Behind a series of consecutive dislocations of the kneecap is undoubtedly chronic kneecap instability. However, this is no reason to stop your favorite sport and consciously limit your range of motion. Looking at the mechanics of the anterior aspect of the knee joint, it becomes clear that the kneecap tends to move outward (laterally) as the knee moves. The greater the tension in the quadriceps muscle, the more the kneecap is displaced outward (this is known as physiologic valgus) due to the shape of the joint between the femur and tibia. This shift is usually compensated for by the medial (internal) patellar retainer (or medial (internal) femoral-patellar ligament) as well as the specific shape of the thigh block. In primary patellar dislocation, the medial (internal) retainer of the patella is torn, and even if the diagnosis is absolutely correct and all recommendations are followed, the recurrence rate is as high as 60 %, both because of the poor healing ability of the medial retainer and because of the shape of the femoral blockage causing kneecap dislocation. This form of thigh blockage is very common in young girls with soft connective tissue and is referred to as outer thigh condyle hypoplasia.

- Instability of the knee joint
- causes
- Symptoms of luxating patella
- Types of patellar dislocations
- causes
- classification
- Treatment of lateral instability
- rehabilitation
- causes of injury
- How do you recognize a femoral condyle fracture?
- Diagnosis of pathology
- Surgical treatment of chronic kneecap instability
- Rehabilitation after surgical treatment of chronic patellar instability
- Dysplastic vertebral slippage (spondylolisthesis)
- 3 Degenerative gliding vertebra.
- Causes.
- Main types of kneecap dislocation
- diagnosis
- AdobeStock_85536119.jpg
Instability of the knee joint
The stability of the joint is a prerequisite for good function. It can move with a certain amplitude and in certain directions, and all loads are correctly distributed. Stability is provided by the joint capsule, ligamentous apparatus and the normal state of the articular cavity. Instability of the knee leads to a redistribution of loads. This not only damages the joint itself, but also the adjacent structures.
The main cause of knee instability is damage to the cruciate ligaments. Located in the joint cavity, these ligaments connect the articular surfaces of the tibia and femur. Damage to the cruciate ligaments often occurs as a result of trauma, meniscus damage and hemarthrosis (blood congestion in the joint cavity).
causes
Serious road accidents or competitive sports such as football, ice hockey, running or cross-country skiing often lead to the development of this pathology. The following activities can lead to the development of the disease:

People with a genetic predisposition (underdeveloped ligaments) are most susceptible.
Symptoms of luxating patella
The clinical symptoms of a patellar dislocation appear immediately after a traumatic mechanical impact. The first symptom is a sudden pain in the knee. The injured person notices a severe limitation of active mobility in the knee joint. The execution of passive movement actions is not possible to the full extent. Any passive movement or attempt to stand on the injured leg is accompanied by severe pain and a noticeable cracking sound.
When examining the patient, a displacement of the kneecap relative to the knee joint is detected. The area around the knee is swollen and congested. On palpation, a crunch (crepitation) can be felt in the area of the dislocation. Soft tissue injuries can lead to subcutaneous bleeding.
Types of patellar dislocations
The classification of dislocated kneecaps depends on whether they are congenital or acquired. Kneecap dislocations can also be classified according to their direction:
Depending on the severity of the injury, it can be a dislocation:
- mild and moderate dislocations not associated with ligament damage;
- Acute – first-time dislocations without full displacement and damage to surrounding tissues;
- Habitual – recurrent kneecap dislocations caused by pathological changes in the surrounding musculoskeletal system.
Determining the type of patellar dislocation largely determines the doctor's tactics and rehabilitation program.
causes
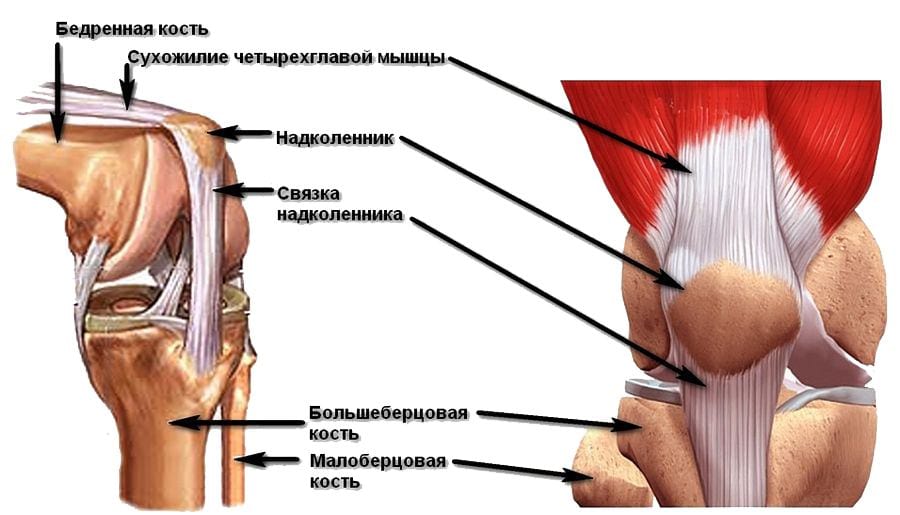
This dislocation usually results from direct trauma (falling on the knee joint, knocking the kneecap out of the way) in conjunction with a quadriceps contracture. Lateral dislocation of the kneecap usually occurs when the lower extremity is stretched. With the knee flexed, lateral dislocation is almost impossible because the kneecap is pressed firmly against the intercondylar surface of the thigh. In rare cases, vertical dislocation of the kneecap can occur when the tibia is flexed.
A flat patellar socket, an underdeveloped external thigh condyle, and an imbalance between the quadriceps axis and the ligaments of the kneecap increase the likelihood of a kneecap dislocation. These anatomical changes are usually subtle and go unnoticed until the injury occurs.
classification
In traumatology and orthopedics, a distinction is made between acquired (traumatic) and congenital dislocations of the kneecap. Depending on the age of the injury, a distinction is made between an acute kneecap dislocation and a permanent kneecap dislocation. A repeated dislocation is called a habitual dislocation. The distinction is made according to the direction of the dislocation:
- Lateral dislocations of the kneecap (external and internal);
- torsional (rotational) dislocations, in which the kneecap rotates about its vertical axis;
- Vertical dislocations in which the kneecap rotates about its horizontal axis and becomes trapped in the joint space between the tibia and femur.
The most common kneecap dislocation is external, while internal kneecap dislocation is less common. Torsion and vertical dislocations of the kneecap are extremely rare.
Treatment of lateral instability

The treatment of chronic kneecap instability is essentially surgical. In the vast majority of cases of habitual dislocation of the patella, arthroscopic revision (complete examination) of the knee joint and removal of free and immobile bodies of cartilage is required. These result from repeated traumatic pinching of the kneecap and thigh block, with the inner or medial cartilage of the kneecap being most commonly affected.
To ensure the proper function of the knee joint in chronic instability, the mechanical ability of the patella to withstand external displacement must be restored: the medial (internal) ligament of the femur and patella must be restored.
rehabilitation
In reconstruction of the medial (internal) ligament of the kneecap, an experienced surgeon stabilizes the kneecap with an autograft (a patient's tendon) to prevent repetitive dislocations. This elegant operation is now the gold standard for the treatment of chronic lateral patellar instability and allows the patient to return to their old sports program as quickly as possible. Long-term immobilization of the knee joint is generally not required after this type of surgery; rather, active rehabilitation should be started as soon as possible after surgery to restore range of motion and muscle strength as quickly as possible. The load on the lower limb is completely limited after this type of surgery. This type of surgery replaces the medial Yamamoto retention suture and lateral patellar release as it is more aesthetically pleasing and less likely to cause postoperative patellar instability.
causes of injury
In car accidents, your legs are more likely to hit the front seat or dashboard when you bend your knee. The direction of the force also plays a role in a hard impact – this injury is characterized by a direct impact on the lateral projection of the knee.
A low impact injury is caused by a slight bump or a simple fall. The main role is played by a disruption in the bone structure, which can occur with osteoporosis or as a result of age-related changes.
If there is an isolated fracture of the lateral condyle, it is likely that the tibia was forcibly externally tipped. If it moves medially, the fracture is in the medial structure.
How do you recognize a femoral condyle fracture?
- The main syndrome in this injury is pain. The focus of pain is the knee joint, which becomes flattened and loses its usual contours;
- Internal bleeding causes tissue bulging, swelling, and pain on palpation;
- When you press on the kneecap, you can feel its abnormal position and how it 'bounces' under the pressure of the blood that has pooled in the joint;
- When the condyle is dislocated, the tibia tilts to one side;
- The patient cannot perform active movements, and passive movements cause acute pain.
These symptoms occur with fractures of the kneecap and condyle, as well as with dislocations of the knee ligaments and meniscal injuries. For this reason, additional diagnostics are required for an accurate diagnosis. Femoral condyle fractures differ from fractures of the femoral condyle of the lower leg in that in the latter the pain is localized above the joint space of the knee, while it occurs below it.
Diagnosis of pathology
The diagnosis is made on the basis of the clinical data and additional research methods. Diagnosis begins with interviewing the patient and examining it. The doctor pays attention to the visual signs of fractures characteristic of a condyle fracture. When taking the anamnesis, attention must be paid to the type of injury, so that the patient must describe it precisely in a discussion with the doctor.
- The 'gold standard' is to have an X-ray taken. The X-ray image is made in two projections - straight and lateral. There are other examination methods, but they are used less frequently.
- If the X-ray results are not very conclusive or if there is any doubt, a CT scan is performed.
- MRI does not provide the necessary information about the condition of the bone - this method is used when there is a risk of soft tissue injury and it needs to be ruled out.
Surgical treatment of chronic kneecap instability
To treat the cause of this problem, the doctor may perform surgery on the kneecap.
The current state of the art makes it possible to operate on the knee joint with cumulative, gentle techniques.
One such technique is arthroscopy, a minimally invasive procedure performed under spinal anesthesia. Patients can usually walk again the day after the procedure.
It is performed with an arthroscope, a device in the form of a wire with a camera and light. During the procedure, two small incisions are made in the knee, through one the doctor inserts the arthroscope and through the other special mini-tools. The image from the arthroscope camera is transmitted to a high-resolution screen, allowing the surgeon to see all the smallest details and reliably monitor the operation. The operation usually lasts between 1-1.5 hours.
The fixation of the kneecap stabilization is also carried out via minimally invasive approaches, but without arthroscopic monitoring.
The preparation for the operation follows the usual medical standards.
Rehabilitation after surgical treatment of chronic patellar instability
After the operation you will have to stay in the hospital for three days. The doctor will fit the operated extremity with an orthosis for three weeks. During this time you will be on crutches. After two weeks, the crutches can be replaced with a walking stick. Then you can go independently.
After three weeks you can begin to bend the leg stretched in the splint to a 90 degree angle. You will continue these exercises for a fortnight.
Aggressive exercises to restore joint mobility and exercises to strengthen the thigh muscles can be started 1.5 months after surgery.
You can actively play sports again after 5-6 months.
Dysplastic vertebral slippage (spondylolisthesis)
Dysplastic spondylolisthesis (vertebral slippage)Dysplastic spondylolisthesis, also known as congenital lameness, is caused by underdevelopment of the facet or arch joints, usually the L5 or S1, causing the L5 to slip out of alignment with the sacrum. In addition, a misalignment of the sliding plane of the facet joint is determined. Women are twice as likely to be affected by this form of gliding vertebra as men.
Weakening of the articular processes, which can be caused by a fracture (more common in childhood or adolescence), causes the upper vertebra to slip out of alignment. It is the most commonly diagnosed slipped vertebra in young people, usually occurring at the L5-S1 level, and resulting in compression of nerve structures from enlarged connective tissue at the fracture site. Some authors suggest that the cause of the isthmic slipped vertebra is not a one-off injury but rather repeated trauma. Most patients with isthmic slipped vertebrae do not achieve a high degree of slipped vertebrae and do not complain of pain for a long time.
 Fig.3a,b,c. Isthmic spondylolisthesis (spondylolysis). (a) Radiograph of the lumbar spine. The arrow shows the defect area (spondylolysis) of the L5 vertebral arch. (b) Computed tomography (CT) of the L5 vertebra. The arrow indicates the defect area (spondylolysis) of the L5 vertebral arch. c) Magnetic resonance imaging (MRI) of the lumbar spine. The arrow indicates the posterior displacement of the 1st degree of the L5 vertebra. Fig.3a,b,c. Isthmic spondylolisthesis (spondylolysis). (a) Radiograph of the lumbar spine. The arrow shows the defect area (spondylolysis) of the L5 vertebral arch. (b) Computed tomography (CT) of the L5 vertebra. The arrow indicates the defect area (spondylolysis) of the L5 vertebral arch. c) Magnetic resonance imaging (MRI) of the lumbar spine. The arrow indicates the posterior displacement of the 1st degree of the L5 vertebra. |
3 Degenerative gliding vertebra.
The old classification called this form pseudospondylolisthesis because there was no weakness of the vertebral arches or the facet joints. This form of vertebral slippage was later referred to as degenerative because it is caused by degenerative changes in the spine ('aging of the spine'). The vast majority of people with degenerative slipped vertebrae appear after the age of 40. year of life. Women are four times more likely to suffer from a degenerative slip vertebra than men. The degenerative slip vertebra most commonly occurs at L4-L5, but can also occur at L3-L4 and L5-S1. Trunk defects in this form are rare, but the slipped vertebra can result in stenosis (narrowing) of the spinal canal with varying degrees of low back pain.
A slipped vertebra can also occur as a result of trauma. This damages the ligaments of the spine and sometimes fractures the vertebral bodies or spinous processes. The result is traumatic spondylolisthesis. Traumatic spondylolisthesis..
Causes.
People with an active lifestyle, who play sports and get a lot of physical activity are among the group most at risk of injury. The most common mechanisms are a fall on the knee, a lateral blow to the joint, and a sudden extension of the lower limbs.
Some of the most common causes of these types of injuries are.
- meniscus tear.
- Abnormal development of the kneecap.
- Weak ligaments and muscles in this area.
- Prolonged dislocation of the kneecap.
- dysplasia.
- Arthrosis of the articulating part of the knee.
- valgus deformity.
- Injuries Suffered.
- bleeding into the articular cavity.
Main types of kneecap dislocation

Traumatic and congenital dislocations are known in medicine, with a general distinction being made between acute and chronic (chronic) forms. Recurring injuries are referred to as the habitual type.
In addition, there are differences depending on the direction of the dislocation:
- Vertical – rotation occurs around the horizontal axis and is accompanied by penetration into the joint space.
- Rotation - when the 'pan' develops along its vertical axis.
- Lateral - occurs with a fall and a hard blow to the side of the knee, accompanied by lateral displacement of the kneecap (most common).
diagnosis
A patellar injury to the knee joint is always diagnosed with the help of instrumental methods of examination, which include:
- X-rays of the knee in straight and lateral projection are the most common diagnostic method performed in the trauma unit.
- Ultrasonography of the knee joint is a technique used to determine the volume of synovial fluid or blood in the joint cavity.
- Computed tomography and magnetic resonance imaging are high-resolution procedures that can be used to show even small anomalies in the anatomy of the knee.
- Arthroscopy is a diagnostic and treatment method in which an arthroscope (a tube with a camera and light) is inserted inside the knee joint to visualize the condition of the inner walls. Arthroscopy is usually used for combined injuries.
Once a kneecap injury is diagnosed, symptoms and treatment are individually determined by a trauma orthopedic specialist.
AdobeStock_85536119.jpg

AdobeStock_85536119.jpg
Treatment of the injury must be comprehensive. The type and extent of treatment depends on the type and severity of the injury:
- Patellar ligament injuries with incomplete rupture require conservative management. With a complete rupture, surgical treatment is performed.
- If the fracture does not move, the bone is immobilized with a plaster cast. If there is a slight displacement, the fracture is first reduced. A fragment fracture is treated surgically with osteosynthesis.
- The dislocation is reduced under anesthesia and then immobilized.
Arthroscopic surgical techniques are used for combined injuries.
Read more:- Dislocation of a bone in a joint.
- The lateral ankle is.
- dislocation of the foot.
- How do you tell if it's an ankle fracture or a dislocation?.
- dislocation of the ankle.
- Axis of rotation of the knee joint.
- The lateral side is.
- Rupture of the medial collateral ligament.
