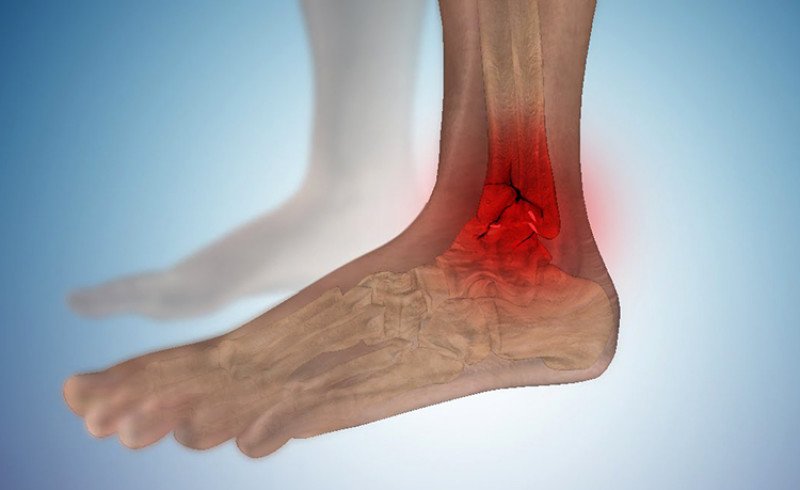
The knuckles are the bony extensions that form the ankle joint. The medial malleolus is the bony process of the lower part of the tibia, and the medial malleolus is the end of the fibula. An ankle fracture is almost the most common skeletal fracture, with the outer ankle being injured about five times more often than the inner ankle. This fracture is most common in the winter season as it is caused by falls on black ice.

- Fractures of the lower leg bones
- Clinic automation: fast and cheap!
- Clinic automation: fast and inexpensive!
- classification
- signs and symptoms
- Treatment
- Types of lateral malleolus injuries
- Lateral ankle sprain
- Type B (B1-3)
- Type C (C1-3)
- Symptoms of ankle fractures
- Treatment of ankle fractures
- period of rehabilitation
- complications
- symptoms
- to form
- causes
- diagnostic procedures
- Types
- symptoms
- What are the dangers of a deformed ankle joint?
- Treatment of ankle deformities in children and adults
Fractures of the lower leg bones
Tibia fracture – A pathological condition that occurs when the anatomical integrity of the tibial bone is disrupted [6].
Title of the minutes: 'Tibia fractures'.
Protocol code:
ICD-10 codes:
S82.1 Fracture of the proximal part of the tibia
S82.2 Fracture of the tibial shaft [diaphysis] of the tibia
S82.3 Fracture of the distal part of the tibia
S82.4 Fracture of fibula only
S82.5 Fracture of the medial malleolus
S82.6 Fracture of external [lateral] malleolus
S82.7 Multifracture fractures of the tibia
S82.8 Fractures of other parts of the lower leg
S82.9 Fracture of unspecified tibia.
Abbreviations used in the protocol:
HIV – Human immunodeficiency virus (HIV).
Ultrasound – Ultrasound examination
ECG – electrocardiogram.
Date of creation of the protocol: 2013
Patient category: Patients with tibia fractures
Users of the protocol: Traumatologists, orthopedists, surgeons in hospitals and polyclinics

Clinic automation: fast and cheap!
– 800 RUB / 5500 KZT / 27 BYN – 1 position per month

Clinic automation: fast and inexpensive!
classification
INTERNATIONAL CLASSIFICATION (Osteosynthesis associations) [1]
Depending on the location Tibia fractures are divided into three segments with one exception:
1. proximal segment
2. middle segment (diaphyseal)
3. distal segment
Exception for the distal part of the tibia:
4. Proximal segment of the ankle joint
1 Proximal segment fractures are divided into 3 types:
1А. Periarticular, in this type of fracture the articular surface of the bone is not damaged, although the fracture line runs within the capsule.
1В. Incomplete intra-articular fracture, in which only part of the articular surface is damaged and the rest remains connected to the diaphysis.
1С. Completely intraarticular, the articular surface is cleft and completely separated from the diaphysis.
2 The diaphyseal fractures are divided into 3 types according to the presence of contact between the fragments after reduction:
2А With only one fracture line, which can be spiral, oblique or transverse.
2В. with one or more fractures that still have some contact after reduction.
2С. Compound fracture with one or more fragments, fragmentary fracture in which there is no contact between the fragments after reduction.
3 Fractures of the distal segment are divided into 3 types depending on the degree of extension of the fracture to the articular surface:
3А. Periarticularly, the fracture line can be spiral, oblique or transverse, with breaks.
3В. incomplete intra-articular, only part of the articular surface is damaged, the rest remains connected to the diaphysis.
3С. Completely intraarticular, the articular surface is cleft and completely separated from the diaphysis.
4 Ankle fractures are divided into 3 types depending on the degree of damage to the lateral malleolus in relation to the level of the syndesmosis:
4А. Subsyndesmosis fractures (can occur in isolation, combined with a medial ankle fracture and with a fracture of the posterior edge of the tibia).
4В. Transverse syndesmosis (isolated, can be combined with a fracture of the internal ankle joint and with a fracture of the posterior edge of the tibia).
4С. Suprasyndesmosis (simple fracture of the lower third of the fibular diaphysis, fragmentary fracture of the lower third of the fibular diaphysis associated with damage to the medial structures, and fracture of the upper third of the fibula associated with damage to the medial structures).
signs and symptoms
The symptoms of a broken ankle can be similar to those of a sprained ankle (pain), but are usually more severe in comparison. An ankle sprain is extremely rare when only the ligaments are damaged. However, if the ankle joint breaks, the ankle bone can become unstable and dislocate or dislocate. Patients may experience ecchymosis ('black-blue' coloration due to bleeding under the skin), or there may be misalignment, alignment, gross instability, or lack of normal movement due to pain. In a displaced fracture, the skin sometimes extends beyond the sharp edge of the broken bone. Sharp fragments of the broken bone sometimes tear the skin and form a wound that communicates with the broken bone or joint space. This is called an 'open' fracture and if not treated in a timely manner, infection often occurs. Almost all displaced ankle fractures are now treated surgically to ensure proper alignment of the displaced fragments.
During the clinical examination, it is important to determine the exact location of the pain, the range of motion and the condition of the nerves and blood vessels. It is important to palpate the tibia (fibula) as there may be an associated proximal end fracture (Maisonneuve fracture), and to palpate the sole of the foot to look for a Jones fracture at the base of the fifth metatarsal (burst fracture).
Ankle injuries are assessed according to the Ottawa Ankle Rules, a set of rules designed to avoid unnecessary x-rays. The complete ankle series consists of three radiographs: anteroposterior, lateral and oblique (or 'mortise'). Incident view: an anteroposterior radiograph in which the ankle is rotated inward so that the lateral ankle is in the same horizontal plane as the medial ankle and the line drawn through both ankles is parallel to the tabletop, giving a position in which The tibia and fibula do not normally overlap. Typically, 10 to 20 degrees of internal rotation is required.
Treatment

Surgically treated bicondylar ankle fracture
Treatment for ankle fractures depends on the stability of the ankle joint. Some types of fractures are considered stable and can be treated like ankle sprains. All other fractures require surgical intervention, usually open reduction and internal fixation (ORIF), which uses a permanently implanted metal device to hold the bone in place during the natural healing process.
For children, recovery may be quicker with an ankle splint than with a full cast. for stable fractures.
Types of lateral malleolus injuries
Since the lateral ankle joint is subjected to constant stress, the most common injury is a fracture or sprain. In the first case there is a complete loss of human mobility and in the second case there is a partial loss of mobility. Loss of connection between the ankle and the foot occurs when the anterior and posterior ligaments of the talus maloneus or calcaneus maloneus are damaged.
There are the following types of ankle injuries:
- pronation In this case, an external force tries to rotate the fork outwards.In this case, an external force attempts to rotate the fork outward, resulting in a torn ligament and possibly a fracture. This type of injury is the most common, accounting for approximately 75 % of all injuries.
- Supination. What is characteristic is the opposite direction of external influence. However, the consequences are the same.
- broken bones. A common cause is impact, a sudden pressure surge to the area of the foot.
Treatment regimens were developed for each case described. Knowing where the ankle is can help determine the type of injury based on external symptoms, provide first aid and find yourself in a difficult situation.
If corrective action is not taken in a timely manner, there is a high probability of post-traumatic exacerbations. These include arthrosis of the ankle joint, which occurs due to inadequate treatment of the ankle joint.
Lateral ankle sprain
Most frequently The most common type of injury is a sprain rather than a tear of the ankle. It is caused by a sudden rotation of the foot without releasing the foot from its base or by a strong one mechanical mechanical impact. As a result, tears occur in the connective tissue structure and fluid - intercellular exudate and blood - accumulates.
Possible consequences include loss of mobility and flexibility of the ligaments.
- A fall from height, especially if the landing puts pressure on the heel area;
- a fall from a height, especially if the foot is compressed in the heel area while running or walking;
- spontaneous twisting of the foot when walking on uneven ground.
The first symptom of such an injury is a sharp pain in the ankle area. After 10-15 minutes, swelling appears and small hematomas may form. If the strain on the lower extremity persists, the symptoms worsen.
There may also be a slight grinding sensation when walking or changing foot position.
- There may be slight pain without anything changing on the outside. These will subside within a few days.
- Definite pain and swelling.
- The pain is constant and the swelling spreads over a large part of the lower leg.
If these symptoms occur, it is necessary to stop putting weight on the ankle and let it rest. Cold compresses or painkillers will relieve the pain and swelling.
Danger! If the pain worsens within 1-2 hours, an ambulance must be called. The cause can be not only a dislocation, but also a broken or broken bone.
Type B (B1-3)
Humerus: Oblique or torsion fracture that begins at the level of the ankle and runs proximally. The fracture line can be smooth or broken depending on the force applied.
Lateral malleolus: Intact or burst fracture at the attachment point of the ligament, rare tear of the deltoid ligament.
Posterior tibia: Intact or dorsolateral triangular fragment (Volkmann's triangle) with burst fracture of the posterior ligamentous syndesmosis.
Interosseous ligament system: The interosseous membrane is usually intact. The dorsal syndesmosis is more often intact or tears along with the posterior edge of the tibia (Volkmann's triangle).
The anterior syndesmosis (anterior tibiofibular ligament) remains intact below the ankle joint in the event of an oblique fracture of the lateral malleolus. However, if the fracture line begins at the level of the ankle joint gap, the anterior syndesmosis is ruptured or completely torn. Occasionally, a burst fracture can occur at the attachment of the ligament on the tibia (Tillo-Chaputa tuberosity) or on the fibula. The interosseous membrane usually remains intact.
The severity of the damage to the ligamentous apparatus and the severity of the ankle fracture progressively increases from type A to type B and type C.
In addition to ankle fractures and damage to the ligamentous apparatus, fractures of the medial and lateral edges of the talus bone should also be identified. Large osteochondral fragments may be present, as may fractures with cartilage separation.

Type C (C1-3)
Tibia: Diaphyseal fracture between syndesmosis and fibular head.
Medial ankle: Tearing fracture or rupture of the deltoid ligament.
Posterior edge of tibia: intact or torn at the site of the syndesmosis insertion.
Interosseous ligament apparatus: always torn. Tear in the proximal interosseous membrane of the ankle extending at least to the level of the fractured fibula.
The syndesmosis is torn or detached, along with bone fragments at the attachment site.
Symptoms of ankle fractures
The broken ankle is painful and swollen. The affected person is usually unable to shift their entire body weight onto the injured limb.
To diagnose a fracture, the doctor examines the ankle and gently palpates it. If a fracture is suspected, he will take several x-rays to confirm (or rule out) it.
Based on the results of the examination and the X-ray images, the doctor determines the stability of the ankle. He can determine the best treatment method.
Treatment of ankle fractures
For unstable fractures, surgery can sometimes be performed to compress the bone fragments.
With most stable ankle fractures (including burst fractures), doctors typically provide an ankle brace or cast that must be worn for about six weeks. An ankle brace has a Velcro closure, a rigid frame, and an outer cover to protect the foot from further damage. Stable ankle fractures usually heal well.
In case of Unstable ankle fractures surgery may be required. Typically, open repositioning with internal fixation surgery (ORVF) is performed. In ORVF, the broken bone fragments are reduced and then fixed with metal pins, screws, rods, plates and fixation brackets. After an unstable ankle fracture, the ankle may no longer be as resilient as before.
If the ankle is stable and the bone fragments are positioned correctly, the fracture will usually heal well. If the bone fragments do not stay in place, arthritis may develop and the ankle may break again.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
period of rehabilitation
From the time the bandage is removed for immobilization, immediate rehabilitation is recommended. The goal of rehabilitation therapy is to fully regenerate tissue, restore nerve communication between the limb and the brain, improve blood circulation, and build muscle lost during rest. How is rehabilitation carried out after an ankle fracture?
- During the first month, the doctor recommends light exercises that focus on the toes and knee. These exercises help restore joint mobility and gradually progress to more complex, compound exercises.
- In the second phase, more difficult exercises are performed: jumping, fast walking, swimming and running. It lasts 1.5-2 months and depends on the individual characteristics of the patient's body. Older people, for example, need significantly more time than children. Age is not the only limiting factor. It also depends on the complexity of the injury and chronic illnesses.
Important: Compliance with the doctor's recommendations is no less important. If these are followed, the positive prognosis is usually 100 %. Patients who do not adhere to the rest periods and special diet risk prolonged treatment and serious complications.
complications
The delicate mass is easily damaged and difficult to repair. In addition, an ankle injury is a complicating factor in therapy. It is worth noting that following the doctor's recommendations, daily treatments and diet can reduce undesirable effects to zero, but unfortunately no one is immune from this. What are the possible complications?
- The formation of a false joint. A false joint is the creation of mobility in an area of the bone where it shouldn't be. It is possible to eliminate this consequence through surgery.
- Development of arthritis, including purulent arthritis (if infected). This complication occurs more often after surgical treatment, but it can also occur with conservative treatment if rest and a balanced diet are not observed.
- Damage to a joint, e.g. B. Osteoarthritis. Partial, slight damage to the synovial membrane restricts the synthesis of synovial fluid. This leads to limited joint mobility, accompanied by painful sensations.
Damage to nerve structures can lead to loss of sensation and partial loss of innervation to the foot. Although these consequences are rare, they do occur.
There are many other complications, but they occur much less frequently than those mentioned above.
symptoms
The clinical presentation of ankle fractures varies and depends on the mechanism of injury, the number of fractures sustained, and whether the joint is subluxated or dislocated. Ankle fractures are accompanied by varying degrees of pain at the fracture site, pronounced swelling of the entire joint and the inability to put weight on the leg. However, in some cases - when there is only an ankle fracture without displacement and without dislocation of the joint - the patient is able to walk and overcome the pain.
Physical examination reveals deformity of the joint, swelling at the site of injury, and extensive bruising. When palpating the ankle joint, local tenderness is noted. When trying to move the bones that make up the joint, deformity, abnormal mobility of the joint and crepitus (crunching of bone fragments) are noted. When the affected foot is moved to the side of the fracture or to the other side, pain occurs. In the first case it is caused by the stress on the ankle bone caused by the broken ankle, in the second case by ligament tension and irritation of the fracture site. Movement of the ankle joint is restricted by severe pain. In subluxations and dislocations, the foot is displaced, often outward, resulting in a bayonet-like flexion of the limb. The skin on the side opposite the dislocation is tense and whitish in color (a sign of ischemia).
to form
Depending on the mechanism by which the ankle fracture occurs, a distinction is made between:
- Pronation and pronation abduction fractures – occur when the foot is externally rotated;
- Supination and supination-abduction fractures – occur when the foot is rotated inward;
- Rotational fractures – occur when the tibia rotates around an axis while the foot is in a fixed position.
The combination of fracture and dislocation is called fracture-dislocation. It is classified as a compound fracture.
causes
Direct injuries – injuries resulting from a direct impact on the ankle area (impact of the ankle or foot on an object, sprain of the ankle, self-injury). Non-direct injuries - are abnormal or excessive movements of the foot (plantar flexion of the foot - inward or outward rotation of the foot, dorsiflexion or plantar flexion).
diagnostic procedures
The diagnosis of an ankle fracture is made by the trauma surgeon based on the complaints, medical history, clinical examination and instrumental examination methods. Diagnosis is aimed at determining the type and location of the rupture, the severity of the disease and the complications present.
Based on the history, it is important to determine the mechanism of injury.
If a bone fracture in the foot is suspected, x-rays of the foot are taken in two projections - lateral and anterior. Computed tomography (CT) is used when X-ray examination does not provide sufficient information. Magnetic resonance imaging (MRI) allows for a more detailed view of soft tissue structures, which is essential for diagnosing nerve, vascular and ligament injuries.
General clinical urine and blood tests, as well as routine biochemical blood tests, have no independent value and are carried out to assess the general condition, as well as to diagnose the underlying disease and any complications that may arise.
Torn ligaments (complete or incomplete) of the ankle joint are used in the differential diagnosis of fractures.
Most important instrumental examinations:
Types
Fractures of the ankle joint can be closed or open.
They are classified according to their location:
- Closed fracture of the lateral ankle joint;
- Fracture of the medial malleolus of non-open type;
- Fracture of the lateral or medial part of the ankle joint with displacement;
- Fracture of both fragments without dislocation;
- both parts of the ankle are broken and the foot is dislocated or subluxated;
- open fracture.
According to the mechanism of injury, a distinction is made between:
- Injuries related to pronation (outward rotation of the foot). There is a stretch or tear of a group of collateral ligaments and there is a high possibility of a fracture of the fibula in the lower areas. A strain of the intercondylar joint is often observed.
- Supination wounds (foot tilted inward). There is a separation of the lateral part of the bone and a fracture of the medial part. The distal part of the tibia is fractured.
- Rotational lesions (the tibia rotates around its axis, the foot remains in a fixed position). Possible dislocation or subluxation of the foot in the anterior and posterior projection. Rotational fracture of the fibula and splinter injury of the tibia. The intercondylar joint is torn. The skull bone is broken or detached.
symptoms
The symptoms of the disease are as follows:
- A crunching sound is heard at the time of injury;
- Acute pain in the affected area that increases with strain, no grip on the limb, palpation is painful.
- Significant soft tissue swelling; the ankle joint is enlarged;
- Hemorrhages and multiple hematomas spreading near the site of injury;
- Invalidity of the joint, possible anomalies of movements, crunching noises;
- the correct position of the sole is disturbed.
What are the dangers of a deformed ankle joint?
Now let’s look at the dangers of ankle deformity. Most often, in childhood, it leads to complete curvature of the lower limbs and the development of clubfoot, which is very difficult to correct in the future using conservative methods. By the age of 5, the foot bones, their position, the connecting joints, ligaments and tendons are actively developing. Any deviation from the norm has negative consequences. The child begins to lag behind physically, unable to run and jump at the same pace as healthy peers. This leads to the accumulation of excess body weight, which can develop into full-blown obesity.
The metabolic disorders further increase the process of pathological changes in the cartilage tissue of the ankle joint. The length and elasticity of the tendons and ligaments are changed. The tendon and ligament apparatus becomes unstable in relation to the attachment of the bone heads that form the joint capsule. This leads to numerous recurring strains and sprains.
In adults, deformities of the ankle joint damage nerve fibers and disrupt the blood supply to the soft tissues of the foot. This leads to pain and reduced endurance during physical activity. There is a risk of developing heel spurs.
An equally dangerous complication is the destruction of all large joints of the lower limbs. These include deforming gonarthrosis, coxarthrosis and arthrosis of the hip and sacroiliac joint. This can accelerate the degeneration of the cartilage discs between the spine and the ankle joints, for example to absorb the increased shock load.
Only if you contact the doctor and orthopedist in a timely manner and begin to correct the existing problem, the development of these tragic complications and negative consequences can be avoided.
Treatment of ankle deformities in children and adults
Ankle deformities in children up to 5 years of age can only be partially corrected by using special orthopedic footwear. Because up to this age, the formation of the foot continues, and it is not safe to use any radical methods. In our chiropractic clinic we only accept children aged five and over for the treatment of problems with the musculoskeletal system.
Treatment of ankle deformities in children and adults always begins with an examination and identifying the possible causes of the problem. The doctor will then do everything possible to rule out further negative effects. For example, if the patient is overweight, a special diet is developed, moderate exercise is carried out and other techniques are used to normalize the weight. If weakness of the ligaments, tendons or muscles is detected, rehabilitation measures are carried out, etc.
The course of correction and treatment of ankle deformity is determined by the orthopedist individually for each patient. That's why it's worth making a free appointment at our chiropractic clinic right away.
We use a range of techniques that allow for complete healing of the ankle (except for stage 3 and 4 disease). For correction we use the following therapeutic techniques:
- Osteopathy – the specialist uses manual manipulations to improve all tissues and restore microcirculation of blood and lymph;
- Massage – increases the tension and flexibility of muscles, ligaments and tendons, controls the alignment of all bones in the joint capsule, improves blood circulation and fluid drainage;
- Physiotherapy – accelerates metabolism at the cellular level and shortens rehabilitation time;
- Reflex therapy – activates the regeneration of all damaged tissues by acting on biologically active points on the human body;
- Therapeutic exercises and kinesiotherapy strengthen the muscles and improve their functional state, correct foot alignment is possible;
- In complicated cases, laser treatment is performed.
- syndesmosis.
- The intercondylar syndesmosis is the.
- fibula.
- pelvic subluxation.
- tibia and fibula.
- The hock is the place where.
- The lateral dislocation is.
- Anatomy of the syndesmosis.
