The players stand in a circle. The leader in the middle throws the ball in the air and calls out a player's name. The named player has the task of catching the ball. If the ball is not caught, the player switches places with the leader. The player who least expected to be the leader wins.

- Gait disorders in children: causes and symptoms
- Causes of gait disorders
- Development of arms and legs
- other skills
- See
- The hearing
- Speak
- social behaviour
- How do you tell if a child has a gait disorder?
- Osteopathy – a painless method of treating gait disorders in children
- Double hemiplegia
- Hyperkinetic form
- Massage therapy
- Therapeutic gymnastics
- Gait changes associated with brain pathology
- When will your child be able to walk: what do the experts say?
- When is a delay a sign of problems?
- Why does cerebral palsy affect mobility?
- Mobility problems depending on the type of cerebral palsy
- Causes of dyspraxia
- Treatment of dyspraxia
Gait disorders in children: causes and symptoms
Walking is a familiar but difficult process. When a person takes one step after another, all the muscles in his body work together, and the central nervous system and brain coordinate the movement. Several factors are responsible for efficient gait:
- Correct anatomical structure of both legs.
- Absence of muscle dysfunction.
- Correct mobility of the joints.
- Good neuromuscular coordination between the brain and the musculoskeletal system.
- Absence of abnormalities in the middle ear, which is responsible for coordination.
If at least one factor is abnormal, gait is impaired to some extent.
Causes of gait disorders
If a child has difficulty walking, it may be an indication that something is wrong with the CNS or brain. However, the causes of gait disorders are not always associated with abnormalities of the internal organs. There are a number of factors that have nothing to do with brain activity or the functioning of the CNS (here gait disorders occur because the child simply feels pain when walking):
- Previous trauma. If the child has suffered a fracture, sprain or sprain, it may cause pain for some time while walking.
- Existing injuries.
- An ingrown toenail.
- Calluses, spurs or warts on the foot.
- Long walking times.
- Uncomfortable shoes.
Finally, orthopedic problems such as club feet or flat feet are also causes of gait deviations.
Development of arms and legs
At this stage the child is able to hold two objects in one hand at the same time, e.g. B. two dice. He learns to pull the toys together using the string.
One of the most common games from the 10th month onwards are throwing games. When baby is big enough, he or she will enjoy dropping toys and watching them fly away and disappear from sight. And the unconditional joy that the child feels when he picks up the toy, it is returned to him and he starts playing again until he gets bored. However, the child cannot yet consciously let go of the toy and must be supported, for example by gently knocking it out of his hand.
By the age of 10 months, a baby often develops what is known as a pincer grip:
This additional way of grasping objects is derived from the pincer grip and allows the child to grasp small objects even more precisely. In the pincer grip, the tip of the thumb meets the tip of the index finger - nail to nail. With this grip it should be possible to stretch the thumb wide and turn it towards the index finger. The joints of both fingers are slightly curved and look like pincers when gripped. This form of grasping is the most complex or diverse grasping function that a child can master in the first year of life. Even adults cannot always perform the pincer grip correctly because it requires the thoracic spine to be completely straightened. The more bent a person is and the rounder the thoracic spine is, the more limited shoulder mobility is.
With this method, the child can pick up, examine and put increasingly small pieces of bread, oatmeal or peas into their mouth as they eat. When perceiving, the child now learns to use only the index finger, for example when turning the wheels of a toy car.
other skills
See
From this stage onwards, nothing remains hidden from the child: he can now see clearly at greater distances.
The hearing
The child begins to perceive sounds that are outside of his field of vision. When a car passes by on the road, it listens carefully and may soon stop.
Speak
The child's linguistic imitation becomes more and more accurate: the child tries to repeat the first spontaneous words. The first word is often 'mom' or 'dad'. Animals are referred to by the sounds the animal makes, e.g. E.g. a dog of this age is called 'woof woof'.
social behaviour
The child begins to recognize his toys, that is, he can distinguish his own from those of others. It laughs at its reflection, examines it and touches the mirror, but does not yet recognize or identify itself. However, it now responds to its name.
Don't forget that the child is now beginning to check the parents' inhibitions: how consistent or inconsistent the adults are in their behavior; what really shouldn't be done and where mom and dad and other adults can show weakness. They are aware of when and with whom they want to cuddle.
In addition, children at this stage often try to imitate the actions of others, e.g. E.g. drinking from a cup or eating with a spoon.
How do you tell if a child has a gait disorder?
To determine normal gait, three conditions must be met:
It's possible to recognize at a young age that a child is beginning to walk abnormally - and to see a doctor for a diagnosis at that time. As always with treatment, the sooner you see a specialist, the more effective the treatment will be.
Symptoms of abnormal gait
1 Walking on tiptoes: A child who previously walked safely up and down on a surface suddenly only walks on tiptoes. It is important to ensure that this gait is consistent and that the child strikes with the whole foot when jogging or climbing stairs.
2. Shaky, unsteady gait: The child tries to spread his legs further when walking so as not to fall over. Restlessness when the child should already be walking safely. Some instability is normal in the first few months of independent walking.
3. Asymmetrical gait: The child leans more on one foot, or puts one foot forward and pulls the other up, or turns the foot up, or puts one foot up. Only do not be alarmed if the child is just learning to walk and walks with a treadmill on his foot - this is normal.
4 Zezen, turning the feet inwards. In principle, this may be a normal variant in infants, but it is better to consult a doctor.
5 Old man's shuffling gait: a shortened step in which the child appears to drag his feet behind him.
6. 'Stair walk': The child bends their knees slightly as if they were climbing stairs, even if they are walking straight.
7. the 'duck walk': The child walks from one side to the other.
At a tender age, you should pay attention to everything: sudden changes in gait, inability to walk from 1.5 years old (provided that the child has been walking independently since the age of one or earlier), inability to climb stairs from 2 years old, jumping off 2.5 years, inability to walk on tiptoes or stand on heels. Although seemingly insignificant, every detail can indicate the onset of serious impairment.
Osteopathy – a painless method of treating gait disorders in children
Osteopathy treats gait disorders comprehensively, taking into account the balance of all body systems, including those mentioned above. An osteopath may be hired to balance the ankles (foot - shin - hip - pelvis) and correct birth injuries, which are often the cause of gait disorders. Early correction prevents or reduces the risk of skeletal deformities as we grow up.
We recommend consulting an osteopath if your child exhibits the above-mentioned gait abnormalities after the age of 1.5 years.

Osteopathic doctor, orthopedic surgeon. Specialized in: Musculoskeletal problems in children, headaches, neuroses in children, treatment of stuttering.
Double hemiplegia
The most severe and rare form of the disease, causing profound damage to the musculoskeletal system and significant mental impairment. Children diagnosed with this form of cerebral palsy cannot sit, walk, care for themselves, and have no ability to speak or understand.
Children diagnosed with this form of cerebral palsy are capable of primitive emotional reactions, such as: B. recognizing and feeling joy with their parents, but are unable to master even simple skills and cannot learn. The aim of treatment is to improve the patient's overall condition and maximize their quality of life.

Hyperkinetic form
Risk factors for the hyperkinetic form of cerebral palsy include hemolytic disease with jaundice, premature birth, infectious diseases in the mother and low birth weight of the child.
The symptoms of this form of cerebral palsy are manifested in delayed motor development. The child is found to have sluggish movements, spinal anomalies and irregular leg positioning. Mental development is usually not affected, the child develops well intellectually and successfully adapts to life in society. This form of cerebral palsy is diagnosed in 20-25 % of patients.
Massage therapy
Therapeutic massages must be performed in cycles. It should only be carried out by a trained therapist. The child must receive 4-5 treatments per year. The duration of the massage treatments is 15-30 minutes. The duration can be increased gradually. Parents can also massage their child's feet at home after consulting the doctor.
The massages aim to strengthen the muscles of the thigh and shin and relax them on the outside of the legs. This helps the bones that make up the joint align properly with each other again. In addition to the legs, the buttocks, lower back and upper back are also massaged.
Therapeutic gymnastics
After the massage treatments, gymnastic exercises are performed. They are carried out under the supervision of a professional. Once the child has mastered the correct movements, parents can do the exercises themselves at home. To correct the shape of the legs, exercises are selected that increase muscle tone on the inside of the thighs and shins and reduce it on the outside.
The experts recommend the following as basic exercises:
- Lotus position, which relaxes the muscle group on the outside of the thighs. If the child cannot sit in this position, he simply brings his feet together and bends and separates his knees;
- 'Bicycle', performed in the supine position. The child puts the legs up, with the lower back still on the surface, and moves them in a series of movements that mimic cycling;
- Walk with the weight of your body on the outside of your foot. With each step, the child rolls to the side and rocks from side to side;
- heel and toe walking;
- Walking on a horizontal line, curb, or other object places the feet in close positioning and strains the muscles on the inside of the legs.
The doctor selects exercises for therapeutic training. Otherwise, the condition can lead to flat feet and other complications.
Physical therapy is a complementary measure to therapy. Children with leg curvature should do this daily. Heavy exercises that cause muscle pain should be avoided. This can lead to rejection by the child or have negative consequences for the musculoskeletal system.
Gait changes associated with brain pathology
The main cause of this gait, which is also called senile gait, is not the patient's age, but his fear, a phobia of falling. If this problem is not addressed, the patient's mobility will become more and more limited and they will become less and less functional. A characteristic symptom is a significant improvement in gait when shaking a person's hand.
This change in gait develops against the background of the contraction of certain muscle groups. The faster the affected person tries to move, the more pronounced they become. A distinction is made between the hemiplegic gait and the spastic paraparetic gait. In the first case, the upper extremity (elbows, wrists, fingers) is flexed and the patient's shoulder is turned inward. The patient's leg is stretched in all joints. The paraparetic gait develops in spinal cord injuries and cerebral palsy.
Cerebellar ataxia (damage to the cerebellum) results in an unstable cerebellar-ataxic gait with legs wide apart, steps of different lengths and lateral swaying. Causes include multiple sclerosis, alcohol, tumors, etc.
Spinal cord injuries and sensory polyneuropathies can also lead to a slow ataxic sensory gait - with short, unsteady steps and high foot lift. The affected person has to control his movements using his eyesight.
If the frontal lobe cortex is affected, an ataxic cortical gait (also known as 'fox gait') develops. The person may even walk with their feet in a straight line and their legs may be twisted. Sometimes these patients are simply unable to stand in one place.
This is characteristic of patients with Parkinsonism. The person bends their body forward and walks with small steps, barely lifting their legs off the ground. It looks like he or she is falling, and he or she is trying to move forward so that doesn't happen. The hands are pressed against the body and the patient often stumbles; sometimes he stays in one place for 10 seconds and cannot move forward.
When will your child be able to walk: what do the experts say?

Even if it is difficult not to be proud that your child is already walking quickly on his own while others are still learning to crawl, this is an individual characteristic. Some children actually learn to run faster thanks to their parents' efforts, but this is usually by chance.
In addition, pediatricians and orthopedists do not consider standing early to be a good achievement. Immature ligaments may not be able to withstand the strain and you could end up with flat feet and foot deformities.
The golden rule is: your child will walk when he or she is ready. This willingness can still be refined a little.
The norm for the first steps is very wide and ranges from eight to 18 months. Some pediatricians (Acta Paediatrica study) say the norm is that some children die before the age of 20.
However, there are situations where delay should be a cause for concern.
When is a delay a sign of problems?
A healthy child will definitely take his first steps at the age of 20 months. At this age, not only the muscles and ligaments, but also the child's central nervous system, sense of balance and mental health are already sufficiently developed.
If the child does not walk at all or walks only by hand, he should be examined by a pediatrician, and then the help of specialists - an orthopedist and / or neurologist - will probably be required.
The second important factor is general development before the age of 20 months. As a rule, in Russia parents start to worry at the age of 1 year, in European countries and the USA at the age of 14 months (ScienceDaily).
In this case, experts advise assessing the whole picture: if the child is active, can crawl, can sit up, tries to stand with support and move with the help of a treadmill, reaches for toys, tries to climb onto the bed , jumps when you hold your hands, and the skills are constantly improving - then everything is fine. If motor activity is low and there is no progress, this is a good reason for an examination.
Why does cerebral palsy affect mobility?

Cerebral palsy is a neurological disease caused by damage to the brain. The damage to the central nervous system that a child suffers during or shortly after birth affects muscle tone and mobility, affecting mobility in all respects.
Cerebral palsy causes, among other things, increased muscle tone, abnormal reflexes, limited range of motion, coordination problems, balance problems and various postural problems. All of this affects the way a person moves and can get from one place to another.
Mobility problems depending on the type of cerebral palsy
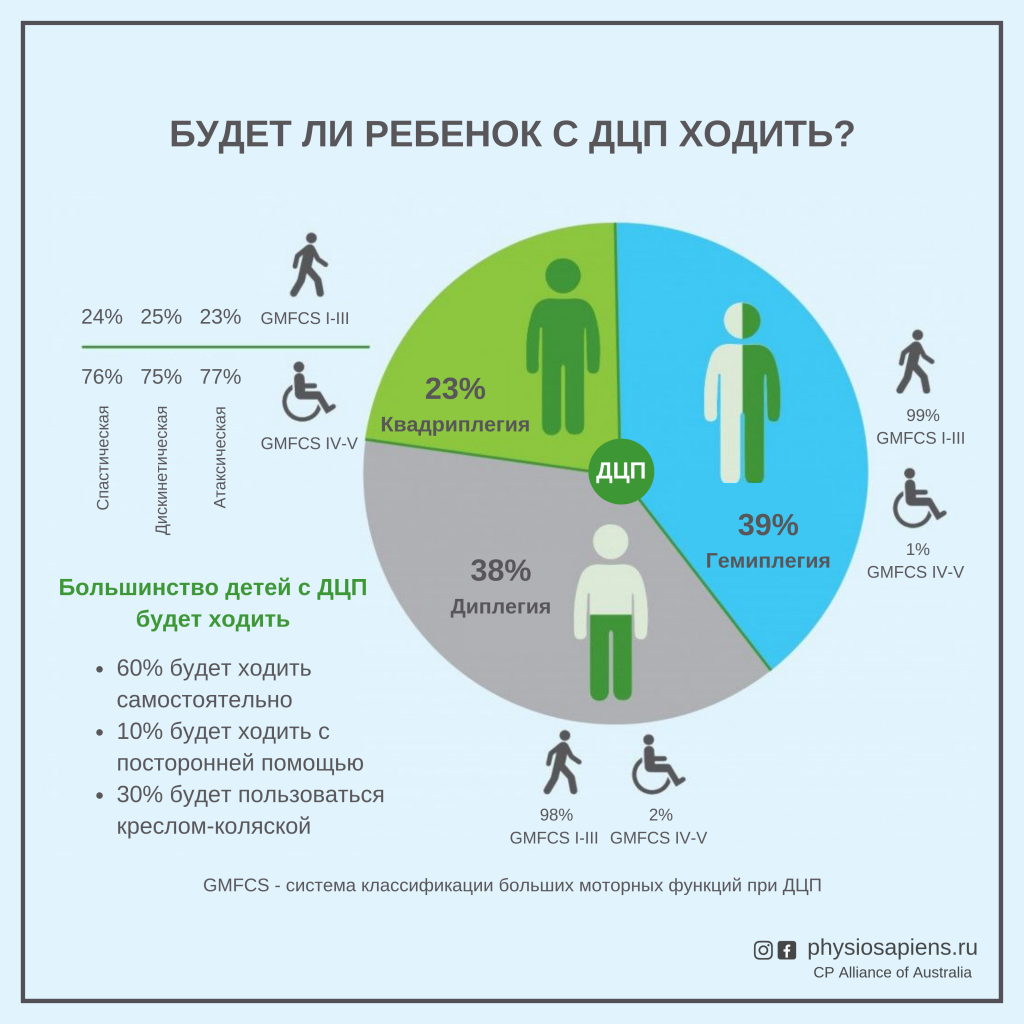
All people with cerebral palsy are different and the degree and type of disability can vary significantly. What most people with cerebral palsy have in common is difficulty moving, getting from one position to another, or moving in space.
The most common form of cerebral palsy is spasticity, which is characterized by increased muscle tone and spastic movements. Tense, stiff, overly tense muscles make it difficult to control movements. When the muscles of the lower limbs are paralyzed, it makes walking difficult and causes a jerky and clumsy gait.
With dyskinetic cerebral palsy, the affected person struggles with involuntary muscle movements. Muscle tension ranges from excessively high to excessively low, meaning movement and control of the limbs is extremely difficult. Ataxic cerebral palsy causes wobbly movements and problems with balance. When walking, a person with this type of cerebral palsy must spread their legs wide to maintain some balance. Mobility also depends on which part of the body is affected and how severely it is affected. For example, if the legs are affected, mobility becomes a major problem.
Causes of dyspraxia
Although the exact causes of dyspraxia are not known, recent neurophysiological research suggests that it is caused by underdevelopment or immaturity of neurons in the brain rather than brain damage. Hypoxic-ischemic brain damage during the perinatal period plays a special role in the development of the disease.
Dyspraxia (impaired ability to perform purposeful movements) cannot be diagnosed until after the age of seven, when it can be differentiated from coordinative motor disorders.
Dyspraxia can only be diagnosed by a pediatrician or a pediatric neurologist or psychoneurologist.

Manifestations of 'clumsy child' syndrome:
- Delayed physical development.
- The child is slow to learn to dress and eat independently.
- The child is careless when eating and uses a knife or fork inadequately
- Clumsiness in any purposeful activity
- Can't jump or doesn't jump well, doesn't ride a bike well, often falls and stumbles when walking.
- Can't play ball well.
- Has difficulty writing and drawing.
- Various psycho-emotional and behavioral complexes.
- Unsteady and sluggish posture.
Children with this diagnosis have some difficulty with social interactions, often with peers refusing to interact with them. It is not easy for an 'unstable' child to adapt to healthy children in everyday life. Such children are more exhausted because their energy expenditure to complete normal daily tasks is much higher than that of healthy peers.

Treatment of dyspraxia
Treatment for dyspraxia should be comprehensive. Depending on the type and severity of the disease, neurologists, psychologists and speech therapists should be involved in the treatment.
- Encourage your child and help them acquire special skills.
- Praise your child for every attempt to perform an activity without considering the outcome.
- Make sure you have a daily routine.
- Set clear and understandable goals for your child.
- Start with activities that your child enjoys.
- Be patient with your child.
Games to promote coordination skills in children with dyspraxia:
(Development of fine motor skills, sense of touch, tactile sensitivity).
Place up to 10 small objects in an opaque cloth bag and show them to the child beforehand: pen, bottle cap, notebook, remote control, etc. The child identifies the objects in the bag by touch.
(Develops fine hand muscles, verbal coherence, memory and imagination).
By saying, 'There's a lock on the door.
who can open it
Pull it, twist it,
Knock and open it!',
Rhythmic rapid interlocking of fingers into a lock, then pulling the handles in different directions, hands with interlaced fingers move from side to side, palms tapping against each other, fingers unclenching, palms pulling apart. Multiple repetitions.
(promotes coordination and speed of movement of large and small muscle groups, develops correct posture, trains attention, improves vision and hearing, coordinates the movements of the trunk and limbs).
You will need 20 cm long sticks, string or pieces of string, toy horses or other toys of your choice.
The children sit on chairs and hold sticks to which toy horses (or other toys) are tied with strings at a distance of 15-20 steps. At a signal, the children begin to wrap the string around the stick and bring the toy closer together.
Read more:- 2 year old child with clubfoot.
- A child begins to have clubfoot between the ages of 1 and 5.
- A person walks on tiptoe.
- The child walks on its toes.
- Equino valgus.
- Tiptoe walking.
- X-shaped legs in a child.
- Child with Komarovsky clubfoot.
