The tibio-calfal syndesmosis is the connection between the distal tibial and fibular epiphyses. It is formed by three ligaments: the anterior and posterior inferior tibio-calfal ligament and the interosseous tibio-calfal ligament. A fourth ligament (the transverse inferior tibial ligament) is part of the posterior inferior tibial ligament, although some authors consider these ligaments separately. Although the syndesmosis is technically a joint, most literature describes syndesmosis injury as an injury to these ligaments. We have the same opinion.
- RU2187269C1 - Method for treating a distal intertibial syndesmosis tear - Google Patents
- Pictures
- anatomy
- Inferior tibiofibular ligament
- Anterior inferior tibial ligament
- diagnosis and treatment
- Sources:
- Types of pinched lower back nerve in men and women
- Diagnosis of dorsopathy
- Rupture of the distal intertibial syndesmosis
- Consequences of a torn syndesmosis of the ankle joint
- treatment methods
- Free medical advice and diagnosis
- Journal of Trauma Vol. 11, No. 4, 2010
- How do ankle injuries occur?
- Symptoms of torn ligaments
- ICD-10
- Causes of synostosis
- Congenital synostosis
- Post-traumatic synostosis
- Intercorporeal syndesmosis injury – treatment in St. Petersburg (SPb)
- Prices for treatment of intertibial syndesmosis injury in St. Petersburg (SPb)
RU2187269C1 - Method for treating a distal intertibial syndesmosis tear - Google Patents
Publication number RU2187269C1 RU2187269C1 RU2001100640A RU2001100640A RU2187269C1 RU 2187269 C1 RU2187269 C1 RU 2187269C1 RU 2001100640 A RU 2001100 640A RU 2001100640A RU 2001100640 A RU2001100640 A RU 2001100640A RU 2001100640A RU 2187269 C1 RU2187269 C1 RU 2187269C1 Authority RU Russia State of the art Keywords anterior tibia canal anterior ankle joint date of stand of technology 2001-. 01-09 Application number RU2001100640A Other languages English ( en ) Inventor Р. M. Сабиров В.В. Никитин Р.И. Еникев А.В. Конев Original Assignee Конев Андрей Владимирович Priority date (The priority date is an assumption and does not represent a legal conclusion. Google has not conducted a legal analysis and does not guarantee the accuracy of the specified date). 2001-01-09 Date of submission 2001-01-09 Date of publication 2002-08-20 2001-01-09 Application submitted by Конев Андрей Владимирович submitted Critical Конев Андрей В ладимирович 2001-. 01-09 Priority to RU2001100640A Priority Critical Patent/RU2187269C1/ru 2002-08-20 Application granted Critical 2002-08-20 Publication RU2187269C1 Publication Critical Patent/RU2187269C1/ru
- Espacenet
- Global documentation
- discussion
- 2100003423 Ankle joint anatomy 0,000 Claims Summary Description 38
- 2100002303 Anatomy of the tibia 0.000 caveats abstract description 18
- 210000000988 Anatomy of the bone and ankle 0.000 Details Description 34
- 230000015572 Biosynthesis process Effects 0.000 Claims Description 3
- 238000005755 Generation reaction methods 0.000 Description of claims 3
- 2100001149 Lower tibial joint anatomy 0.000 Description of damage 3
- 239000003814 Medicinal substances 0.000 abstract description 3
- 230000000399 Orthopedic effects 0.000 abstract description 3
- 230000000694 Effects Effects 0.000 abstract description 2
- 230000000903 Blocking effects 0.000 abstract description 1
- 2390000126 Substance Effects 0.000 abstract description 1
- 238000002560 therapeutic procedure methods 0.000 summary 1
- 2100001737 Ankle joint anatomy 0.000 Description 11
- 2100002683 Anatomy of the foot 0.000 Description 7
- 2100003906 Anatomy of the tibial head 0.000 Description 6
- 2100003041 Anatomy of Ligaments 0.000 Description 5
- 206010022114 Trauma-related illnesses 0.000 Description 4
- 206010023204 Joint dislocations Diseases 0.000 Description 4
- 2100002082 Anatomy of the fibula 0.000 Description 3
- 229920004936 Lavsan® Polymers 0.000 Description 3
- 239000005020 Polyethylene terephthalate substances 0.000 Description 3
- 2100002414 Anatomy of the legs 0.000 Description 2
- 2100004417 Anatomy of the kneecap 0.000 Description 2
- 208000002847 Wound surgery 0.000 Description 2
- 2100004233 Calcaneus Anatomy 0.000 Description 2
- 2100002435 Anatomy of tendons 0.000 Description 2
- 238000006073 Methods of the contortion reaction 0.000 Description 2
- 239000011505 Gypsum substances 0.000 Description 2
- 210000000456 Anatomy of the ankle bone 0.000 Description 2
- 210000002808 Anatomy of connective tissue 0.000 Description 1
- 206010011376 Diseases of the spine 0.000 Description 1
- 2100003414 Limb Anatomy 0.000 Description 1
- 206010018987 Hemorrhagic diseases 0.000 Description 1
- 210000001503 Anatomy of the joints 0.000 Description 1
- 2100003141 Anatomy of the lower limbs 0.000 Description 1
- 206010030113 Edema diseases 0.000 Description 1
- 2100003491 Anatomy of the skin 0.000 Description 1
- 2100003371 Anatomy of the toes 0.000 Description 1
- 2300002146 Bilateral effect 0.000 Description 1
- 23000052 Comparative Effects 0.000 Description 1
- 2300001054 Cortical effects 0.000 Description 1
- 238000002316 Cosmetic Surgery Methods 0.000 Description 1
- 238000003745 Diagnosis Methods 0.000 Description 1
- 229940079593 Medication Medication 0.000 Description 1
- 2300003203 Daily Impact 0.000 Description 1
- 238000002955 Isolation Methods 0.000 Description 1
- 2100001699 Anatomy of the lower limbs 0.000 Description 1
- 239000002184 Metallic substances 0.000 Description 1
- 238000010606 Standardization methods 0.000 Description 1
- 238000002559 Palpation methods 0.000 Description 1
- 239000004033 Plastics Materials 0.000 Description 1
- 2100001519 Tissue Anatomy 0.000 Description 1
- 230000001228 Trophic Effects 0.000 Description 1
Pictures
The invention relates to medicine, in particular to orthopedics and traumatology, and can be used to treat a tear of the distal intertibial syndesmosis. A posterior canal is formed in the tibia from the inside out, extending behind the lateral malleolus. Formation of a second bony canal in the lateral malleolus from back to front in the sagittal plane. Form an anterior canal in the tibia from outside to inside with an opening in front of the lateral malleolus. Pass the graft through the posterior canal until the larger bone fragment is wedged. Pass the graft through the second canal and into the anterior canal. At the exit of the anterior canal, the graft is maximally stretched and sutured to the tibia. This method prevents instability of the intercondylar joint. 3, Fig.
anatomy
The tibiofibular syndesmosis plays an important role in the stability of the ankle joint. To better treat this region, we need to know its anatomy.
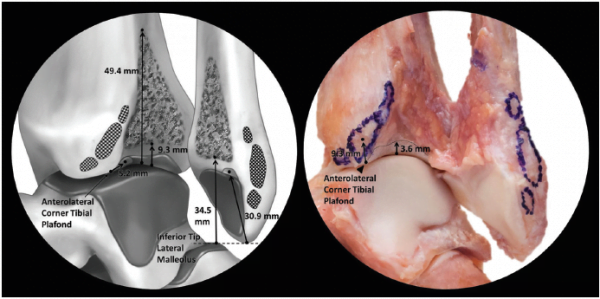
Inferior tibiofibular ligament
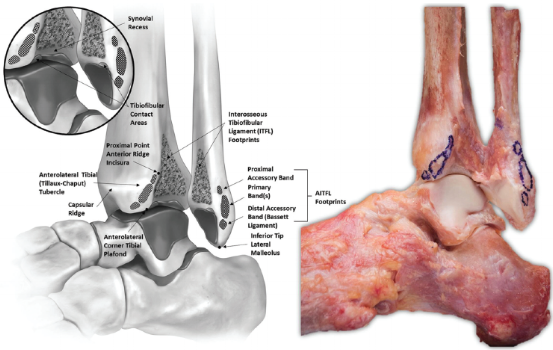
The inferior tibiofibular ligament (AITFL) begins at the anterior tubercle of the distal tibial epiphysis (9.3 mm above its lower edge), runs obliquely downwards at an angle of 35° and attaches to the anterior surface of the lateral malleolus (30.5 mm above its bottom edge). The band consists of 3-5 bands, depending on the individual anatomy. Together they form a trapezium with short additional fibers proximally and long main fibers distally.
Anterior inferior tibial ligament
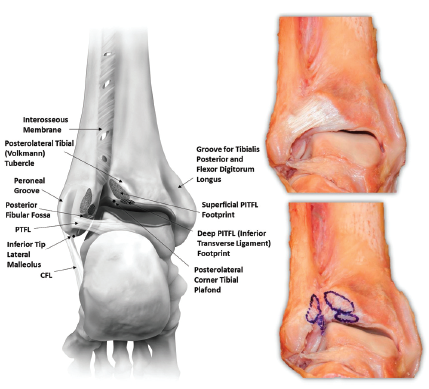
The posterior tibiofibular ligament (PITFL) is also trapezoidal. It is an extension of the overlying interosseous membrane. The posterior tibiofemoral ligament consists of two parts, the superficial and deep ligaments. The deep ligament is often referred to as the inferior transverse tibiofemoral ligament. The superficial fibers originate from the posterolateral tuberosity of the distal tibial epiphysis (8 mm above its lower border) and insert on the posterior surface of the fibula (26.3 mm above its lower border). The deep fibers are denser and their attachment points on the tibia are oval in shape.
diagnosis and treatment
Now that we know the anatomy of this region, our treatment must be more specific. In particular, we need to be able to palpate the anterior inferior tibial ligament (AITFL), as well as the tarsal ligaments: the anterior tibial ligament (ATFL), the posterior tibial ligament (PTFL), and the calcaneal ligament (CFL). Most physical therapists only palpate the distal epiphysis of the fibula to rule out a possible fracture and determine which talar ligament is damaged. However, we also need to check the anterior medial surface of the fibula and the anterior inferior tibiofibular ligament for swelling and pain. If pain occurs in this area, it is most likely a dislocation of the syndesmosis and the collateral ligaments of the ankle joint. In this case, the fibula should be pressed against the shinbone and the talus area should be stabilized. The patient should avoid dorsiflexion of the foot (e.g. during deep knee bends or calf stretches).
This video demonstrates ankle taping. This technique was developed by Brian Mulligan. This type of taping is used on people after an ankle sprain. The aim is to reposition the syndesmosis of the distal part of the tibia, resulting in a significant increase in range of motion and a reduction in pain.
Sources:
Ebraheim, N.A., Taser, F., Shafiq, Q., & Yeasting, R.A. (2006). Anatomical evaluation and clinical significance of the tibial syndesmotic ligaments. Surgical and radiological anatomy, 28(2), 142-149.
Golano, P., Vega, J., de Leeuw, PAJ, Malagelada, F., Manzanares, MC, Gotzens, V., & van Dijk, CN (2016). Anatomy of the ankle ligaments: a pictorial essay. Knee Surgery Sports Traumatology Arthroscopy, 24(4), 944-956.
Types of pinched lower back nerve in men and women
The classification is based on the duration of symptoms and the time of their onset. So, spinal cord root compression can be divided into three types: acute (occurs suddenly and lasts 1 month), subacute (symptoms last 3 months) and chronic (lasts more than 3 months).
A pinched nerve in the lower back is a sharp pain that is very difficult to endure. It can radiate into the buttocks or the leg. Some parts of the lower limbs are numb, muscle weakness occurs, the previous sensitivity of the legs is impaired, and movement in the back area is restricted.
The pain can also manifest itself in the form of stabbing cramps and severe back pain. The extent of the pain increases with each passing day. This is because the complaints from the various nerve roots are concentrated in a single, very problematic nerve root. This also causes the spine to pulsate even more strongly.
In the case of a herniated disc, the symptoms of a pinched nerve are slightly different. For example, in a calm state, the pain is mild but persistent. If the affected person suddenly sneezes, coughs or does physical activity, the pain increases significantly. However, if you lie down with your legs bent, the pain stops.
What are the symptoms of a pinched nerve in the spine? When a radius is compressed in an anatomical canal, pain increases slowly rather than quickly. It gradually spreads to the legs, entire back and pelvis. Trying to get into a lying position often doesn't help stop the pain. In this situation, you should simply sit upright. Then the pressure on the radius bone decreases and the symptoms disappear.
Depending on which level of the spine the dorsopathy occurred, additional symptoms of radial joint stiffness may occur. For example, compression at the L3 level leads to a loss of feeling in the knees and lower legs. Compression at the level of L5 results in decreased sensation in the inner part of the foot and tibia (outer part of the shinbone).
Diagnosis of dorsopathy
First, the doctor carries out a comprehensive examination. Visually examines the lower back, pressing on the different levels and identifying painful areas, listening to the person's complaints and his history of the occurrence/development of the pathology. Next Steps:
- The doctor then asks the patient to perform various physical exercises to determine the response of the nerve root and the entire spinal cord.
- He then carefully examines the condition of the skin where the pressure was applied.
- He conducts a neurological examination.
- In most cases, these measures are enough to make an accurate diagnosis. However, the doctor may take x-rays in two projections (lateral and direct).
- He may also order an MRI or CT scan.
- If there is suspicion that the spinal cord is compressed, the doctor will recommend myelography and electroneuromyography.
These examinations must be carried out using modern medical equipment so that false information is not obtained. The clinic of Dr. Long (in Moscow) has innovative diagnostic equipment for examining a person with a compressed nerve root in the spinal area.
Chief chiropractor, osteopath, chiropractic neurologist
Experience for 18 years In our clinic we successfully use a wide range of techniques, including both traditional and state-of-the-art treatment methods. Our specialists are proficient in a variety of techniques: craniosacral therapy, post-isometric relaxation, palsing, myofascial release, short and long-arm techniques, etc.
- Training as a chiropractor at the world-famous Charité in Germany in 2003,
- Chiropractic training in Los Angeles, New York (USA, 2015).
- Studying the treatment of large herniated discs with the head of the Department of Spinal Urology, Tsib V.
- He has summarized the best of the known techniques in his own method that really helps in difficult cases.
Rupture of the distal intertibial syndesmosis
The rupture of the syndesmosis can be partial or complete. If the intertrochanteric syndesmosis is partially ruptured, it is still possible to move independently. However, this causes severe pain. No significant separation of the tibia and fibula can be seen on the x-ray.
A complete rupture of the distal syndesmosis is characterized by separation of the tibial and fibular condyles by 4 cm or more. The patient is unable to walk without assistance. There is significant ankle deformity.
A distal intertibial syndesmosis tear is an injury that requires immediate medical attention from a trauma surgeon. It is not possible to heal such an injury on your own. In severe cases, surgery may be necessary.
Consequences of a torn syndesmosis of the ankle joint
The syndesmosis of the ankle joint is the most important anatomical structure for permanently fixing the bones and keeping them in a stable position in the joint capsule. Large blood vessels and nerves run through them. They supply the tissues of the foot and toes with blood and nutrients.
Therefore, with a syndesmotic rupture of the ankle joint, the following types of side effects are often observed:
- Disturbance of soft tissue trophism, which in severe cases can lead to necrosis and the development of dry gangrene, trophic ulcers, in milder cases the skin begins to peel and a rupture of the integrity of the skin occurs, a pale color and a Reducing the intensity of pulsation;
- Disruption of the innervation of foot tissues, including muscles, which can lead to paresis, paralysis and even atrophy (decreased muscle strength and lack of mobility of the toes);
- Unstable position of the bone heads in the ankle joint, leading to the development of deforming arthrosis;
- Increased cushioning load on other tendons and ligaments in the ankle area;
- Lameness, limited mobility, contractures.
A complete rupture of the ankle joint syndesmosis can lead to complete separation of the tibial and femoral condyles if not treated in a timely manner. This leads to severe deformity of the lower limbs and loss of joint mobility. The affected person may be disabled for the rest of their life.
treatment methods
Modern traumatology and orthopedics has a rich arsenal of treatment options for this problem. The most effective techniques include:
- Standard arthroscopy. It allows assessment of the condition of the damaged tissues, confirmation of syndesmosis injury and identification of accompanying tears, e.g. B. the adjacent cartilage or the deltoid ligament.
- Tendoplasty, which ensures the restoration of the ankle joint. In this procedure, channels are drilled into the shinbone into which the doctor implants a new ligament.
- A brace and a compression screw, which are used to fix and immobilize the shin bones, prevent displacement and stiffening.
- The 'button system' is a method that maintains physiological mobility in the joint area and creates the conditions for the healing of the ligaments.
The Endobutton devices are not inferior to screws in terms of fixation, but they allow patients to undergo rapid rehabilitation, allowing them to quickly return to their normal lives without the need to remove screws.
During the operation, the surgeon takes into account the possibility of serious vascular diseases and the risk of thrombosis in the lower limbs. If necessary, he prescribes medications to improve metabolism and the integrity of the vascular walls. A complex of surgical and pharmacological treatments helps the patient recover as quickly as possible.

The success of the treatment depends to 90 % on the doctor's experience and qualifications.
Free medical advice and diagnosis
During the consultation, we carry out a thorough diagnosis of the entire spine and each of its segments. We determine exactly which segments and nerve roots are affected and cause the pain symptoms. As a result of the consultation, we give detailed treatment recommendations and, if necessary, prescribe additional diagnostics.
We carry out a functional diagnosis of the spine
We carry out a manipulation that leads to significant pain relief.
We set up an individual treatment program.

Since an ankle fracture is an intra-articular injury, intra-articular injuries always require the help of a trauma surgeon as well as a rehabilitator.
This is much more common in the winter time. Fractures of the ankle joint are therefore the most common winter injury. The foot can be twisted outwards and inwards. Typically, an ankle fracture is a combination of ligament and bone injuries, with ligament injuries playing just as important a role as bone injuries and bone fractures. The possibility of conservative or surgical treatment depends on this combination of soft tissue injury and bone fracture.
If you have an ankle fracture, it is important to see a doctor as soon as possible. A correct diagnosis is important here because ankle fractures can be very, very different. It is important to get a specialist's opinion on whether and how surgery is necessary.
As far as the anatomy of the ankle is concerned, there is the lateral malleolus, which is a natural extension of the fibula, and the medial malleolus, where the tibia ends. The outer malleolus and the inner malleolus, together with the shinbone, form what is known as the fork of the ankle joint. In this foramen is the talus, whose main movements are flexion and extension. The human foot can rotate outward and inward, supinate or pronate, that is, bend inward or outward, but only within certain limits. When these boundaries are violently and unintentionally violated, a rupture occurs. For example, a person slips, all the weight is on one foot - the bone cannot bear the load. A triquetral fracture and a 'posterior ankle' are sometimes referred to. In reality, there is no such thing as a back ankle. But this term exists because there are strong posterior intercondylar syndesmotic ligaments attached to the back of the tibia. This is sometimes referred to as Folkman's triangle. In some injuries, the ligaments are stronger than the bone and Folkman's triangle is torn. In this case one speaks of a fracture of the triangle.
Journal of Trauma Vol. 11, No. 4, 2010

Based on the literature, the function of the intertibial syndesmosis was analyzed from the perspective of ankle joint stability. The conclusion is that in the treatment of ankle injuries associated with damage to the intertibial syndesmosis, it is necessary to preserve the mobility of the fibula relative to the tibia.
Based on the literature, the function of the intertibial syndesmosis is analyzed from the perspective of ankle stability. It is concluded that in the treatment of ankle injuries associated with a tear of the intertibial syndesmosis, it is necessary to preserve the movement of the fibula relative to the tibia.
Based on literature data, the function of the tibial syndesmosis is analyzed from the aspect of ankle stability. It is concluded that when treating ankle injuries with tibial syndesmosis injury, mobility of the fibula rather than the tibia must be preserved.
The ankle joint is a true synovial joint of complex configuration and irregular shape, located between the tibia and the foot bone. The tibia and fibula are connected distally by a connective tissue formation, the intertibial syndesmosis, which is connected along its length to the interosseous membrane [1,2].
Although the anatomical and functional features of the ankle joint have been described in detail, the issue of mobility of the distal intertibial joint and its role in ankle function is only sporadically addressed in the literature. This question usually arises in connection with the validity of treatment tactics for ankle injuries with ruptured syndesmosis [35]. Clinicians have repeatedly demonstrated that the tibia is mobile using radiographs, ultrasound scans, and experimental studies on cadavers. This mobility is approximately 2.3 mm and can be verified (6,7). These data, together with anatomical data on the structure of the talar block, have provided a strong concept of anterior mobility of the tibia, which is due to the difference in width of the talar block, which is slightly wider in the anterior region and narrower in the posterior region. Therefore, when the foot is extended, the talus tends to push the tibia apart. Contrary to clinician belief that there is anterior mobility of the tibia, it is generally accepted by anatomists that there is rotational mobility of the fibula as well as vertical mobility of the tibia (8-10). While the question of the presence of mobility in the intercondylar syndesmosis can be answered positively, the question of its nature and purpose remains open.
How do ankle injuries occur?
Rupture of the ankle ligaments often occurs as a result of a fall or trauma during sporting activities. The ligaments lose their stabilizing function and patients can no longer move as before. The outer ligaments are most susceptible to injury. In almost all collateral ligament injuries, the anterior ligament of the hip is injured.
Risk factors such as obesity, incorrect footwear and poor physical training can cause a tear or sprain.
Symptoms of torn ligaments

Injuries to the external collateral ligaments are associated with severe pain and the formation of hematomas. © Leo, Fotolia
Ankle pain and swelling are typical symptoms of a sprain and are often confused with a simple sprain and not treated by a doctor. Hematomas can also occur as a result of ruptured popliteal veins. Other symptoms include ankle pain and the inability to elevate the leg. The injury usually leads to a limitation in exercise capacity that can last for several days and sometimes weeks.
If the victim is unable to stand on the leg, it is likely that the leg is completely torn.
ICD-10


A synostosis is the connection of several bones together. The consequences depend on the location of the synostosis and can be asymptomatic or even life-threatening. Synostosis is distinguished from joint stiffening (ankylosis) and stiffening of bone fragments after a fracture (consolidation). Synostosis is treated by orthopedic traumatologists.

Causes of synostosis
Natural bone gaps are anatomically normal, occur at certain periods of life and have no negative consequences. Natural synostoses include, for example, pelvic bone fusion in adults. Pathologic synostosis can be caused by trauma, abnormal fetal development, or certain infections.
Physiological synostosis is the normal fusion of bones that occurs during puberty. Normal synostosis occurs during puberty and adolescence at the site of synchondrosis (cartilaginous connections) between the pelvic bones, sacral vertebrae, and skull base bones. In hypergonadism, eunuchoidism, Kashin-Beck disease and some other diseases, this process is delayed or accelerated, which can lead to disorders of the musculoskeletal system.
Congenital synostosis
Pathological fusion of bones caused by hypoplasia or aplasia of the connective tissue between bones. It most commonly occurs between the ulnar and radial bones. Less common are craniostenosis (premature fusion of two or more cranial sutures), synostosis of the nail and the middle phalanx of the fifth finger, and synostosis of the carpal bones. The literature describes cases in which the phalanges of adjacent fingers are fused in syndactyly, several normally developed ribs have grown together, and the first rib and the costal process of the cervical spine have fused. Vertebral synostoses develop in Klippel-Feil syndrome. Antley-Bixler syndrome is characterized by a variety of pathologic fusions, including craniostenosis, tarsal synostosis, epiphyseal synostosis, carpal tunnel synostosis, brachioradial synostosis, and radial condyle synostosis.
Post-traumatic synostosis
This is the fusion of adjacent bones caused by damage to the bone, epiphyseal cartilage, or periosteum. Synostosis most commonly occurs between the tibia, forearm, and adjacent vertebrae. Synostosis of the ulna and radius, as well as the fibula and tibia, is in most cases caused by a coincidence of fractures of these bones at the site of injury. Spinal synostoses arise from ossification of the anterior longitudinal ligament after peripheral shaft fractures and vertebral misalignments.
Intercorporeal syndesmosis injury – treatment in St. Petersburg (SPb)
What's special about treating this injury is the importance of immediate first aid. Because this injury is accompanied by a sharp deviation of the foot to the side, which leads to disruption of the innervation and blood supply to the soft tissues.
First aid should be to apply a splint to immobilize the joint and leave it in a still position until the ambulance arrives.
Treatment is prescribed by the doctor after a thorough examination. Diagnosis is made through palpation and anamnesis, as the injury is visible 'from afar'.
Treatment is usually conservative, that is, with pain-relieving and anti-inflammatory medications as well as a removable splint that must be worn for 14 days.
If the injury is complicated and the dislocation is significant, the doctor prescribes surgery: atroscopy, tendoplasty and other surgical interventions.
These techniques can be combined to achieve the best possible result. When we talk about plastics, it involves strengthening the ligaments with a strip of the patient's own hip fascia.
Prices for treatment of intertibial syndesmosis injury in St. Petersburg (SPb)
To find out the prices, how much the treatment of an intertrochanteric syndesmosis injury costs in St. Petersburg and how much the intertrochanteric syndesmosis injury operation costs, please call the clinic or make an initial appointment with a specialist in our clinic.
| Treatment of intertrochanteric syndesmosis injury, price | 10,000-30,000 rubles. |
| Consultation with a specialist in the treatment of intertibial syndesmosis injuries, price | 600-1,600 RUBLES. |
- syndesmosis.
- Anatomy of the syndesmosis.
- The intercondylar joint.
- Injury to the navicular semilunar ligament.
- pelvic subluxation.
- The lateral ankle is.
- fibula.
- Growth zones of the foot bones.


