There are currently no recommendations for arthrodesis when interventional procedures do not provide pain relief. Surgery may be indicated for grade I or II spondylolisthesis, but is not the method of first choice as it does not always provide pain relief.

- Facet joint syndrome
- Etiology and pathogenesis
- articular surfaces
- Ligaments and joint capsule
- epidemiology
- etiology
- symptoms
- Treatment
- Treatment
- Complications of osteoarthritis of the lumbosacral spine
- Symptoms of cervical spondylitis
- diagnosis
- Treatment of facet syndrome
- Conservative treatment
- surgical treatment
- prognosis and prevention
- Causes of Spondyloarthritis
- pat anatomy
- ABOUT FACET PAIN SYNDROME
- A little anatomy
- Prices for facetoplasty, radiofrequency denervation
- Symptoms of facet syndrome
- diagnosis
Facet joint syndrome
Facet joint syndrome is a disease associated with degeneration and damage to the facet joints and usually presents as back pain without neurological involvement.
Degenerative changes in the spine can develop after birth, favored by congenital spinal anomalies (lumbarization, sacralization), hypermobility of the spinal segments, and trauma. The incidence of facet syndrome is up to 2 in older people.
Etiology and pathogenesis
The morphological basis of facet syndrome is deforming arthritis (spondyloarthritis). According to most authors, the terms 'spondyloarthritis' and 'facet syndrome' are synonymous. However, some researchers believe that the term 'spondyloarthritis' has a more general meaning because the degenerative process usually affects the facet, the articular capsule of the intervertebral joint, the yellow ligament and other periarticular tissues. The term facet syndrome refers to a more specific clinical symptom that arises from a specific joint.
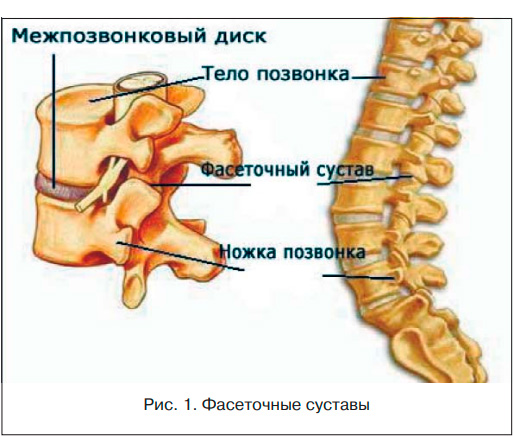
Anatomy of the facet joints. The facet processes (synonyms: arch joints, articular processes) grow from the vertebral lamella and are involved in the formation of the facet joints (Figure 1). Two adjacent vertebrae are connected by two facet joints located on either side of the arch symmetrically to the midline of the body. The articular processes of the neighboring vertebrae point towards each other and are covered at their ends with articular cartilage. The ends of the articular processes are enclosed by a joint capsule. Thanks to the presence of facet joints between the vertebrae, a variety of movements are possible and the spine is a flexible, movable structure [1].
The anatomical structure of the spine emphasizes the task of its front parts (anterior longitudinal ligament, vertebral bodies, intervertebral discs), primarily to resist gravitational forces (compression), and of its rear parts (intervertebral joints, pedicles, transverse and spinous processes, laminae), to resist axial forces To protect against rotational and displacement forces in the anteroposterior and lateral directions. The distribution of gravitational forces in the normal spinal movement section, to which the complex belongs, is as follows: 70 to 88 % fall on the anterior parts and 12 to 30 % on the posterior parts, mainly the intervertebral (facet) joints, although both parts of the spine all forces are exposed. In case of intervertebral disc damage, where the degenerative changes of the spine most often begin, the load of body weight is gradually transferred to the intervertebral joints and reaches 47-70 %. This overloading of the joints leads to further changes: synovitis with accumulation of synovial fluid between the facet surfaces; degeneration of articular cartilage; Stretching of the joint capsule and joint subluxations. Further degeneration from repeated microtrauma, weight bearing, and overload of the rotator cuff leads to periarticular fibrosis and the formation of subperiosteal osteophytes that enlarge the upper and lower facets, which then appear pear-shaped. Eventually the joints degenerate dramatically and lose almost all of the cartilage. This degeneration process is often asymmetrical and manifests itself in uneven stress on the facet joints. The combination of intervertebral disc and facet joint lesions leads to significant restriction of movement in the corresponding movement segment of the spine.
articular surfaces
The facet joint is formed by the articular surface of the superior articular process of the basal vertebra and the articular surface of the inferior articular process of the superior vertebra. The articular surface of the superior articular process of the basal vertebra is flat in the cervical and thoracic spine and convex in the lumbar spine (the articular surface of the inferior articular process of the superior lumbar vertebra is concave and forms an arc with the tip towards the vertebral body).
The facet joints have different orientations depending on the spine:
The articular surfaces of the facet joints of the cervical spine are at an angle of 45 degrees to the horizontal plane, with the articular surfaces of the upper articular processes pointing upwards and backwards and the lower articular processes pointing downwards and forwards.
The articular surfaces of the facet joints between adjacent thoracic vertebrae are at an angle of 60 degrees to the horizontal plane and 20 degrees to the frontal plane, with the articular surfaces of the superior articular processes pointing backwards, upwards and laterally and the inferior articular processes pointing forwards, downwards and medially.
The articular surfaces of the lumbar facet joints lie in the sagittal plane; The articular surfaces of the facet joints are at right angles to the horizontal plane and at a 45 degree angle to the frontal plane. The upper facet surfaces are oriented medially and the lower surfaces are oriented laterally. This changes at the lumbosacral joint, where the articular surfaces lie in the frontal plane, with the lower frontal surface of the L5 vertebra facing forward. This prevents the spine from moving forward in relation to the sacrum.
Ligaments and joint capsule
The posterior ligament complex stabilizes the spine and keeps the facet joints of the adjacent vertebrae in a fixed position relative to one another. It consists of the following structures:
- Posterior longitudinal ligament (ligamentum longitudinale posterior).
- The yellow ribbon.
- Intervertebral ligament.
- Poster oil tape.
- The articular sac of the facet joint. Facet joints, like other synovial joints in the body, are surrounded by a connective tissue capsule that produces synovial fluid to nourish and lubricate them. Each facet joint is innervated by two small nerves, the paired medial branches of the posterior (dorsal) branch of the spinal nerve. These nerves are activated when there is degeneration or inflammation in the facet joint.
epidemiology
Lower back pain is known to occur in 65-80 % of adults.
- FBS is more common in older people because joint changes increase with age.
- Anyone who has done heavy work before the age of 20 increases the likelihood of developing FS osteoarthritis.
- Obesity also contributes significantly to the development of osteoarthritis and is therefore likely a contributing factor to the development of FS.
- Degenerative spondylolisthesis in FS is most commonly caused by osteoarthritis and usually occurs in the L4-L5 segment.
- Spondylolisthesis, which occurs at a younger age (30-40 years), is caused by congenital anomalies, mechanical stress, or acute fractures.
- Cervical FS disease and pain occur in 29-60 % of cases following whiplash, although overall such trauma is a fairly rare cause.
In a study by Eubanks (2007), degenerative FS disease was identified in 647 lumbar vertebrae of cadavers:
- 57 % of samples aged 20-29 years;
- 93 % of people aged 40-49 years;
- 100% of cases had severe FS osteoarthritis at age 60;
- the highest prevalence and severity of the degenerative disease was found in the L4-L5 segment.
etiology
Spinal degeneration, also called spondylosis, is the most common cause of FS damage.
- When joint degeneration occurs due to natural wear and tear and abnormal body mechanics, it is called osteoarthritis. The pathophysiology of osteoarthritis is not yet fully understood, but it is complex and involves various cytokines and proteolytic enzymes as well as individual risk factors.
- Secondary damage, e.g. B. through trauma or sport.
- Secondary inflammatory diseases, e.g. B. rheumatoid arthritis, ankylosing spondylitis (contribute to synovitis).
- Subluxation of the intervertebral joint due to spondylolisthesis may also contribute to the lesion.
People with FS show symptoms of cartilage erosion and inflammation, which can lead to pain. In response to this process, the body also undergoes a number of physical changes.
- Ribbons, such as B. the yellow band, can thicken and hypertrophy.
- New bone formation around the joint may be accompanied by the development of osteophytes or bone spurs.
- An increase in subchondral bone volume with hypomineralization may also occur.
symptoms
- Acute attacks of lumbar and cervical facet joint syndrome occur intermittently and unpredictably and may occur several times a month or year.
- Most patients continue to experience local pain in the area of the inflamed joints and some loss of elasticity in the back muscles (which have a protective function).
- In general, bending backwards causes more discomfort than bending forwards.
- Lower back pain from facet joint syndrome often radiates from the back of the thigh to the buttocks. The pain rarely occurs anterior to the hip and rarely radiates below the knee or into the foot, whereas such pain is common with herniated discs.
- Similarly, in cervical facet syndrome, the pain may be localized and radiate to the shoulders or upper back and very rarely to the front of the arm or hand, which is more typical of herniated discs of the cervical spine.
- The frequency of pain episodes can be quite frequent and quite unpredictable in both duration and intensity. It is not uncommon for patients to believe that the symptoms are psychosomatic and that they can be traced back to 'problems in the head'.
- With lumbar syndrome, mobility is limited when standing, while both pain and muscle tension increase quickly when sitting or driving. Sitting has a paradoxical effect on pain patients.
- At the peak of pain and limitation of movement, muscle contraction becomes so strong that muscle fatigue occurs and the pathological condition becomes cyclical.
In cases where the pain recurs monthly or more frequently, x-rays should first be taken in multiple projections. As a rule, pathological changes in the facet joints can be detected using x-rays. However, with computer tomography, not only the joints but also other structures of the spine can be better visualized.
Treatment
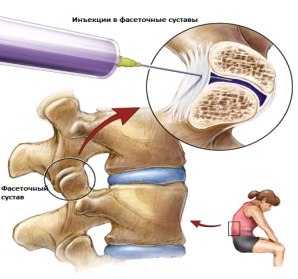
Local administration of anesthetics and corticosteroids. The disappearance of acute or chronic pain during the duration of these medications has both therapeutic and diagnostic value. There are a variety of treatments for acute episodes of facet joint pain, and many of these treatments may provide temporary or long-term relief, but often have no long-term effect. Conservative methods used to treat facet joint syndrome include:
LFC. An exercise program restores abnormal biomechanics, corrects posture, and strengthens muscles and ligaments.
physical therapy Physical therapy can help reduce pain and inflammation in the joints.
Changes in daily life (e.g. reducing long daily commutes) and adequate rest breaks.
Pharmacological treatment Taking anti-inflammatory medications (Ibuprofen, Celebrex).
Manual therapy Manipulation can restore mobility to the facet joints and relieve pain.
The use of orthopedic pillows and a cervical collar is particularly useful when facet joint syndrome is limited to the cervical spine.
A more permanent effect can be achieved by blocking the nerve endings in the facet joints (this procedure is called rhizotomy and is performed with a cooled or heated suppository under X-ray control). Botox injections can also be used, which is good for relieving muscle spasms.
In severe cases, when not only the facet joints but also the intervertebral discs are severely changed, surgical treatment may be necessary. However, in most cases, conservative treatment is able to maintain an acceptable quality of life.
Treatment
Treatment of lumbosacral spondyloarthritis is aimed at both relieving symptoms and stopping the progression of pathological processes in the joints or bones.
Most doctors take a conservative approach in the initial stages of treatment. Only then are invasive options considered, but only if symptoms do not respond to conservative treatment or severe neurological symptoms develop.
The most common treatments for lumbar spondylitis include:

- Physical therapy (PE) is used to strengthen the muscles of the lumbar spine. Stronger muscles provide better support for the spine, reducing stress on the facet joints.
- Reduction in body weight Improves symptoms by simply reducing stress on the lumbar spine. Although weight loss may be difficult for some patients, low-impact exercise (e.g., swimming) combined with a low-calorie diet can often achieve the results needed for pain relief.
- Pharmacological treatment. Anti-inflammatory medications can reduce swelling and inflammation around the facet joints. While over-the-counter medications such as Aleve (naproxen) or Advil (ibuprofen) can often provide sufficient symptom relief, stronger prescription medications such as Voltaren (diclofenac) and Arthrotec (diclofenac/misoprostol) are sometimes necessary.
- The use of cold and heat may also be effective in relieving lumbar pain. Heat can help relax the spine before physical activity, while ice is best used after activity to reduce inflammation.
- Chiropractic treatment. Chiropractic manipulation is often used to treat spinal disorders. Although chiropractic treatment cannot restore the full range of motion of the spinal motion segments and restore the structure of the spine, manipulation can relieve pain and improve mobility.
- Epidural injections (Epidural) include: injecting a steroid (cortisone or similar) into the area of the pinched nerve. Cortisone can influence the immune system and thereby reduce local inflammation and radicular pain.
Complications of osteoarthritis of the lumbosacral spine
Osteoarthritis rarely causes severe neurological dysfunction through compression of nerve structures.
However, over time, degenerative changes can cause spinal stenosis, a narrowing of the spinal canal that can lead to compression of the spinal cord and nerve roots.
Spinal stenosis can be a complication of spondyloarthropathy.
Cauda equina syndrome, a disorder caused by compression of the nerves in the lower part of the spinal cord by overgrowth of tissue or a disc, is a relatively rare complication of osteoarthritis that can lead to serious neurological problems.
Symptoms of cervical spondylitis
The main symptoms of the disease in the initial stages are pain and discomfort in the neck. The pain is usually excruciating and persistent and increases with movement. The pain may worsen and sometimes be sharp if you remain in an uncomfortable position for a long time or if you exert yourself for a single time. Patients often experience neck stiffness in the morning, which usually subsides within 30-40 minutes. Radiation of the shoulder and arm is rare, and there are no neurological abnormalities.
As cervical spondyloarthritis progresses and osteochondrosis becomes more severe, the symptoms become more pronounced and varied. The pain increases in spurts and begins to radiate into the shoulders and upper back. Dizziness, headaches, a feeling of fog and heaviness in the head may occur. Paresthesia and numbness in parts of the body as well as sensory disturbances may occur. Damage to the joints of vertebrae I-II (uncovertebral spondyloarthritis) can be accompanied by balance disorders, inflammation of the cervical and shoulder nerves, and hyporeflexia.
diagnosis
Diagnosis and treatment of cervical spondyloarthritis is carried out by orthopedists, neurologists and vertebrologists. The following imaging tests are recommended to confirm the diagnosis:
- X-ray. It is carried out in two main and additional projections. It is meaningful when there are obvious joint changes. The images of the cervical spine show deformations of the joint surface, osteophytes and joint narrowing.
- Computed Tomography. It is more sensitive and can diagnose spondyloarthropathy at an early stage. It shows changes in the hard structures – bones and cartilage – well.
- Magnetic resonance imaging (MRI). Used when the condition of the surrounding soft tissues needs to be assessed. Atrophy, fibrotic changes and signs of inflammation can be recognized.
- The ultrasound examination.. Doppler ultrasound (USG) of the head and neck is recommended to assess cerebral blood flow and rule out vertebral artery syndrome.
The neurological examination reveals accompanying sensory and movement disorders. If indicated, an advanced neurological examination using instrumental techniques is performed.
Treatment of facet syndrome
Conservative treatment
In acute cases, the main goal is to treat the pain as quickly as possible. First-line drugs are selective nonsteroidal anti-inflammatory drugs (NSAIDs), which act primarily on COX-2 and have fewer side effects. Patients with facet syndrome require long courses of NSAIDs, which may be combined with gastric protection.
In addition to analgesic treatment, muscle relaxants are used to relax the tension of the spinal muscles and break the vicious circle of pain-muscle-spasm-pain. Pharmacotherapy is enriched with chondroprotective agents to slow the progression of joint changes. If pain is severe, local anesthetics and glucocorticosteroids are indicated to quickly relieve symptoms and allow normal movement.
Physiotherapy techniques play an important role in pain relief and patient rehabilitation. Phonophoresis, ionogalvanization and magnetic therapy have a good pain-relieving effect. Once the pain has subsided, they prescribe physiotherapy, therapeutic massage and manual therapy. Cognitive behavioral therapy can be used to learn how to deal with unpleasant facet syndrome.
surgical treatment
If conservative treatment fails or complications of facet syndrome occur, neurosurgical help is required. The most commonly used method is minimally invasive - the destruction of the spinal root branches supplying the facet joints with radiofrequency current. This method does not require anesthesia, no skin incisions and no rehabilitation period. Radiofrequency current denervation has an 80 % success rate in eliminating pain and lasts more than 12 months.
prognosis and prevention
Phasic syndrome is characterized by a recurrent course, with each subsequent episode being more severe than the previous one. It does not pose an immediate threat to health, but underlies a more serious spinal disease and affects the patient's quality of life, so the prognosis is questionable. The following measures are recommended for prevention: correct sitting and standing posture, back and neck exercises, regular swimming courses.
1. Lumbar facet syndrome in elderly patients: diagnosis and treatment / TL Visilo et al. – 2016. – №5.
2. The problem of chronic back pain: facet syndrome / NN Spirin, DV Kiselev // RMJ. Medical Review. – 2015. – №23.
4 facet syndrome. Issues of therapy and prevention / OV Vorobyova / RMJ. Rheumatology. – 2013. – №32.
Causes of Spondyloarthritis
This pathology is caused by degenerative-dystrophic changes in the spine, which occur both as a result of natural aging processes and as a result of various negative factors. The decisive factor for spondyloarthrosis is the constant functional overload of the facet joints due to excess weight, increased physical stress and the disruption of the relationships between the various anatomical elements of the spine.
Early-onset spondyloarthritis is often observed in association with developmental abnormalities such as sacral spine junction (lumbralization and sacralization). During lumbralization, an additional VI enlarges. The lumbar vertebra provides the 'lever arm' for the lumbar spine, which leads to increased stress on the lumbosacral junction. With unilateral sacralization, the load on the spine is unevenly distributed, which leads to the development of spondyloarthropathy on the opposite side.
In addition, congenital malformations of the spine, such as: B. articular tropism (asymmetry of paired facet joints), vertebral arch formation, and fusion of vertebral arches and vertebral bodies, causing early development of spondyloarthropathy. It is worth noting that small spinal anomalies are common and are found in about half of the world's population.
Injuries that increase the likelihood of developing spondyloarthritis include both severe trauma (vertebral compression fractures), after which the anatomical relationships between the various spinal structures may change, and mild trauma (traumatic facet joint subluxations). The latter often occur in untrained people over 30 years of age during a single, strenuous physical activity. This can e.g. This can happen, for example, from lifting heavy weights when moving house or while working in the country, but also from occasional exercise on holiday or when trying to 'get in shape'.
pat anatomy
The statics of the spine are such that in most cases the lower lumbar spine and the upper sacrum are the most overloaded. Therefore, osteochondrosis, spondylarthrosis, spondylolisthesis and other pathologies of the spine are often detected simultaneously at this level. Osteoarthritis of arthritic joints most commonly occurs in the section between the fifth lumbar vertebra and the first sacral vertebra. The section between the fourth and fifth lumbar vertebrae is less commonly affected.
The main symptom of the disease is pain that occurs with movement, flexion and rotation of the body and subsides or subsides with rest. Unlike a herniated disc or osteochondrosis, the pain syndrome in spondyloarthritis is often localized and is not accompanied by radiation to the limbs, weakness or numbness in the arm or leg. After progression of spondyloarthritis, morning stiffness occurs, which bothers the patient 20 minutes to 1 hour after the start of movement.
Facet joint subluxation in spondyloarthritis causes localized, dull pain and discomfort in the affected area. These symptoms worsen with prolonged standing in one position, so patients try to change positions frequently. Subluxations can be restored to the correct position alone or with chiropractic care, and the joint surfaces often snap back into place. In the later stages of spondyloarthritis, excessive osteophytes form in the affected area, which press on the nerve roots and narrow the spinal canal. In such cases, sciatica symptoms appear that are atypical for spondyloarthritis - radiating pain, accompanied by weakness and numbness in the limbs.
When examining patients with spondyloarthritis, some stiffness and limitation of movement in the affected area are noted. With deep palpation, pain is detected in the projections of the small joints of the spine. In some cases, pain and tension occur in the extraspinal and paravertebral muscles. These symptoms are particularly pronounced in exacerbations of spondyloarthritis.
ABOUT FACET PAIN SYNDROME
A little anatomy
The vertebrae consist of vertebral bodies and vertebral arches. The vertebral bodies are connected to each other by intervertebral discs and the joints by facet joints.
The facet joint – is the point where the articular processes of the vertebrae come together. Like all joints, the bones that make up the joint are covered in cartilage, and the joint itself is surrounded by a small synovial sac that contains synovial fluid. These joints protect the intervertebral discs from excessive stretching during flexion and rotation of the body, in which the spine is involved.
The information on this site should not be used for self-medication or self-diagnosis. Diagnostic examinations for acute illnesses should only be carried out by a doctor! In order to make a correct diagnosis and prescribe treatment, you should consult your doctor.
Prices for facetoplasty, radiofrequency denervation
Please note that prices on the website may vary.
Please call the administrators to find out the actual costs.

NikolaevAnton Valerievich traumatologist and orthopedist
Has been practicing for patients for 15 years. Experience as a doctor: 17 years.
Cost of admission: 4000 ₽
MAKE AN APPOINTMENT

SidorkinDmitry Nikolaevich traumatologist and orthopedist
Has been accepting patients for 10 years Category 1 doctor, MD, PhD Experience: 12 years
Cost of admission: 4000 ₽
MAKE AN APPOINTMENT

ChelnokowaNatalia Valeryevna traumatologist and orthopedist
Doctor of Medicine/PhD degree (13 years) Medical experience: 20 years.
Cost of the visit: 6000 ₽
MAKE AN APPOINTMENT
ZirenkoEvgeniy Aleksandrovich traumatologist and orthopedist
Has been accepting patients for 14 years. Doctor with the highest qualification category. Doctor's experience: 31 years.
Cost of admission: 4000 ₽
MAKE AN APPOINTMENT

Symptoms of facet syndrome
The most typical symptom of facet syndrome is a monotonous, dull pain. They are localized, penetrant or bilateral. They occur during any physical activity, during various movements, when bending and turning the body or when standing in one position for a long time. Some patients experience pain attacks that mimic sciatic pain. In most cases, the pain is more intense in the morning after getting up and in the evening after exercise.
Initially, the symptoms of facet syndrome occur in the lumbar spine, but also in other parts of the spine, once or twice a year. With each recurrence, the pain episodes become longer. If the source of the pain is in the neck area, the pain can radiate to the back of the head, shoulders and shoulder blades. If the lumbar region is affected, the pain can radiate to the groin, hips, thighs and buttocks. This disease is to be distinguished from piriformis muscle syndrome.
diagnosis
The diagnosis of facet joint syndrome is made on the basis of a neuroorthopedic and instrumental examination. This includes:
MRI is considered the safest and most conclusive method for diagnosing facetalgia. The precise, non-invasive technique makes it possible to accurately detect hypertrophic changes in the intervertebral joints and determine their severity without the use of other techniques.
Spinal rehabilitation: Input from the specialists of the 'Movement Laboratory' rehabilitation center.
Download a detailed rehabilitation program
Read more:- articular process.
- Which doctor do you go to if you have joint problems?.
- sphenoid.
- back foot.
- The lateral dislocation is.
- The long fibula muscle hurts.
- X-ray foot subluxation.
- Diagram of a joint with and without a dislocation.
