The difference between the function of the ankle joint and the knee joint is that in addition to the flexion, extension and rotation movements of the foot, push-off movements of the foot are also required. Furthermore, these movements of the foot cannot be mutually exclusive and occur together [16]. What is the anatomical solution to this problem? Is the presence of the fibula a solution? And if so, what is the mechanism of their involvement?
- Closed knee injuries
- Short description
- Clinic automation: fast and cheap!
- Clinic automation: fast and cheap!
- classification
- Journal of Trauma Vol. 11, No. 4, 2010.
- classification
- causes
- Mechanism of creation.
- classification
- Main symptoms
- Ligament injuries – tibial joint
- information
- synostosis
- This will be explained by a specialist from CMRI.
- Causes of synostosis
- Specific features of the injury
- Main symptoms of injury
- Therapeutic exercises after surgery
- Causes of synovial cysts
- Which doctor should I see?
- Our specialists
- Prices for Services
Closed knee injuries
ICD categories: Fresh meniscus tear (S83.2), Fresh knee cartilage tear (S83.3), Strain, tear and overstretching of the (external) (internal) collateral ligament (S83. 4), Strain, tear and overstretching of the (anterior) (posterior). ) cruciate ligament (S83. 5), sprain, tear and strain of other and unspecified parts of the knee joint (S83.6), injury to multiple structures of the knee joint (S83.7), contusion of the knee joint (S80.0).
Short description
Closed knee joint injury – Injury to the structures of the knee joint without skin injury caused by mechanical energy [1].
Users of the protocol: Orthopedic traumatologists, surgeons, general practitioners, emergency physicians, paramedics.
Class I – the usefulness and effectiveness of the diagnostic method or treatment measure has been proven and/or generally accepted
Class III - the available evidence or general consensus suggests that the treatment is not useful/effective and may even be harmful in some cases
B – Results from a single randomized clinical trial or large non-randomized trials
C – General expert opinion and/or results of small studies, retrospective studies, registries.

Clinic automation: fast and cheap!
– 800 RUB / 5500 KZT / 27 BYN – 1 order per month

Clinic automation: fast and cheap!
classification
II. DIAGNOSIS AND TREATMENT METHODS, APPROACHES AND PROCEDURES
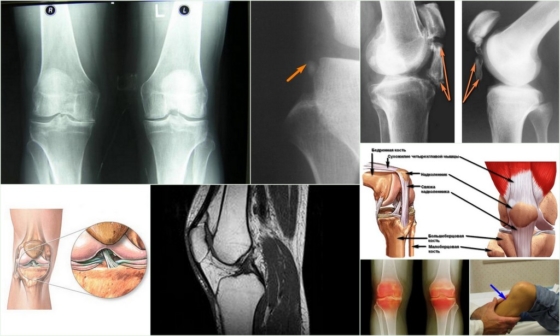
4. Magnetic resonance imaging of the knee joint (indications: torn, dislocated and damaged knee ligaments)
Minimum list of examinations to be carried out upon referral for a planned hospitalization: No planned hospitalization.
1. Magnetic resonance imaging of the knee joint (indications: ligament tears, sprains and injuries of the knee)
Collection of complaints and anamnesis, physical examination.
Medical history: Presence of trauma with a direct (severe blow to the knee, fall on the knee) or indirect (acute rotation of the trunk with a standing foot) mechanism of injury.
3) Gross pathological mobility in the area of the knee joint.
– Two-dimensional x-rays of the knee joint: no bony pathology, but secondary signs of soft tissue damage: widening of the joint space, spreading of the syndesmosis.
– MRI: Signs of damage to the ligamentous apparatus of the tendon sheath and tendon are detected.
Journal of Trauma Vol. 11, No. 4, 2010.

Based on the literature, the function of the intertibial syndesmosis was analyzed from the perspective of ankle joint stability. The conclusion is that when treating ankle injuries associated with an intertibial syndesmosis injury, it is necessary to preserve mobility of the fibula relative to the tibia.
Based on the literature, the function of the intertibial syndesmosis is analyzed from the perspective of ankle stability. It is concluded that in the treatment of ankle injuries associated with a tear of the intertibial syndesmosis, it is necessary to preserve the movement of the fibula relative to the tibia.
Based on literature data, the function of the tibial syndesmosis is analyzed from the aspect of ankle stability. The conclusion is that when treating ankle injuries with worsening tibiofibular syndesmosis function, mobility should be preserved in the fibula, not the tibia.
The ankle joint is a true synovial joint of complex configuration and irregular shape, located between the tibia and the foot bone. The tibia and fibula are connected distally by a connective tissue formation, the intertibial syndesmosis, which extends along the length of the intertibial membrane [1,2].
Although the anatomical and functional features of the ankle joint have been described in detail, the issue of mobility of the distal intertibial joint and its role in ankle function is only sporadically addressed in the literature. This question usually arises in connection with the validity of treatment tactics for ankle injuries with ruptured syndesmosis [35]. Clinicians have repeatedly demonstrated that the tibia is mobile using x-ray and ultrasound data as well as experimental studies of cadaveric material. This mobility is approximately 2.3 mm and can be verified (6,7). These data, together with the anatomical data on the structure of the talar block, have given rise to a strong concept of anterior mobility of the tibia, which is due to the difference in the width of the talar block, which is slightly wider in the anterior region and narrower in the posterior region. Therefore, when the foot is extended, the talus tends to push the tibia apart. Contrary to clinician belief that there is anterior mobility of the tibia, it is generally accepted by anatomists that there is rotational mobility of the fibula as well as vertical mobility of the tibia (8-10). The question of the presence of mobility in the intertibial syndesmosis has therefore been answered positively, but the question of its nature and purpose remains open.
classification
The condition is classified under ICD-10 code M23.8, Other Internal Knee Lesions. A number of diseases fall into this group, including ligamentitis of the knee joint. There is no specific classification for this pathology, and only the affected ligaments are taken into account in the diagnosis:
Most commonly, inflammation of the cruciate ligament occurs, resulting in impairment of full extension, severe pain, and limited rotation of the tibia during knee flexion.
causes
Cruciate ligament inflammation occurs most often in athletes, as frequent injuries or damage to the ligamentous joint are a trigger. Older people with osteoarthritis are also at risk.
The most common causes of band formation:
- From the age of 30, the body's natural aging process, pre-programmed by nature, begins. The ligaments in the knee joint also undergo these changes - they become less flexible and the likelihood of tearing increases dramatically;
- Frequent inflammation of the ligaments – inflammatory damage to a ligament increases the risk of ligament destruction;
- Recurrent trauma – even minor injuries can trigger the pathological process of the disease;
- Recurrent arthritis and osteoarthritis of the knee joint - Inflammation and thinning of the cartilage compromise the integrity of the ligament attachments to the periosteum, which may result in a ligamentotomy of the knee joint;
- Sedentary lifestyle, lack of moderate physical activity – promotes laxity of ligaments and increases the risk of ligament injuries.
Danger!!!
Due to their structure, the ligaments have very little stretch - they tear easily under heavy loads. When the load is low, the fibers no longer return to their original length.

Mechanism of creation.
It is characterized by the interruption of one or two links that are responsible for the mobility of the joint. In most cases, there is complete or partial destruction of the cartilage, leading to fusion of the articular surfaces. Inflexible fibrous tissue grows in or around the joint. Less commonly, fusion of the cartilage itself occurs. This leads to partial or complete loss of mobility.
classification
Ankylosis is classified according to the type of fusion:
- In the fibrous type, the bones are connected to each other by fibrous tissue. X-rays show deformation of the joint space. The function of the joint is almost completely impaired and mobility is hardly present. The pathology occurs with prolonged immobility and chronic, non-pneumonic processes.
- The bony type is a complication of purulent arthritis, an intra-articular fracture. All bones in the affected area fuse together. No joint space can be seen on the x-ray and the joint is completely immobilized.
- The cartilaginous type, a consequence of arthrogryposis, is diagnosed in young children. The x-rays show an abnormal configuration of the joint ends and the affected joint is immobile.
Depending on the extent, the ankylosis is complete or partial. Depending on the localization, the pathological process can occur outside the joint, inside the joint or mixed.
Main symptoms
The main symptom is the lack of mobility of the affected joint. Initially there is morning stiffness which resolves after 20-30 minutes, but as the disease progresses the stiffness increases.
During the inflammatory process, the soft tissue over the affected joint is swollen, red and hot to the touch. In the fibular type, pain occurs with muscle contraction or at rest, but no pain with bone fusion. The joint is in a fixed position for greatest mobility or complete mobility.
- Shoulder joint – moderate forward extension with outward extension;
- Elbow joint – flexion up to 90 degrees;
- Hip joint – slight adduction and flexion;
- Knee joint – slight flexion;
- Ankle – just over 90 degrees.
With this immobilization, the patient is still able to care for themselves and move.
The external symptoms are varied: gross deformities in which the limb is distorted or shortened, and localized joint deformities.
Ligament injuries – tibial joint
The bony base of the human tibia consists of two bones: the tibia and the fibula.
In the lower limb they are connected to each other by two ligaments: the anterior and posterior interosseous ligaments. These ligaments limit the mobility of the shinbone and stabilize the ankle joint.
An injury to the intertibial ligaments occurs when the foot is turned inward while the shinbone is turned outward.
Pubic ligament injuries are often accompanied by an ankle fracture, but rarely occur alone.
Patients complain of pain in the lower part of the shinbone when walking and moving the ankle. The pain increases when the ankles are squeezed or when the shinbone is squeezed.
X-rays show an increase in the gap between the tibia and fibula compared to the healthy side of the tibia and fibula.
Treatment of ligament injuries in the tibial joint.
In case of an incomplete ligament tear To relieve pain, local anesthetics (Novocaine, Lidocaine) are injected into the torn area; If pain persists, the injection is repeated after a few days.
Physiotherapeutic treatments (use of paraffin and ozokerite, other heat treatments) and massages are recommended.
In the event of a complete ligament tear To reduce the gap between the bones, pressure is applied to the ankles and a plaster cast is applied from the toes to above the knee joint.
If conservative treatment is unsuccessful, surgical treatment is indicated.
The skin above the ankles is cut open. A hole is drilled through the fibula and tibia, a screw is inserted into the resulting channel and a nut is screwed in, which brings the fibula and tibia closer together. A plaster cast is then applied for five to six weeks.
(495) 50-253-50 – Free advice about clinics and specialists
- Joint operations – types
- Hip joint – joint replacement
- Hip joint – structure
- Hip joint – diseases
- Hip joint – hip joint replacement operations
- Hip joint – prostheses
- Hip – hip joint replacement
- Hip joint – minimally invasive prosthetics
- Minimally invasive technique
- Computer-assisted prosthetic technology
- Surgical approach
- Knee joint – endoprosthetics
- Knee joint – structure
- Knee joint – indications for surgery
- Knee joint – surgical risks
- Knee joint – after knee replacement
- discharge home
- rehabilitation time
- Rehabilitation period Social adaptation
- Knee Joint – Living with a Knee Joint Replacement
- Knee joint – replaced
- Replacement of a shoulder joint
- coxarthrosis
- Coxarthrosis – symptoms
- Coxarthrosis – diagnosis, treatment
- Osteoarthritis, arthrosis
- Gonarthrosis – causes, symptoms
- Gonarthrosis – diagnosis, treatment
- Osteoarthritis of the knee joint
- meniscus
- Meniscus – types and symptoms of damage
- Meniscus – diagnosis and treatment
- Meniscus – cystic degeneration
- Meniscus – meniscectomy
- Becker cyst
- Knee joint – arthroscopy
- Knee joint – arthroscopy technique
- Knee joint – complications of arthroscopy
- Ligament injury
- Ligament injury – intercostal joint
- Ligament injury – kneecap
- Ligament injury – cruciate ligaments of the knee joint
- Ligament injury – lateral knee joint
- Ligament injury – metacarpophalangeal joint 1
- Ligament injury – lateral interphalangeal joint
- Ligament injury – wrist
- Achilles tendon – rupture
- Carpal tunnel syndrome – causes
- Carpal Tunnel Syndrome – Treatment
- Posture – types of posture problems
- scoliosis
- The spine – malformations
- The spine – lumbar and sacral spine
- Spine – bulging vertebrae
- Spine – Tropism
- Spine – spondylolysis
- Spine – vertebral sliding (spondylolisthesis)
- osteochondrosis
- Osteochondrosis – cervical
- Osteochondrosis – thoracic
- Osteochondrosis – lumbar
- Congenital torticollis of the neck
- Congenital torticollis – treatment
- Osteochondropathies – types
- King's disease
- osteosynthesis
- Thorax – Deformities
- Upper limbs – congenital anomalies
- Lower limbs – extensions
- Lower Limbs – Complications After Lengthenings
- Congenital hip dislocation – symptoms
- Congenital hip dislocation – treatment
- flat feet
- Clubfoot Diagnosis
- Clubfoot – prevention
- clubfoot
- osteotomy
- Osteotomy – hip
- Osteotomy – tibia
- Resection of bones
- Big toe deformity
- Hallux valgus – prevention
- Hallux valgus – treatment
- heel spur
- Heel Spur Treatment
- Ingrown toenail
- Nail debridement
- Injuries in athletes
- Sports injuries – tendon rupture
- Injuries in athletes – tendon rupture
- Injuries in athletes – torn muscle fibers
- Injuries in athletes – muscle hernia
- Foot curvature – correction
- Pain - arch of foot
- Pain – toe joints
- plantar fasciitis
- Plantar fasciitis – surgical treatment
- Plantar fasciitis – surgery
- Tarsal tunnel syndrome
- hollow foot
- Diabetic foot
- Deformed toes
- Osteoarthritis of the ankle
- Achilles tendinitis
- Lower limb deformities – symptoms
- Lower leg deformities – causes
- Lower leg deformities – conservative treatment
- Lower leg deformity – surgical treatment
- Lower leg deformity – complications during surgery
- spine
- Spine – research
- Spine – myelography
- Spine – Radiography
- Spine – discography
- Spine – lumbar puncture
- Spine – EMG, ENG
- Spine – magnetic resonance imaging
- Spine – CT scan
- Intervertebral hernia – diagnosis, prevention
- Intervertebral hernia – risk factors
- Intervertebral hernia – symptoms
- Intervertebral hernia – cervical spine
- Intervertebral hernia – non-surgical treatment
- Non-steroidal anti-inflammatory drugs
- Corticosteroid medications
- Myorelaxants
- Antidepressants
- Intervertebral hernia – surgical treatment
- Microdiscectomy
- Percutaneous discectomy
- Laminectomy
- Intervertebral hernia – choice of operation
- sciatica
- Sciatica – symptoms
- Sciatica – Medication
- Sciatica – surgical treatment
- Stenosis of the spinal canal
- Spinal canal stenosis – symptoms
- Spinal canal stenosis – conservative treatment
- Spinal canal stenosis – surgical treatment
- Cervical spinal stenosis – treatment
- Spondylolisthesis isthmicus
- Degenerative spondylolisthesis
- Cauda Equina Syndrome – Causes
- Cauda equina syndrome – differential diagnosis
- Vertebral Equinus Syndrome – Treatment
- Ankylosing spondylitis
- Ankylosing spondylitis – symptoms, diagnosis
- Ankylosing spondylitis (Bechterew's disease) - treatment
- Intradiscal electrothermal energy
- VET – Orthopedic Clinic Kassel
- scoliosis
- Scoliosis – treatment
- Vertebroplasty
- Kyphoplasty
- Spondylolodesis
- Foreign medical centers – spine treatment
- Spinal fusion
- Laminectomy – surgical technique
- Discectomy procedure
- new technologies
- Joint endoprosthesis – Israel
- Knee joint for women
- hip joint
- Orthopedic Surgery
- ENDO Clinic – Hamburg
- Hip joint arthroplasty
- Hip joint – types of prostheses
- Hip joint – dysplasia
- Hip joint – hip joint replacement
- Knee replacement
- Knee Joint – Types of Knee Joint Replacements
- Shoulder joint – latest prostheses
- Shoulder joint – joint replacement
- arthroscopy
- ENDO Clinic – Department of Neurosurgery
- ENDO Clinic – Department of Anesthesiology
- price overview
- Orthopedic clinic in Kassel
- Kassel Clinic – Arthroscopic Surgery
- Kassel Hospital – cutting-edge technology
- Mühlengrund Rehabilitation Clinic
- Kassel Hospital – knee surgery for women
- Kassel Hospital – intervertebral disc surgery
- Kassel Clinic – treatment of spinal fractures
- Kassel Clinic – Treatment of articular cartilage injuries
- Kassel Clinic – provision of shoulder prostheses
- Kassel Clinic – treatment of children and adolescents
- Kassel Hospital – sports injuries
- Kassel Clinic – Spinal therapy
- Kassel Clinic – Diagnostics Department
- Kassel Clinic – treatment of rheumatoid arthritis
- Kassel Clinic – Orthopedics
- Kassel Clinic – Conservative treatment
- Kassel Clinic – Surgical treatment
- Kassel Clinic – Surgical navigation systems
- Kassel Clinic – patient advice
- Kassel Clinic – operations for serious injuries
- Kassel Clinic – treatment costs
- Germany – intervertebral disc prosthesis
- Pediatric orthopedics – Germany
- Cartilage implantation
- Cartilage reconstruction
- Levinstein Rehabilitation Center – Israel
- Total joint replacement – Latvia – Riga
- The best German orthopedists – Prof. W. Siebert – Kassel
- Anterior cruciate ligament plasty – a new technique
information

The best experience in Russia in surgical treatment of patients with thoracic defects (VDHK, KDHK, Polanda syndrome).

Dr. Pekarski is currently the most sought-after spine surgeon in Israel. Dr. Pekarski performed successful spinal surgery on figure skater Yevgeny Plushenko – video report on Channel 1.
Creation of an individual implant depending on the severity of the deformity. The procedure is carried out by Dr. Korolev, MD, thoracic surgeon.
synostosis
This condition is treated by a neurologist.
Synostosis is a pathological or physiological continuous fusion of bones in bone tissue. In medicine it is usually referred to as abnormal fusion of bones. The main causes of this pathology, as well as methods of diagnosis and treatment will be discussed.
This will be explained by a specialist from CMRI.
Date Published: August 15, 2022 Date Reviewed: February 23, 2023 All facts have been verified by a doctor.
Causes of synostosis
This diagnosis can be made in a child or an adult based on the results of examinations.
The symptoms of the disease depend on which part of the skeleton has undergone pathological fusion. With radial elbow synostosis, which is characterized by fusion of the ulnar and radial bones, patients complain of significant limitation in mobility of the upper limbs. Simple self-care activities are difficult. The abnormal fusion of the skull bones leads to incomplete brain development and changes in the shape of the skull.
- Decreased number of cervical vertebrae in Klippel-Feil syndrome
- Reduced length of neck and limbs
- Spina bifida
- Headaches and cramps
- Impairment of mental development
- reduced ability to work
Rib synostosis and premature sternum anastomosis are sometimes discovered incidentally on x-rays.
Specific features of the injury
Injury to the distal joint is accompanied by a rupture of the intercondylar membrane between the tibial bones in the lower third. The injury leads to mobility problems. The injury compromises the integrity of the joint and the bones involved. Most often, a tear occurs in people who put a lot of strain on their limbs during their activities. In most cases, ankle injuries are observed in ballerinas, circus performers and runners.
It looks like an isolated sprain, but is often associated with a bone fracture or tear of some ligament fragments. This leads to acute and unbearable pain. A person suffering from this type of injury needs urgent treatment.
Injury to the cranial or spinal syndesmosis can have serious consequences. In particular, the injury can occur in a newborn during the birth process. In this case, the intervertebral membrane of the skull is damaged and bleeding may occur. In a compression fracture, the syndesmosis is not completely torn. Only partial damage or stretching occurs.

Main symptoms of injury
After a serious injury, clear symptoms appear immediately. The affected person feels unbearable pain that extends to the entire affected area. The pain increases when the ankle is felt, which is very uncomfortable for the injured person. The swelling develops gradually and increases minute by minute.
The torn ligament is accompanied by an unnatural position of the foot. The foot is often turned outwards due to the severe swelling. The area of injury is hyperemic. The examination shows a source of bleeding.
An x-ray is required for an accurate diagnosis. The person is unable to care for the injury independently. Increasing pain and swelling cannot be treated with painkillers and anti-inflammatory medications.
An x-ray helps rule out dislocations and additional damage. X-rays show exactly which areas are affected. A competent specialist can then prescribe the appropriate treatment. Anyone who experiences acute pain due to an injury or after sporting activities should go to hospital immediately.
Therapeutic exercises after surgery
As part of rehabilitation, each patient is offered an individual exercise plan by a specialist from the Master Health Clinic to restore the function of the knee joint after surgery.

Kryukov Alexander Sergeevich,
Chief physician of the health workshop,
Orthopedic Traumatologist
Release date:
July 30, 2018
Update date:
02.08.2021 г.
Causes of synovial cysts
Often the neoplasm occurs in the vertebral arches or roots, less often in the vertebral bodies themselves. The specialists dealing with this pathology have not determined the actual cause of its formation. However, they have identified a number of conditions that can lead to cyst formation. The most common include:
Provocative factors can aggravate the situation and accelerate the development of synovial cysts. This includes:
- The effects of mechanical trauma;
- sedentary lifestyle;
- instability of the joint;
- Excessive and irregular muscle activity;
- Congenital bone anomalies;
- metabolic disorders;
- Infections with helminths.
In addition, poor nutrition can promote the formation of a synovial cyst. A nutrient deficiency affects the entire body, including the joints.
Which doctor should I see?
A synovial cyst, regardless of its location, has a negative impact on the patient's well-being. It also puts pressure on nearby tissues, nerve endings and vessels. Therefore, if you notice unpleasant symptoms, you should go to a medical facility. The diagnosis and treatment of this condition is usually carried out by our specialists:
Our specialists
The prices stated on this page are not a public offer. Please call 8 (495) 255-37-37 to find out the cost of services and make an appointment with a doctor.
Prices for Services
In some cases, an arthrologist, trauma surgeon, and infectious disease specialist may also be called upon to treat the cyst. However, the doctor must familiarize himself with the patient's condition before determining the method of treatment. To do this, he carries out a series of necessary steps, viz
- He will listen to the patient's complaints;
- He asks how often the patient is exposed to physical exertion;
- He will take a medical history;
- He asks whether the patient has a predisposition to being overweight;
- ask a series of questions about the patient's condition.
- The intercondylar syndesmosis is the.
- Dislocation of a bone in a joint.
- Schopar'sche joint.
- The key to a chopper joint is.
- Shapar joint.
- Lisfranc joint.
- pelvic thigh joint.
- The Chopara joint forms 2 joints.
