The Lauterge operation involves the anterior stabilization of the joint using a displaced scapular process on a tendon stalk of a corpse.

- Osteoarthritis of small joints: how to get rid of pain in the hands and feet
- species
- Osteoarthritis in the hands and fingers
- Osteoarthritis in the ankles
- When should you agree to surgery?
- When surgery is contraindicated
- Types of injuries to the shoulder structures
- diagnosis of the injury
- Indications and symptoms of Chopard arthrodesis
- Arthrodesis of the Chopar joint - where and where in St. Petersburg?
- Congenital spondyloepiphyseal dysplasia, congenital spondyloepiphyseal dysplasia
- Treatment
- The valgus foot in Ehlers-Danlos syndrome
- Treatment
- Material and methods.
- Conclusions
- RS85 ultrasound machine
- Examples
- Features of muscle structure and function
- Common shoulder dislocation
- Latarger operation
- Treatment in the Health Energy Clinic
- Benefits of the clinic
Osteoarthritis of small joints: how to get rid of pain in the hands and feet
Osteoarthritis of the small joints is a disease in which the cartilage between the joints is destroyed. The disease can affect the joints of the hands, fingers and feet. Osteoarthritis of small joints is less common than disease of large joints. The disease occurs more frequently in older people.
Osteoarthritis begins with impaired blood circulation in the subchondral layer of the periosteum. As a result, the nutrition of the cartilage is impaired, it loses elasticity, becomes thinner and cracks appear. The amount of synovial fluid decreases and the friction causes arthritis to develop.
Progressive osteoarthritis is very dangerous. If arthritis of the hand or foot is not treated in a timely manner, the joints take on an unnatural, ugly shape and may lose mobility.
This disease often occurs in women during menopause. Women's hormones change and they produce less estrogen. This causes the body to lose a lot of moisture, causing cartilage and joints to become more brittle.
species
There are two types of osteoarthritis, depending on the location:
Osteoarthritis in the hands and fingers
Osteoarthritis of the hands is common among typists, pianists, computer programmers, and secretaries. The disease affects the interphalangeal joints. With osteoarthritis of the fingers, the joint tissue dries out and tears. Small nodules often form under the skin in the joints of the hands. These usually do not disappear again.
As the disease progresses, the bone tissue thickens and hypertrophy occurs. They cause severe pain when moving the fingers. In advanced cases, the affected person loses the ability to move the hand and fingers.
Symptoms of the disease include a crunch in the joints when moving the fingers, pain in the fingers during exertion, thickening of the finger joints, and swelling of the periarticular tissue.
The doctors in the health studio treat hand osteoarthritis using non-surgical methods.
Osteoarthritis in the ankles
Ballerinas, dancers, gymnasts, wrestlers and divers are susceptible to osteoarthritis in the foot. The disease affects the joints of the toes. Bony growths form on the small joints of the foot. These make moving the foot painful for those affected. As the disease progresses, the deformation of the joints becomes clearly visible and the affected person can hardly move their foot.
Osteoarthritis of the big toe is the most common form of foot osteoarthritis. This causes a 'ball' to form in the joint area of the big toe. Osteoarthritis of the big toe is caused by wearing tight shoes.
Symptoms of osteoarthritis of the foot: pain in the foot when exerting weight, crunching of the joints when moving, enlargement of the joints. The affected person limps and leans on the outer edge of the foot.
To treat foot osteoarthritis, the doctors at the health workshop use, among other things, laser therapy and magnetic therapy.
When should you agree to surgery?
If pathological changes develop in the cartilage, ligaments or meniscus, there is a gradual loss of function of the joint - the patient suffers from pain, swelling and inflammation. In many cases, the condition is made even worse by poor blood flow to the joint. As a result, the cartilage is destroyed, its surface becomes thinner and deforms.

In the early stages, the joint can be treated with conventional medications, physical therapy, and exercise. If the patient falls into a bad condition, the only solution is surgical treatment.
Important!!!
Arthrodesis should only be performed if the patient cannot receive an artificial prosthesis due to weakening of the bone or rejection of the implant by the body.
- Significant joint instability – with the progression of certain pathological diseases, the joint space decreases. The ligaments do not shorten, the attachment of the bones of the limb decreases. This leads to abnormal dislocations and subluxations that require surgery;
- Osteoarthritis - in the initial stages, its progression can be slowed down by medications and general corrective treatments, but if the patient does not follow the doctor's advice, over time the disease leads to irreversible changes in the joint, requiring surgery;
- Osteoarthritis is a rapidly progressive disease that is often difficult to treat. Arthrodesis is indicated when there are mobility problems and severe deformities of the leg;
- Osteoarthritis – damage and wear of the cartilage deforms the joint, requiring surgical treatment;
- Joint disorders in periarticular fractures - if the bone has healed so much that the joint is not mobile, arthrodesis is required;
- Developmental anomalies – in some congenital anomalies, the joints do not function properly and subluxation of the joints may occur. In these cases, surgery is indicated;
- Other causes – serious complications of certain diseases, which lead to irreversible damage to the connective tissue and thus to joint deformation and restricted movement up to ankylosis.
When surgery is contraindicated
Despite the simplicity of the procedure, there are several contraindications to this type of operation:
- Age criteria – children under 12 years old and elderly people over 60 years old. In a child, the bone component has not yet fully matured - artificial ankylosis cannot form. In old age, bone regeneration is poor - the postoperative area cannot withstand daily stress;
- There are infections, abscesses or fistulas - arthrodesis requires a high level of bone regeneration, which is severely limited in these conditions;
- The unstable and severe condition of the patient – rehabilitation will be lengthy and there is a greater risk of side effects.
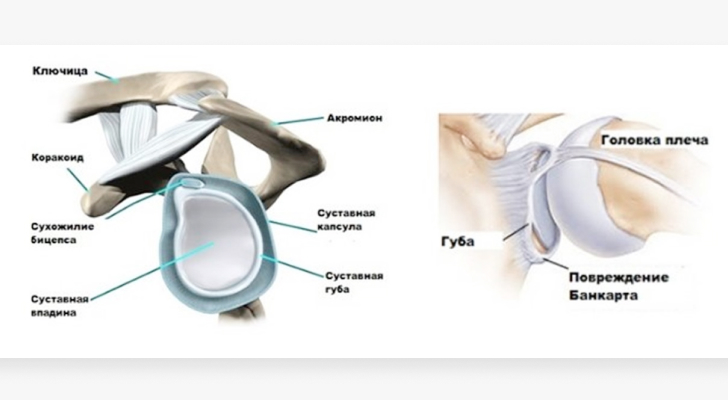
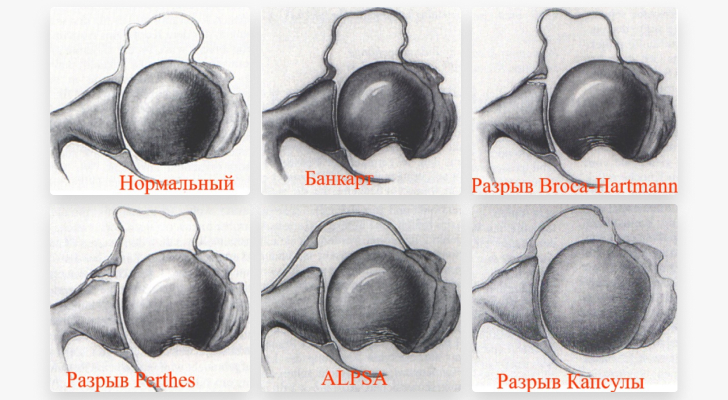
Types of injuries to the shoulder structures
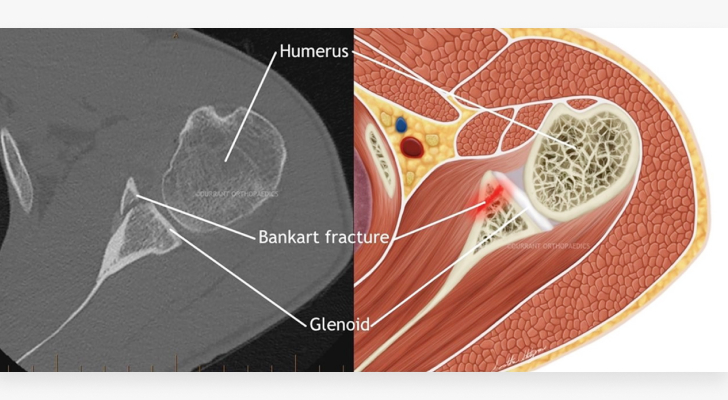
Bankart fracture – classic tear of the anterior lip of the lower articular cartilage of the shoulder joint socket.
Bankart fracture – displaced anterolateral fragment of the articular process of the scapula.
Injuries to the articular labrum along with the joint capsule and ligaments at various levels and in various modifications are soft tissue injuries of the shoulder joint.
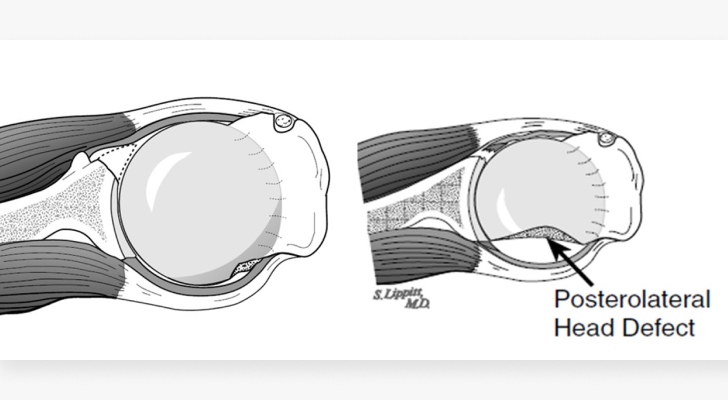
In 80 to 100 % cases it is a Hill-Sachs fracture, a fracture of the posterior tip of the humeral head.
diagnosis of the injury
At the first consultation, the doctor takes a detailed anamnesis: he states under what circumstances the primary shoulder dislocation occurred - with or without trauma, who caused it and where (in the trauma center or at the site of the dislocation), whether and for how long Extremity was immobilized.
In addition, an examination of the injured joint should be ordered and tests performed to check for instability. X-rays, MRIs and, in some cases, CT scans can be used to objectively assess the shoulder joint injury.
In the final consultation, the trauma surgeon will discuss the pathology and discuss the surgical treatment options indicated for this pathology.
Indications and symptoms of Chopard arthrodesis
The main indication for surgical intervention is paralysis of the foot, dislocations and fractures of the schopar joint. If the articular surfaces are severely injured, it may be necessary to perform a primary arthrodesis immediately after the dislocation.
If the sprain is sprained or broken, the shape of the foot is significantly disrupted. Swelling and severe pain occur, making it difficult to walk on the foot. The edge of the navicular bone can be felt on the inside and back of the foot. Blood circulation in the affected area of the foot is severely impaired.
Arthrodesis of the Chopar joint - where and where in St. Petersburg?
Injuries of this type require a good emergency reduction. In this situation, the main focus is to correct the dislocation, followed by treatment of fractures of other bones.
During this procedure, one assistant holds the lower third of the shin, a second holds the heel, and a third holds the forefoot and pulls firmly. The surgeon at Andro Meda Clinic applies firm pressure to the inside of the foot with the first toe, while the other hand applies pressure in the opposite direction to the inside of the heel. The surgeon then moves one hand to the back of the foot and the other to the sole area and applies firm pressure towards the sole.
After pushing the foot backwards, a plaster cast is placed around the knee joint. The foot must be positioned at a right angle; It is particularly important to model the arch of the foot precisely. The limb is placed in a splint and blood flow to the joint is monitored.
If this is not possible, surgical intervention is necessary. The surgical procedure is performed under anesthesia or general anesthesia on the healthy side of the foot. A specialist surgeon will make an incision on the outside of the foot and further back on the foot.
Congenital spondyloepiphyseal dysplasia, congenital spondyloepiphyseal dysplasia
Congenital spondyloepiphyseal dysplasia involves severe and stiff clubfoot and severe congenital bone deformities that progress rapidly with age. Changes to the metaphyses of the short bones of the foot are characteristic. In general, however, the distal skeleton is less affected than the proximal skeleton. In some forms (pseudo-Morchio syndrome) there is a very strong shortening of the metatarsal bones and toe phalanges, and the feet are square.
Treatment
Conservative treatment of gross bony foot deformities is not very effective. Surgical treatment consists of a combination of THA, Ilizarov device, simulated bone resection, and tibialis anterior muscle grafts. It is advisable to stabilize the result by creating artificial ligaments, and in case of talar deformity, astragalectomy is indicated. Milder, functionally insignificant foot deformities do not require surgical correction.
The valgus foot in Ehlers-Danlos syndrome
A characteristic feature is the combination of rigid deformities in some joints with hypermobility in others. When multiple joints are affected, clubfoot is similar to clubfoot arthrogryposis.
Treatment
Plaster casts should be applied from the first weeks of life. However, there is a high risk of developing secondary clubfoot, which can develop without treatment due to static loading if the deformity is not corrected. Therefore, a Ponseti cast with surgical correction of the equinus component is indicated. At the first signs of secondary deformity, conservative therapy must be stopped and surgical treatment performed. In cases of severe hypermobility, tendon lengthening is approached in moderation, capsulotomy is sometimes avoided, and postoperative immobilization is carried out strictly in the metatarsal position. Due to the incomplete connective tissue, the risk of postoperative neuropathy and postoperative hematomas is increased.
Material and methods.
Ultrasound examination of the hip joints was carried out in 395 children up to 6 months of age according to the method of G. Reingard [3] with simultaneous assessment of the development of the osteochondral relationship of the joints and determination of the sonographic types of the hip joints.
During the hip examination, the following hip joint types were distinguished in 395 children.
During the ultrasound examination of 286 (72,41%) children, hip types 1a and 1b (according to G. Reingard) were determined. Clinically and sonographically, types 1a and 1b correspond to the age of the child - these are healthy joints. The bony part of the acetabulum is well defined, the bony arch is slightly flattened or rectangular, the cartilaginous part of the roof encloses the femoral head, and the bone to cartilage ratio is greater than or equal to 2/3. The angle α is greater than or equal to 60°. A β angle less than 55° is type 1a (Figure 1); a β angle greater than 55° is type 1b.

Illustration 1. Hip joint type 1a.
1 – angle α=70.9°;
2 – Angle β=51.2°.
Thirty-five (4.81 %) children had simple bilateral hip dysplasia without spatial abnormalities (Figure 2). This pathology leads to delayed ossification (nucleus pulposus formation), which is accompanied by a reduced calcium content in the child (as a result, with increasing physical stress on the joints, when the child begins to sit and stand after the sixth month of life, a deformation of the femoral head can occur).

Figure 2. Simple dysplasia – delayed ossification without spatial abnormalities (child 5 months).
Type 2a hip arthroplasty (Figure 3) was diagnosed in 46 (11.6 %) children. This is a variant of physiological delayed hip development in children under 12 weeks in which the α angle is less than 59° but greater than 50° or the β angle is greater than 60°.
Conclusions
The present study confirms the need for outpatient hip ultrasound examinations in children younger than 6 months to avoid unnecessary radiation exposure. The use of the information obtained allows early corrective therapy for all types of hip joints, followed by correct training.
- McNally J. Musculoskeletal ultrasound: a practical guide. Vidar-M Publishing. 2007. 400 с.
- Sinelnikov RD, Sinelnikov YR Atlas of Human Anatomy. Second edition, stereotype. In 4 volumes. T. 1. Moscow: Medycyna, 1996. 344 с.
- Reingard G. Sonography of the neonatal hip. Diagnostic and therapeutic aspects: a guide. 5th edition // Sonographic types of the hip joints / Tom University Press. 2005. 196 с.

RS85 ultrasound machine
A revolutionary change in specialty diagnostics. Impeccable image quality, lightning-fast speed, next-generation imaging technology and quantitative analysis of ultrasound images.
Examples
1. Unicompartmental musclesThe hamstring muscles include the lateral femoral latissimus, medial latissimus femoris, and medial latissimus femoris. These muscles lengthen the lower leg. Crossed Crosses the knee joint. Attaches to the femur and shinbone.
2. Two-jointed muscle.Rectus femoris muscle: M. rectus femoris. Exercises flexion of the thigh and extension of the lower limbs. Crosses two joints: hips and knees. It attaches to the hip bone (pelvis) and the shinbone (tibia).
3. Unicompartmental musclesBrachialis, Brachioradialis, Pronator circularis. You perform the flexion of the forearm. Cross elbow joint.
4. Biceps muscle (bicuspid tendon)The long head of the biceps brachii muscle. Flexes the shoulder and flexes the forearm. It crosses two joints. Shoulder and elbow.
5. Multi-joint muscles.Radial flexor of the wrist, superficial flexor of the fingers, deep flexor of the fingers. Exercise: flexion of the hand and fingers. Crossing the elbow joint, wrist and finger joints.
Features of muscle structure and function
1) A muscle can have both one- and two-joint muscles. The quadriceps of the thigh, for example, consists of three unilateral muscles (lateral thigh muscle, medial thigh muscle, and middle thigh muscle) and one bipartite muscle (rectus femoris). The triceps femoris muscle is composed of two two-joint muscles (lateral head and medial head of the calf muscle) and a single-joint muscle, the hamstring muscle. The muscles that allow the toes to move are multi-jointed.
2. The single-joint muscles serve to control the joint angle, as only single-joint muscles can set a specific angle between the joints. The two-jointed muscles, because they 'cross' two joints, cannot give a specific value for the joint angle at a particular joint. However, they perform a number of other functions in human movement.
3. VM Zatsiorski, AS Aruin and VN Seluyanov, (1981) point out that:
- All two-jointed muscles produce opposite moments of force at the joints through which they pass (e.g. flexion of the knee joint and extension of the hip joint). Therefore, during natural movements such as walking and running, these muscles are active during the phases of movement that require such multidirectional forces.
- When two adjacent joints are simultaneously flexed or extended, the length of the biceps muscles changes very little (6-8 % of the original length). Therefore, these muscles can be considered to work in a near isometric mode.
- Bicompartmental muscle activity reduces the mechanical work associated with movement and thus reduces energy expenditure. In this way, the mechanical energy can be transferred from one link to the other.
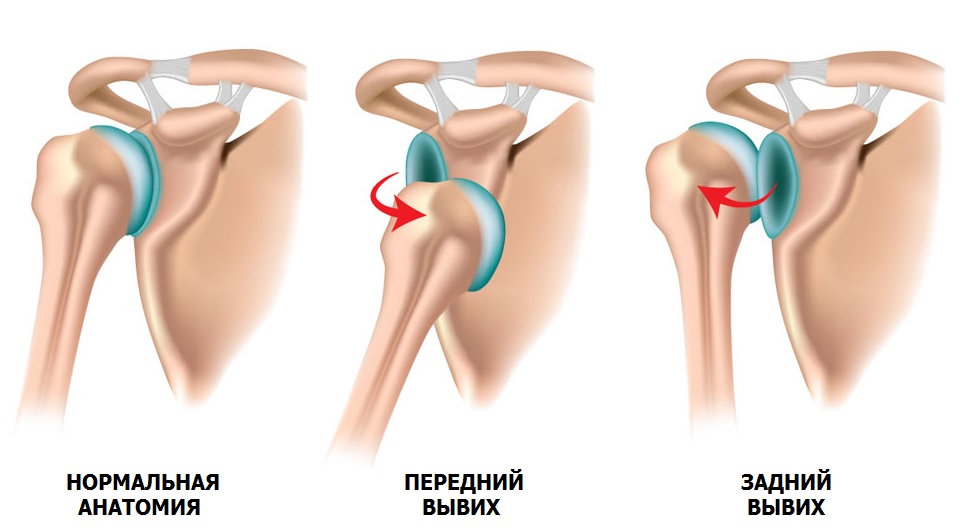
Common shoulder dislocation
It is a misconception that a dislocation is better than a fracture. The consequences of a primary dislocation can be very serious and can lead to recurrence of the injury.
Dislocation is a pathological condition in which the head of the humerus shifts relative to the socket of the scapula (instability of the shoulder joint). In 90 % cases the cause of the dislocation is trauma, e.g. B. a fall with an outstretched arm, a blow to the shoulder joint, lifting heavy objects, excessive movement of the arm and a muscle spasm due to epilepsy.
A predisposition to dislocation is dysplasia, a congenital connective tissue disorder in which the joints are very mobile (hypermobility).
When a sprain occurs, the head of the humerus moves violently, as if it were being pulled out of the joint. The result is damage to the supporting elements: the labrum and the ligaments of the fibula. As the number of dislocations increases, the dislocation occurs with less resistance. The soft tissue structures do not provide adequate support for the joint, and gradually the interacting bones begin to fail, causing erosion. Instability of the shoulder joint progresses over time and dislocations can occur even during sleep.
Surgical treatment is considered the main method of restoring stability to the shoulder joint. Arthroscopy (Bankart operation) is the most gentle method. If the bone is intact and the labrum fibularis is of good quality, the labrum fibularis is refixated with special anchored resorbable implants. The entire operation is carried out using 3-4 skin punctures of 5-6 mm each. Through the first puncture, a camera is inserted into the joint cavity, the image of which is transmitted to a monitor. The joint is viewed from the inside and the fiber lip is torn. Through the remaining punctures, it is mobilized using special mini-instruments and the surface of the scapula is freed from scar tissue. Channels are drilled into the shoulder blade into which anchors are inserted and anchored into the bone. The sutures of these implants are sewn through the fibrous lip and pulled onto the scraped surface of the scapula. By stabilizing the soft tissue structures, the anatomy lost due to the dislocation is restored. The fibrous lip needs time to take root, so the shoulder is placed in a soft support bandage for 4 weeks after the operation.
Latarger operation
If the shoulder joint becomes unstable due to a bony deficit in the scapula, relocation of the scapular process (Latargé operation) is recommended.

The operation is also used for weak shoulder joint ligaments, recurrent dislocation after Bankart operation and missing fibular labrum. During the operation, a piece of the articular process (2×1 cm) is cut out. With the muscles attached to it, it is transferred through the scapular muscle to the anterior surface of the scapular socket (glenoid). After preparation and correct positioning, it is fixed with 2 screws.
The operation repairs the bony defect in the glenoid by relocating the cranial process and provides a supportive effect by moving the muscles closer to the head of the humerus.
Recovery and return to previous work is possible as early as 3 months after the operation.
Treatment in the Health Energy Clinic
The podiatrists at the Health Energy Clinic offer patients comprehensive treatment for shoulder osteoarthritis:
- Modern drug therapy regimens that combine high effectiveness with minimal side effects;
- Proven and new physiotherapy techniques;
- PRP therapy;
- Therapeutic exercises and massages to eliminate restricted movement in the joint.
If necessary, therapeutic punctures of the joint are performed with the administration of anesthetics or artificial synovial fluid to facilitate movement.
We monitor the patient throughout the treatment period to keep the disease under control.
Benefits of the clinic
The Energy Health Clinic offers its patients.
- Comprehensive health monitoring programs;
- Comprehensive medical examinations allowing an accurate diagnosis;
- Consultations with specialists from various fields;
- a modern treatment program that includes not only medication, but also physiotherapy, massage and physical therapy;
- affordable prices for all services.
Osteoarthritis in the shoulder is a problem that can completely change a person's life. Do not allow the disease to reach an irreversible stage, come to Energy Health and seek advice from an orthopedist.
Read more:- Arthrodesis of the subtalar joint.
- Schopar and Lisfranca joints are.
- pelvic thigh joint.
- Shapar joint.
- Lisfranc joint.
- tearing of the joint capsule.
- The key to a chopper joint is.
- Schopar'sche joint.
