thigh triangle, scarpor, more correctly, this Scarpa's triangle [Scarpa], limited to the laterally laterally by M. sartorius, from medial – M. adductor longus, M. adductor longus; his vertex is formed by the intersection of these muscles, and the Base – inguinal ligament. The height of the thigh triangle is 15-20 cm.

- Anatomical Terminology
- directions
- Application in human anatomy
- What is the alveolar process?
- Structure of the alveolar ridge
- etiology
- classification
- formation of plant tissue
- hip channel
- Clinical anatomy of the deep vessels in the region of the femoral triangle
- Advantages and disadvantages
- Rehabilitation after implantation
- The B.UP technique consists of three simple steps
- Temporal range (lifting effect)
- Middle third (modeling)
- Middle Third (Volumization)
- The ideal patient
- General information
- signs
- symptoms
- causes
- Which doctor should be consulted?
Anatomical Terminology
Anatomical Terminology A number of terms are used in the anatomy of humans and other animals with bilateral body symmetry to precisely describe the position of body parts, organs and other anatomical structures in space and in relation to one another. And human anatomy has a number of terminological peculiarities, which will be described here and in a separate article.
Terms describing position in relation to the center of mass and the longitudinal axis of the body or appendage:
- abaxial (Antonym: adaxial) – located farther from the axis.
- adaxial (Antonym: abaxial) – adjacent to the axis.
- apical(Antonym: base)—adjacent to the apex.
- basal (Antonym: apical) – Located at the base.
- distal (Antonym: proximal)—located distally.
- Laterally (Antonym: medial) – Lateral, lying further from the medial plane.
- medial (Antonym: lateral) – medial, lying closer to the medial plane.
- proximal (Antonym: distal)—proximal.
Terms describing position in relation to major parts of the body:
- aboral (Antonym: adorable) – Located at the pole of the body opposite the oral cavity.
- adorable (Antonym: aboral) – located near the oral cavity.
- Abdominal – abdominal, refers to the abdominal region.
- Ventral (Antonym: dorsal)—ventral (anterior).
- Dorsal (Antonym: ventrally) is dorsal (backwards).
- caudal (Antonym: cranial)—caudal, located nearer the tail or posterior end of the body.
- cranial (Antonym: caudal)—Cephalic, situated nearer the head or at the anterior end of the body.
- rostral – Nasal – literally, located closer to the beak. Located closer to the head or at the front end of the body.
directions
In animals, the head is usually at one end of the body and the tail at the opposite end. The end of the head is called in anatomy skull, cranialis (Skull) denoted, and the caudal end is referred to as caudal, caudal (cauda – tail) referred to. The head itself is aligned with the animal's nose, and the direction towards its tip is called rostral, rostralis (rostrum – beak, nose).
The upward facing side of the animal's body, opposite to gravity, is called the dorsal, dorsal (dordum – back) and the opposite side of the body closest to the ground when the animal is in its natural posture, i.e. when running, flying or swimming ventrally, ventricular (stomach – abdomen). For example, the dorsal fin of a dolphin is located dorsaland the cow's udder is on the ventral Page.
The same terms apply to the limbs: proximal, proximalfor a point less far from the hull, and distal, distalisfor a more distant point. The same designations for internal organs refer to the distance from the origin of the organ in question (e.g.: 'distal segment of the jejunum').
Law, dexter, i Left, sinisterPages are labeled as they would appear from the point of view of the animal being examined. The term homolateral, less often ipsilateral refers to a spot on the same page while contralateral – is on the opposite side. Bilateral – refers to the situation on both sides.
Application in human anatomy
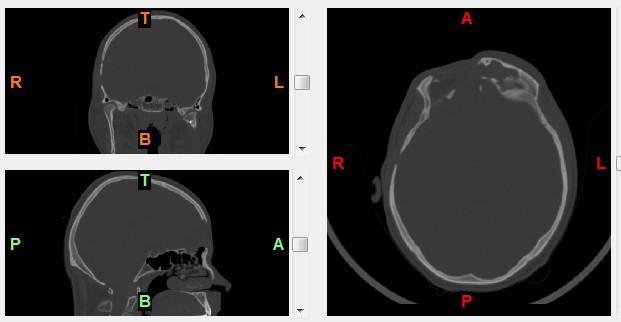

Orientation of the medical image (tomogram):
A - anterior, front, P – posterior, Rear
R - To the right, To the right,L- Left, Left
T - above, above, B – below, below
What is the alveolar process?
Bone tissue, which consists of the basal layer, fibrous tissue, and cortical lamina, plays an important role in the secure attachment of the dentition. It undergoes morphological and histological changes provoked by daily physical activity. Under The Alveolar Process (AO) is the anatomical part that holds together the elements of the upper and lower jaw. It occurs when teeth erupt and disappear after tooth loss.
The alveolar process consists of an inner and outer cortical lamina and cancellous bone tissue. It is traversed by small tubes through which blood vessels and nerves run. The anatomical structure of the jaw ridge is unpaired symmetrical, and cavities can vary in shape and size depending on the position of the tooth units. In the middle of the alveolar ridge are the alveoli, which are usually cone-shaped. A pathology or tooth loss leads to a significant reduction in bone volume, necessitating reconstruction of the alveolar ridge for subsequent implants.
Structure of the alveolar ridge
Based on the anatomical structure, the following parts are distinguished
- Laterally. Outer wall, which is in close proximity to the cheeks and lips.
- medial. The inner wall facing the tongue and hard palate has a compact structure.
- Middle. This area, where the lips are located, has a large number of blood channels. This is where the molars and incisors attach.
The alveoli, i.e. the tooth cavities, are separated from each other by special bony septa. There are also interroot septa in the alveolar region. If the dorsal area is not functionally loaded, the alveolar process deforms and the anatomical structure changes and becomes smaller. The development of pathological processes in the upper and lower jaws often leads to a fracture of the alveolar process, which may require correction of this anatomical region.
etiology
Lateral cartilage lesions of the knee can result from several common predisposing factors:
- A trauma affecting the knee and its components leading to the realization of one of the pathogenetic mechanisms of injury. These often occur in young people with high levels of physical activity and in athletes, both amateur and professional.
- Decreased tissue and cartilage strength, which develops mainly in older people as a result of degenerative processes in the structures of the musculoskeletal system, which are exacerbated by a deterioration in their diet.
- Congenital cartilage disorders that develop from childhood and are caused by changes in the functional activity of certain genes. In this case, the pathology in children can develop against the background of small loads on the musculoskeletal system.
- Chronic inflammation that leads to progressive weakening of the cartilage in the knee. Their development is mainly triggered by an infectious process or by the formation of antibodies by the immune system against one's own tissue (autoimmune process).
The cause must be determined by the doctor as part of the diagnosis. This makes it possible to prescribe preventive recommendations to avoid future pathological conditions.
classification
In order to allow a reliable, quick and qualitative assessment of the nature and extent of the lesions, all lesions are divided into different types. These are differentiated according to the severity of the injury:
- Incomplete tear - the injury is localized and does not extend beyond the knee, so the structure and shape of this joint is not changed.
- Total rupture – the injury is full thickness and extends beyond the cartilaginous element, resulting in a fracture and possible dislocation.
Depending on the location, lesions are distinguished that affect the body or the horn, or a combination of both. Pathological and traumatic lesions are distinguished according to the most important etiopathogenetic factor.
formation of plant tissue
Since then, the processes of cell reproduction and differentiation have progressed so far that a true miracle has emerged - you, the human being. Plants begin life the same way, with a small cell that develops into many different forms of tissues and organs. The learning tissue bears the main responsibility for the growth of the plant.
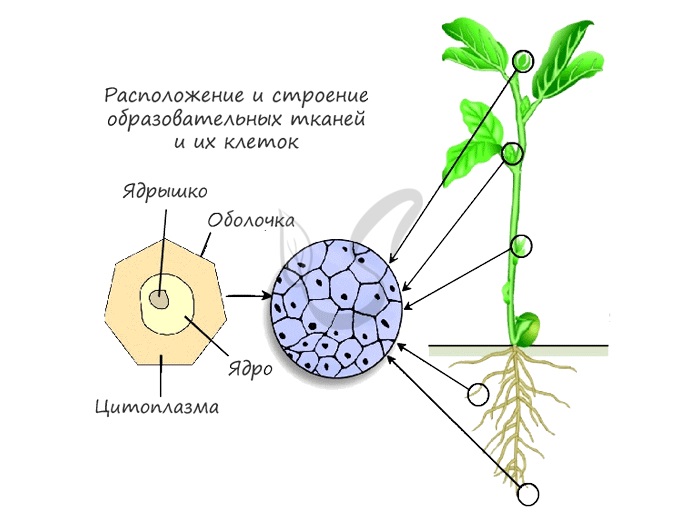
As you can see, the diagram shows schematically the location of the formation tissue. The most important of these are:
- Shoot tip - growth cone of the bud
- Root apex - dividing zone covered by a root sheath for protection
- Cambium - makes the plant grow in width
- The bases of the internodes and petioles are also active growth zones.
Cell division and growth take place in these areas. It is important to remember that seasonal changes in cambium cell activity are responsible for growth ring formation. The appearance of annual rings is due to chronology: more conductive tissue (thinner and looser in the middle) is formed in spring, and mechanical tissue (thicker, harder) in autumn. For this reason, the annual rings on the tree trunk look like interchangeable rings, which are different from each other.
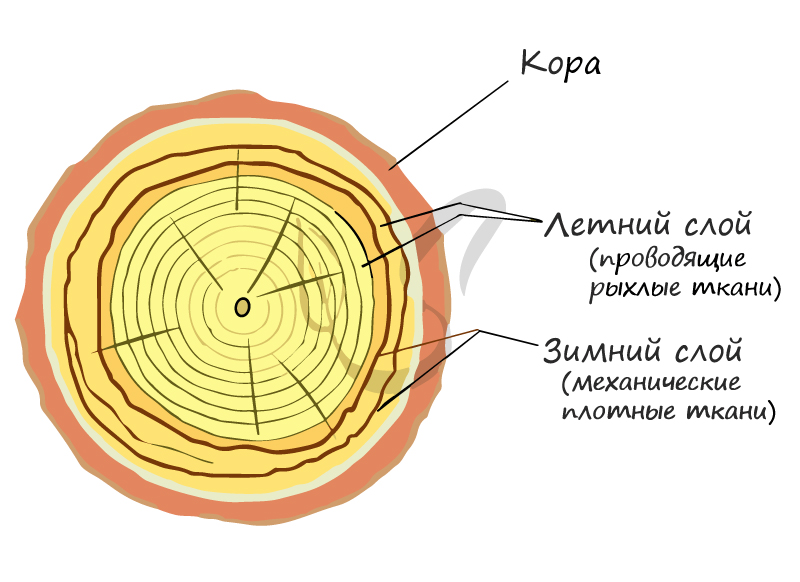
The appearance of the annual rings is strongly influenced by the environmental conditions. For example, when plants growing in swamps are nutrient poor, annual rings appear thinner than usual.
The wind also has an important influence: under its constant influence, the wood is redistributed along the trunk. By acting on the crown, the wind shifts the center of gravity of the tree, which affects the lower parts of the tree. They begin to thicken in a compensatory manner to keep the tree from breaking. With persistent wind, the trunk is severely deformed and the crown shape becomes ailing.
hip channel
All iLive content is reviewed by medical experts to ensure it is as accurate and fact-based as possible.
We have a strict policy in selecting sources of information, citing only reputable websites, academic research institutes and, where possible, peer-reviewed medical studies. Please note that the numbers in brackets ([1], [2] etc.) are interactive links to such studies.
If you think any of our material is inaccurate, out of date or otherwise questionable, please highlight it and press Ctrl + Enter.
The femoral canal (canalis femoralis) is 1-3 cm long and has three walls. The lateral wall of the canal is formed by the femoral vein, the anterior wall by the crescent edge and superior horn of the broad (femoral) fascia. The medial-posterior wall of the canal is formed by a deep flap of broad fascia covering the pectoralis muscle in this area. The subcutaneous ring (anulus saphenus) of the femoral canal is bordered on the lateral side by a crescent-shaped rim and closed by a thin rib fascia (fascia cribrosa). The deep ring of the femur, which usually contains some loose tissue and the Pirogow-Rosenmuller lymph node, has four walls. The anterior wall of the deep ring is the inguinal ligament, the lateral wall is the femoral vein, the medial wall is the lacunar ligament, and the posterior wall is the peclinal ligament, a fibrous periosteum at the pubic crest. The peclinal ligament is formed by connective tissue fibers that run from the medial end of the inguinal ligament posteriorly and laterally along the edge of the superior pubic ramus. These fibers round off the acute angle between the medial end of the inguinal ligament and the pubic bone.
On the front of the thigh are important topographical formations. This is primarily the femoral triangle, which is bounded by the adductor longus muscle of the thigh (medial), the cauda equina muscle (lateral), and the inguinal ligament (above). Through this triangle, under the skin and under the superficial flap of the broad thigh fascia, runs the Furrow of the iliac crest (Sulcus iliopsoas) (Sulcus iliopectineus), which is bounded on the lateral side by the M. iliopsoas and on the medial side by the M. pectoralis. Adjacent to this sulcus are the femoral artery and the femoral vein. This furrow merges into the femoro-popliteal canal, or adductor canal (canalis adductorius), through which pass the femoral artery, the great saphenous vein, and the saphenous nerve. The walls of the adductor canal are the medial vastus femoris (lateral) and adductor major (medial). The anterior wall of the disc canal is a fibrous lamina stretched between these muscles (lamina vastoadductoria, BNA). This lamina contains an opening, the tendon hiatus, through which the saphenous nerve and descending patellar artery exit onto the anteromedial wall of the canal. The femoral artery and vein pass through the inferior opening of the canal, formed by the tendon of the adductor major muscle and the posterior surface of the thigh, and drain into the saphenous fossa from above. The muscles of the thigh are covered by the broad fascia.
Clinical anatomy of the deep vessels in the region of the femoral triangle
Kalinin RE, Sukhkov IA, Klimentova EA, Shanaev IN
IP Pavlov Ryazan State Medical University, Ryazan, Russia
Purpose. Clarification of the anatomy of the deep femoral artery and deep femoral vein in the thigh triangle.
material and methods. The study was based on anatomical vascular section data in the upper third of the thigh (20 specimens) and duplex ultrasound angioscopy in patients undergoing routine vascular examinations (40 patients, 50 lower extremity patients). The ultrasound examination was performed with linear and convex transducers (frequency 3-13 and 3-5 MHz).
Results. The deep femoral artery originated from the common femoral artery in the majority of cases: 100 % of cases based on anatomic dissection and 98 % based on duplex ultrasound angioscopy. Two trunks of the deep femoral artery were identified in 14 % of the cases. Duplex ultrasound angioscopy showed a high branch of the deep femoral artery in 8 % and an anatomical dissection in 10 %. In most cases, the deep femoral artery arises from the posterior surface of the common femoral artery: in 46 % according to duplex ultrasound angioscopy, in 60 % at autopsy; on the posterolateral surface: in 36 % according to duplex ultrasound angioscopy and in 40 % at autopsy. Deviation of the deep femoral artery from the medial surface of the common femoral artery occurred in 8 % of the cases and was associated with an atypical saphenofemoral junction in 6 %. One patient was found to have one of the trunks of the deep femoral artery originating from the anterior surface of the common femoral artery.
Two deep femoral vein trunks were identified in 84 % of the cases. The proximal trunk drained into the femoral vein from the lateral surface just below the confluence of the deep femoral artery, and the distal trunk drained 1-1.5 cm down the posteromedial side of the femoral vein.
Advantages and disadvantages
In the past, lateral implants were very popular because it was possible to restore teeth on implants in unfavorable clinical conditions (bone loss) without having to resort to osteoplasty. Today, however, this technique is rarely used because there are better alternatives for the same indications (see below).
The disadvantages of the lateral technique are as follows
- very large trauma and bone tissue: therefore, rehabilitation takes longer than usual, in addition, patients experience more stress (people are simply afraid of such extensive procedures and the nature of the implants themselves),
- the operation is lengthy,
- there is very large bone loss, bone crushing or a bone block is often required,
- It is not possible to extract a tooth and place an implant at the same time: it is necessary to remove the affected teeth beforehand, and then wait 3-4 months for the extraction site to heal and for young bone to form at the extraction site,
- restriction of chewing activity during osseointegration,
- The chewing pressure is unevenly distributed: the main pressure is on the axis of the implant and not on the leaves,
- Rejection occurs more frequently (30-40 % of cases): in comparison, rejection reactions occur ten times less frequently with classic implantation (only 1-5 % of patients).
Rehabilitation after implantation
The main recommendations for patients after implantation are good oral hygiene and reducing chewing pressure on the implants. In the first days or weeks after the procedure, no solid food should be eaten, only soft food such as groats, mashed potatoes, soft-boiled vegetables or steamed schnitzel.
Due to the extent of the damage, the medications prescribed by the implantologist must be taken exactly as directed. Antibacterial agents, antihistamines, vitamin C, calcium and, if necessary, painkillers should be taken. Recovery is lengthy, requiring about 10-14 days off sick leave and then following strict rules for the next few months.
.jpg)
'In the beginning I was a bit negative about the primary technique because the dentists in my town advised against it. They said it was a very big injury, the bone had to be sawn through. But when I drove to the capital, the doubts went away. The doctor said that the side of the implants that are placed in the bone - this is a bygone era, now everything is much safer and more convenient. I recovered from the base very quickly, there was hardly any pain or swelling, and the teeth were ready by the third day.
The B.UP technique consists of three simple steps
Temporal range (lifting effect)
Step 1. Begins with the introduction of Belotero volume subcutaneously with a cannula (22G x 50 mm) in the middle of the zygomatic arch and 1 cm in front of the pericardium. The cannula is advanced vertically to the lower level, behind the hair growth line. Up to 0.5 ml of the bolus preparation is then injected subcutaneously into the temporal region on one side of the face.
Middle third (modeling)
Step 2. In the cheekbone area, treatment begins with a bolus injection of Belotero intensive supratemporal with a 27G needle. In the sternal fossa, the bolus of Belotero Intense is injected suprafacially with a 27-gauge needle. Up to 0.5 ml of Belotero Intense is injected on each side of the face to model the cheekbones. Belotero Intense is a flexible filler that does not compress, making it the best option for modeling the contours of the face.
Middle Third (Volumization)
Step 3. Up to 0.5 ml is injected into the subcutaneous fatty tissue in the cheekbone area. Belotero volume is injected laterally into the face with a 22G or 25G cannula (50 mm) in a fan or microbolus technique. Belotero Volume is injected with a 22G or 25G (50mm) cannula in a fan technique. Belotero volume powerful volume dispenserCreates a unique three-dimensional effect, 3D volume is achieved by magnifying the projection from different angles, creating a natural, rounded and harmonious shapes.


The ideal patient
- Age between 30 and 55 years.
- Ptosis grade I-II according to the Merz scale.
- No overweight.
- Need for a lift without excess volume.
Note that the density of the ligaments varies from region to region. Too much volume injected causes additional pressure on the septa. It is therefore recommended not to inject more than 1ml of the product on each side of the skin.. Disrupting the integrity of the septum (fan technique) results in reduced effectiveness. Choose the technique based on the patient's needs. Not every patient requires a volume filling in the middle third of the face or a filling in the sternal fossa.
General information
- The 4 incisors are the central teeth;
- The 2 canines are the 'eyes' or third teeth;
- The 4 molars (2 first and 2 second) are the chewing teeth, the fourth and fifth from the middle.
An adult has 28-32 permanent teeth, 20 milk teeth and 3-4 pairs of molars. The third molars, also called wisdom teeth, are the last to erupt. It is not uncommon for wisdom teeth not to have erupted or for there to be four of them. It is possible that the wisdom teeth are not formed in the uterus or that they are formed but do not grow out due to the individual jaw structure. Both conditions are considered normal.
Doctors recommend taking the child to the dentist when the first tooth comes out. And in the future to go to the dental examination every year, if there are no complaints. This time, however, let's not rush into anything. Be patient and wait for the first signs of teething.
signs
Tooth loss in children is a completely natural, physiological process. However, its symptoms can be uncomfortable for the child. However, in a healthy child, teething should not provoke any serious complications.
The symptoms of teething in infants are not specific. Sometimes they can hide behind infections and neurological problems. It is not for nothing that pediatricians and children's dentists refer to children's tooth syndrome as a diagnosis of exclusion. Only when the doctor is sure that all similar diseases have been ruled out can he attribute the symptoms to teething.
We roughly divide the teething diseases into 2 groups:
- Common Symptoms.
- Excessive salivation;
- swelling of the gums, their redness;
- moodiness, crying for no apparent reason;
- sleep disorders - the child has difficulty falling asleep, sleeps poorly, often wakes up and cries during sleep;
- bad appetite;
- Constant need to suck or chew - the child rubs against the pacifier or does not want to detach from the mother's breast;
- finger sucking
- Rare symptoms
- Fever;
- Frequent loose bowel movements;
- nasal congestion; rhinitis and runny nose with clear discharge;
- Vomit.
Don't be alarmed if these symptoms occasionally appear a few weeks before the first tooth erupts. That's nothing to worry about. It is simply a matter of the tooth starting to grow from the inside out, causing itching and increased salivary gland activity. Tooth eruption is asymptomatic in only 2 to 3 out of 10 babies. The appearance of a new tooth is accompanied by irritability, drooling and sleep disturbances in 70-90 % children.
Interestingly, symptoms are more pronounced in premature or low-weight babies (2-2.5 kg or less). These infants are also prone to diarrhea during teething. In immunocompromised infants, teething may be accompanied by a persistent fever and, in addition, throat or ear infections. Babies with neurological problems may even have seizures if teething is accompanied by severe pain.
symptoms
Pathologies of the spine manifest themselves gradually. At the initial stage, the sufferer feels only a slight discomfort in the lumbar region. Later, pain and impairment of many motor functions occur. This is due to the elasticity of the nerve roots and spinal ligaments in the lumbar region. If the canal lumen is slightly narrowed, they move with ease. When stenosis develops, its traumatization increases, which means irreversible changes. This is when a person has the following ailments
- pain radiating to the hip or leg;
- muscle weakness, tingling, numbness in the legs;
- bowel, bladder;
- motor problems;
- shooting spasms ;
- Limp.
Involuntary claudication can already be suspected in patients with lateral spinal stenosis. In the first stage, it is mild, episodic, accompanied by mild pain. At a later stage, it becomes more pronounced and is accompanied by severe pain. Finally, it can happen that the patient can only move with the help of others or is completely unable to move.
causes
A distinction is made between congenital and acquired lumbar spinal canal stenosis. The first type is caused by an abnormality in the skeletal system. For example, the vertebral arch can be short, the vertebral body deformed and the height of the intervertebral disc narrowed. Acquired stenosis is caused by:
- diseases of the musculoskeletal system,
- spinal injuries,
- natural aging of bone tissue;
- Excessive physical stress on the spine;
- excessive body weight;
- a reduction in the height of the intervertebral disc.
Unlike congenital pathology, acquired stenosis develops unnoticed for many years. The discomfort and mild pain that accompanies this degenerative process are perceived as symptoms of radiculitis or some other neurological condition. This process is accelerated by the presence of:
- herniated discs;
- arthrosis of the facet joints;
- thickening and hardening of the ligaments;
- osteophytes;
- dislocations of the vertebrae;
- tumors.
Late treatment leads to unsuccessful consequences. Advanced lateral canal stenosis is associated with severe decompression of the spinal canal and its contents. The patient gradually loses mobility, suffers from severe pain and is at risk of disability. The disease requires complex and intensive treatment over a long period of time and major surgical intervention.
Which doctor should be consulted?
If you have severe lower back pain that radiates down your leg or buttocks, you should not attribute it to physical exertion. Intermittent pain indicates degenerative changes are taking place in your spine. You need the help of a specialist doctor. You might want to visit one of these:
Read more:- Medial and lateral side.
- The lateral ankle is.
- The lateral dislocation is.
- Are human legs the same?.
- Triceps femoris muscle.
- A tricky stump.
- Bump on the side of the child's foot.
- disarticulation is.
