In men, the aponeurosis is less perfectly formed, which is why they are more prone to hernias in the perineal area.
The tendon arches branch out at the ends. The fibers involved in the formation of the tendon itself give rise to the lacunar ligament and the collapsed reflex ligament. The first formation is directed downwards, the second - upwards.
The scapular ligament or Cooper's ligament (pectineal ligament) extends from the base of the lacunar ligament. It extends along the pubic crest. It is very important in inguinal hernia surgeries: to tighten the tissue around the cleft, surgeons often puncture the pectineum ligament and retract the pectinale muscle.
Position
The arc starts at the sinewy part of the oblique muscle of the abdominis. The muscle ends in the aponeurosiswhich have the appearance of elastic fibers. They provide stability in the abdominal cavity. Aponeurosis is more pronounced in women. Therefore, hernia is diagnosed more often in men.

The ends of the tendon arch branch into smaller fibers. The fibers that play an important role in its formation are the origin of the lacunar ligament. The scapular ligament, which runs towards the pubic bone, starts from it. During groin surgery, it is not uncommon for the surgeon to puncture the scapular formation, preserving the scapular muscle.
Structure of the inguinal canal
The inguinal canal extends in one direction. It is a formation located in the peritoneal space at the exit of the internal organs.
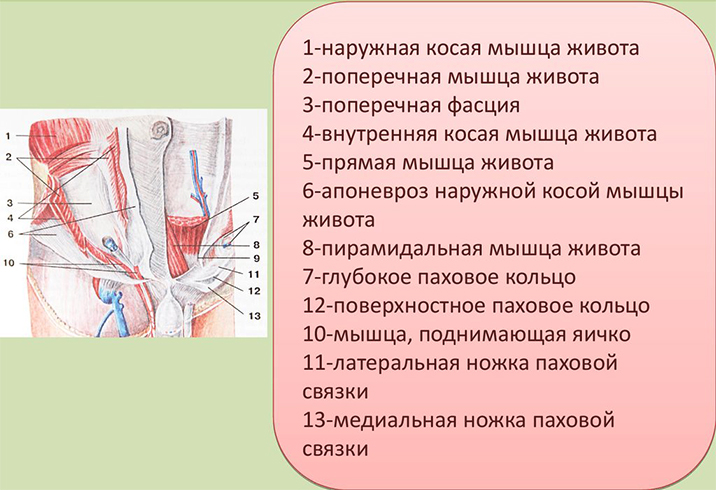
The length of the inguinal canal in men about 5 cm. In women, the fissure is slightly longer but much smaller in diameter. Only the beginning of the index finger fits into the ring at the beginning and end of the fissure. The size of the fissure depends on how stable the groin area is.
The anatomy of the fissure in men is more complex. It contains, among other things vas deferensand vas deferens, but also large blood vessels. In women, the space of the uterus. There is also the vaginal vestibule, which extends to the labia majora.
One risk factor is that the vaginal process does not enlarge, which can lead to the development of a hernia. This leads to congenital hernias in men and various types of cancer in women.
There are two types of hernias in the groin: Aslant i oblique and direct hernia. An oblique hernia is outside the canal. It enlarges the fissure and leads to a weakening of the aponeurosis. If it occurs for a long time, there may be a connection between the hernial sac and the spermatic cord. Such a hernia is often diagnosed as a congenital pathology.
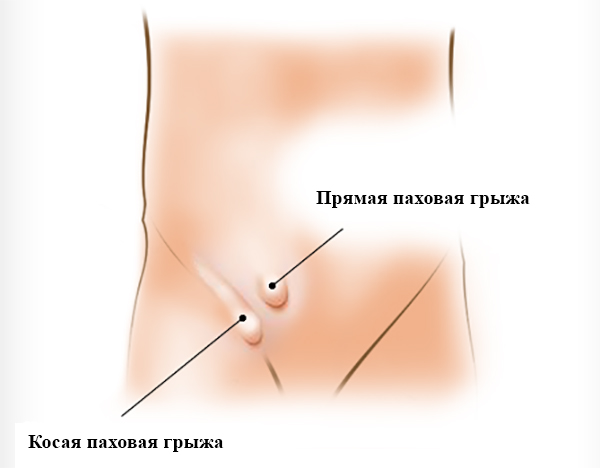
It goes straight through, bypassing the spermatic cord. It does not penetrate the genital organs. It is more commonly diagnosed in older people and is congenital.
With a hernia, the man suffers from pain in the groin. A bulge develops, which increases with physical activity.
epidemiology
Age: usually between 30 and 60 years.
Signs of prevalence: prevalence
Femoral hernias are diagnosed in about 5-8 % of all abdominal hernias.
They are more common in more mature and older women, but can also occur in young women who are pregnant again. Women aged 30-60 years account for 80 % of patients with femoral hernias. The higher incidence of femoral hernias in women is explained by a wider pelvis due to larger muscle and vascular gaps and lower gluteal ligament strength. Femoral hernias in women are more prone to impingement than inguinal and umbilical hernias.
The ratio of women to men has been estimated in various studies to be between 1.8:1 (USA) and 4:1 (Russian Federation).
risk factors and groups
- female gender;
– older age;
– pregnancy;
- Dysplasia syndrome Dysplasia is the abnormal development of tissues and organs.
Connective tissue;
– severe weight loss;
- Conditions associated with increased intra-abdominal pressure.
Clinical criteria for diagnosis
Groin pain, pelvic pain, thigh pain, pain on exertion, groin bulge, dysuria, positive cough syndrome
symptoms, course
diagnosis femoral hernia and hiatal hernia are not difficult to diagnose. Suspicion of such a hernia arises only from the pains in the groin, lower abdomen and thigh, which increase with walking, physical exertion and weather changes.
The pain is associated with a temporary, partial penetration of the hernia contents into the tight, rigid groin - numbness, stiffness.
The inner opening of the thigh canal. Persistent impingement is often the first clinical sign of such a hernia.
Clinical signs are. Complete femoral hernia:
1. A hernia bulge in the area of the ilium and inguinal groove. It is hemispherical, small and is located under the inguinal ligament on the inner side of the femoral vessels (in some cases the hernial bulge is above the inguinal ligament). The hernial orifice is visible in an upright posture and when straining. It disappears upon erection, sometimes with a rumbling sound.
A rumbling eardrum over the bulge is a symptom of a hernia that contains a gassy bowel.
(2) Positive cough symptom (also in the first form of hernia).
(3) In sliding bladder hernia, dysuria is the common term for urinary disturbances such as pain or difficulty urinating from the bladder.
phenomena.
pathology
Of the congenital anomalies and acquired malformations of the urinary bladder, hernia is the most common (see).
Inflammatory processes include furunculosis (see), carbuncle (see), hydradenitis (see), inflammation of the superficial lymph nodes (see lymphadenitis), which develops due to the transmission of infection from foci of inflammation, which develops mainly on the skin the external genitalia and the antero-medial surface of the thigh, sometimes also on the tibia and foot. Specific inguinal lymphadenitis is characteristic of primary syphilis (see) and soft tissue carcinoma (see). Soft tissue carcinoma often leads to purulent lymphadenopathy with the formation of a typical inguinal ulcer. Cold septic pustules caused by tuberculous arthritis sometimes descend into the groin (see).
surgery
The groin area is of great surgical interest in order to choose the safest surgical approach to the iliac blood vessels, abscesses and phlegmon located in the subperitoneal area of the small pelvis (see Pirogov's incision). In addition, surgical access to the contents of the inguinal canal (see) for inguinal hernias (see) and funiculocele (see vas deferens) is created via the PO incision.
Bibliography: Wenglowski RI About the descent of the testicles, in: Book: Works of the Surgical Clinic of the Hospital, ed. by PI Dyakonov, vol. 1, p. 7, M., 1903; the same, Development and 'structure of the groin, its relation to the etiology of hernias, M, 1903; 3olotareva TV. Surgical anatomy of the anterior-lateral wall of the abdomen, in book: Chir.23, L., 1972; Kukudzhanov NI inguinal hernias, M., 1969; Lubotsky DN Fundamentals of topographical anatomy, p. 458, M., 1953; Ostroverkhov GE Lubotsky DN and Bomash YM Operative surgery and topographical anatomy, M., 1972.
Peculiarities of the treatment
Conservative methods of eliminating discomfort that exclude surgical intervention are generally used in non-critical cases, when the torn tissue is only slightly damaged. The goal of this type of treatment, which includes anti-inflammatory drugs and physical therapy, is to reduce pain and normalize range of motion.
The physiotherapy exercises recommended as part of conservative treatment are not only intended to strengthen shoulder muscles and restore motor function, but also to prepare for surgery, which is considered the preferred option for rotator cuff injuries.

In modern medicine, minimally invasive (atraumatic) arthroscopic surgery is the most commonly used technique. This type of operation is performed using a special video camera with minimal magnification and special instruments that are inserted into the injured area through holes in the skin. In this way, arthroscopy prevents damage to the surrounding tissue and ensures a speedy recovery.

In addition to the treatment of rotator cuff injuries, arthroscopy can also be used successfully for other diseases of the shoulder joint, e.g. B. when correcting the shape of bones or removing osteophytes that lead to injuries of the cuff.

The rotator cuff, severed from the bone, is secured with titanium bio-inert anchors that are screwed into the bone. The anchor is sutured with sutures that tighten and fix the torn cuff fragment to the bone until the cuff is fully healed, which takes several months.
Costs
First visit to the surgeon's office
- Data collection through patient survey
- Clinical examination
- Symptoms of rotator cuff injuries
- Familiarization with diagnostic data from haematology, X-ray, MRI and/or ultrasound scans
- formulation of a diagnosis
- Development of a treatment plan
Follow-up examination by an orthopedic trauma surgeon
- Review of the diagnostic data of the first visit
- diagnosis of the disease
- Defining the best treatment option
Arthroscopic repair of the rotator cuff
- stay in the clinic
- anesthesia
- Rotator cuff reconstruction by arthroscopy
- consumables for surgical interventions
- Anchor implants from foreign manufacturers - Mitek, Smith and Nephew
Postoperative consultation with the attending physician
- Postoperative clinical examination
- Review of postoperative diagnostic results
- Presentation of recommendations for recovery
- puncture of the joint
- Injection of hyaluronic acid (possibly into the joint)
- Removal of sutures and bandages
Causes of Bouchard Nodules
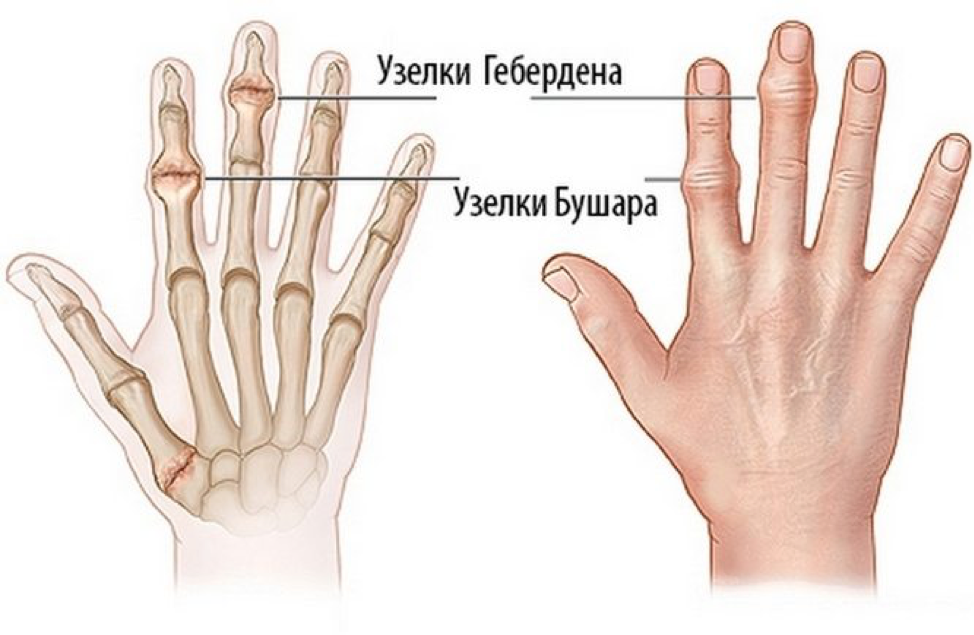
Geberden and Bouchard nodes are typical of osteoarthritis and especially of its special form, arthritis nodosa. They only occur in connection with the disease and never alone. It is believed that genetic factors play a role in the development of the lumps - the type of osteoarthritis in which they occur is inherited by women and is more common among them. The ratio of incidence in males and females is 1:10. Heberden nodules on the fingers are formed against the background of arthrosis. The formation of nodules is the body's response to the breakdown of articular cartilage. Under normal conditions, articular cartilage protects the bone heads by preventing them from rubbing against each other and cushioning impacts. As cartilage dries out, cracks, or wears away, its properties deteriorate, and bones begin to rub against each other instead of moving freely as before. To compensate for the injury and limit movement in the painful joint, the bone begins to form osteophytes. Bouchard nodules can also develop due to the following factors:
- Old. Hormonal changes during menopause and after menopause affect the quality of cartilage and bone tissue. Therefore, the first nodules are observed at the age of 45 and over. After the age of 80 they occur in one in three people. At a young age, Heberden nodules can form in professional baseball players, tennis players, and gymnasts.
- inheritance. Certain abnormalities in collagen synthesis, which are not fully understood at this time, affect the likelihood and rate of nodule formation. Bouchard nodules are also 3.5 times more likely to occur in people whose relatives have similar symptoms.
- injuries. Working with vibrating tools, home and sports injuries and cold injuries affect the cartilage and can promote osteoarthritis and thus the development of Bouchard's nodules.
- abnormalities of the handThey can be congenital (congenital) and affect the alignment of the joint surfaces and joint-specific movement. They can be congenital (e.g. joint hypermobility) or acquired (e.g. due to impaired fracture healing).
- DiseasesMetabolic diseases - e.g. B. Diabetes, gout, immune disorders - rheumatoid arthritis, or hormonal disorders - hypothyroidism, etc.
Stages of Geberden nodules on the fingers
The stage of Bouchard node formation is difficult to diagnose visually - only the size of the osteophytes is a clue. Itching and burning of the affected joints can also occur in the early stages.
The most accurate way to determine the stage of nodal hypertrophy is an X-ray:
- under stage 1 are small osteophytes visible on the x-ray;
- on page stage 2 the osteophytes begin to partially close the joint spaces, narrowing them, creating 'lines' of subchondral sclerosis;
- on page stage 3 large osteophytes and marked narrowing of the joint space are visible;
- large osteophytes almost completely occlude the joint spaces and deform the bone heads so that they become flat.
At no stage are changes found in the blood or urine.
Treatment of vocal cord nodules
Therapeutic tactics largely depend on the etiology, the severity of the disease and the demands of the patient himself or his work environment on the vocal properties. Patients who use their voice professionally often refuse surgery even when there is an immediate indication for surgical treatment. The following measures and methods can be used with 'singing knots':
- Pharmacological treatment. Pharmacological combinations are selected individually. Depending on the situation, antihistamines, NSAIDs and vitamin complexes can be used. Instillation of oils and corticosteroid suspensions is carried out.
- surgical treatment. It is performed in the case of pronounced nodular proliferation and the patient's inability to perform professional duties. The essence of the operation is the removal of abnormal growths under endoscopic control with local anesthesia or anesthesia.
- Physical therapy. Magnetic therapy, electrophoresis of the larynx with potassium iodide and potassium chloride improve the functioning of the voice. Hydro treatments in the form of pine baths, chamomile and sage infusion rinses, zinc and tannin inhalations are recommended.
prognosis and prevention
The prognosis of vocal cord nodules depends on their etiology, the effectiveness of the treatment performed, and the demands of the patient's voice. The criterion for the effectiveness of the treatment is the patient's subjective feeling, and not the presence of nodules on the surface of the vocal folds. It is often possible to alleviate the symptoms, but in the case of a chronic disease, a full restoration of voice quality is not always possible.
There is no specific prophylaxis. Non-specific preventive measures include giving up smoking, wearing respirators when working with hazardous volatile substances, normalizing vocal activity during the working day and adequate rest after it, modern treatment of acute and chronic ENT diseases and minimizing psycho -emotional stress.
1. Nodules of the vocal folds / SG Romanenko, OG Pavlikhin // Russian medical journal. – 2011 – №24.
2. Vocal cord nodules in adults and children / Alimetov HA. // Kazan Medical Journal. – 2003.
Material and methods.
Twenty boys with sliding hernias, including 19 children under 5 years of age with inguinal hernias and one 12-year-old child with bilateral thigh sliding hernias, were followed by us for 30 years. Most of them (14) were admitted with a diagnosis of impinged inguinal hernia. The preoperative diagnosis of a sliding hernia is difficult. An accurate diagnosis is usually only made during the operation. A right-sided sliding inguinal hernia was diagnosed in 16 children, including those with a leaky appendix (12) and a leaky bladder (4). A left-sided sliding hernia with discharge from the descending colon was present in 2 children. In one child, the sliding inguinal hernia was bilateral.
Caution should be exercised when operating on sliding hernias as excision or cutting away of the hernial sac may damage the sliding organ or perforate its wall. We observed two children under the age of 1 year who had a bladder injury with a sliding hernia during surgery. In both cases the bladder wound was repaired with suture and cystostomy and recovery was observed. When suturing the hernial ostium after removal of the hernial sac, the sliding organ behind the hernial ostium should be submerged retroperitoneally, followed by plication by one of the methods described above.
patient K.2.5 years old, was admitted to the Children's Surgery Clinic in Ryazan, complaining of pain in the right groin, enlargement and infiltration of the upper third of the right side of the scrotum. According to his mother, he had been ill and restless for 2 days. The patient was examined by a local surgeon and hospitalized with a diagnosis of hernia and acute lymphadenitis.
On admission he was in fair condition, with a body temperature of 37.8°C, a pulse of 120 per minute and satisfactory inflation. His tongue was swollen and dry and he had thrown up twice. His abdomen was soft, not painful, he did not have a bowel movement, he urinated freely. There was a 3.5 × 1.5 cm nodular mass in the right groin and upper third of the scrotum that was painful on palpation. The scrotal skin on the right side is engorged and infiltrated. The spermatic cord is undifferentiated. Palpation of the hernia is acutely painful. The testicle on the right side in the scrotum. Peripheral blood leukocytes 10-10 9 /l.
discussion
Diagnosing a hiatal hernia before surgery is extremely rare in both adults and children. According to Alessandri (1936), the presence of a urinary bladder in the hernial sac was determined preoperatively in only 5 out of 175 cases, in 71 patients the diagnosis was made during the operation, in 76 cases iatrogenic damage to the bladder was determined during the herniotomy and in 23 cases was the urinary bladder was not recognized even during the operation.
We have not found any description of femoral sliding hernia in childhood in the available literature [9-12].
The material from our study shows how difficult it is to diagnose sliding inguinal hernia before surgery. A correct diagnosis is usually only made during the operation. The second observation shows the possibility of bladder damage during surgery. The third observation shows how difficult it can sometimes be to diagnose a sliding femoral hernia. The child underwent two operations, but the correct diagnosis was never made. The entry of a sliding femoral hernia into the hernial sac could only be determined by a laparotomy and a revision of the anterior abdominal wall from the abdominal side.
So a sliding inguinal hernia in children is rare, a sliding femoral hernia is even rarer. In most cases, children with a sliding inguinal hernia are brought in as an emergency with a diagnosis of a compressed hernia. The colon and bladder as components of a sliding hernia remain viable, but the risk of their intraoperative damage is high.
The authors conclude that there is no conflict of interest.
Read more:- The Ligamentum Treitz, where it is located.
- Where do the body parts go after the operation?.
- Long legs, small body.
- Pronation and supination in anatomy.
- Stamping the shoe inwards, how to repair it.
- Osteophyte of the heel bone.
- shoulder supinators.
- tibial fasciitis.
