I heel bone fractures:
Class A: Fractures of the heel bone or its processes
Class B: fractures of the calcaneus shaft

- Anatomy of the foot
- Symptoms and causes of heel bone fractures
- Bones of the heel in man
- diagnosis
- Physical examination
- visualization tests
- Treatment methods for fractures depending on the type
- Indications for surgical treatment of a fracture
- Treatment
- Pre-hospital care
- Conservative treatment
- surgical treatment
- Symptoms of a heel bone fracture.
- complications
- complications
- Treatment of a fractured heel bone
- Fractures without dislocation
- Compression and comminuted fractures
- Symptoms of a heel bone fracture
- Treatment of heel bone fractures
- anatomy
- causes
- Diagnosis of heel pain
- Treatment methods for heel pain
- heel spur
- bursitis
- Haglund's deformity
Anatomy of the foot
Let's start by deciphering some terms.
tarsus – The small bones that lie between the tibia and metatarsal bones.
tarsus – The bones of the foot that lie between the tarsal bone and the pontics.
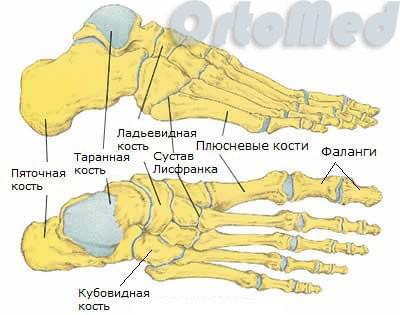
The foot consists of the tarsal bone, the metatarsal bone and the pontics. There are 27 bones in total. The tarsal bone is the rear pivot point of the foot, one of the largest and strongest bones in our body – the heel bone. It is connected to the tendons and muscles of the foot. The tendons, muscles, and the bone itself work together to ensure that the bone is in the correct position and can move correctly when needed.
When a bone fractures, not only does the anatomical structure of the bone change, but also the balance of forces acting on it. The consequences are long-term and possibly lifelong functional limitations.
Symptoms and causes of heel bone fractures
The main cause of 'fractures one of the strongest bones in our body is a jump from a great height with straight legs. In other cases, the cause of this injury is most often a traffic accident or a hit to the heel. Because the heel bone is extremely strong, its fractures are more commonly associated with fractures of other bones in the body, such as the calcaneus. B. the ankle or the thoracic and / or lumbar vertebrae.
Irrespective of this, there are the so-called stress fractures of the heel bone. These can occur both in newly drafted soldiers and in non-professional athletes.

Fractures of the heel bone are associated with:
- pain in the heel area;
- inability to step on the heel;
- heel deformity and heel swelling;
- Bleeding in the heel area can also indicate a possible bone fracture;
- the mobility of the ankle is limited.
Bones of the heel in man
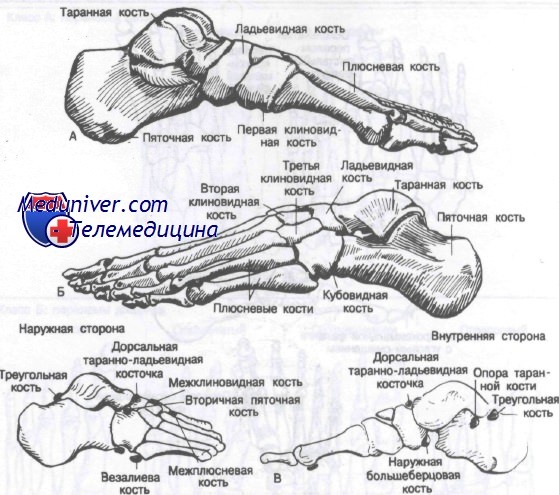
There are 28 bones and 57 joints in the foot. Bone fractures in the foot Fractures in the foot are common and account for 10 % of all fractures. The foot can theoretically be divided into three parts: the posterior part (talus and heel bone), the middle part (scaphoid bone, sphenoid bone and cuboid bone), and the anterior part (metatarsal bone). The figure shows the bones of the foot, including the typical sesamoids, in medial and lateral projection.
The foot has a big one Section of normal movements, including flexion, extension, inversion, and eversion. Also, normal movements include supination, which is a combination of adduction and inversion, and pronation, which is a combination of adduction and extension. The foot consists of two arches: the longitudinal arch (midfoot) and the transverse arch (forefoot). Under normal conditions, body weight pressure is evenly distributed between the forefoot and heel.
The pressure on heads of the metatarsal bones is uneven because the head of the first metatarsal supports twice the weight of the other four bones. The load on the foot is greatest in the push-off phase when walking and running.
broken bones bones of the footFractures of the foot bones generally result from three main injury mechanisms: direct trauma mechanisms, indirect trauma mechanisms, and overloads. The radiographic diagnosis of foot fractures is often complicated by the presence of secondary ossification centers and sesamoid bones. The most common sesamoid bones are the os trigonum, the os tibiale externum, the os peroineum and the os vesalcanum. They can be distinguished from a fracture by the smooth, dense outlines of the bones.
The classificationused in this article differs from the classification used in other articles on this site. Since dislocations of the foot bones (with the exception of the interphalangeal joints) are almost always associated with fractures, the authors included them in the article on fractures.
diagnosis
The diagnosis begins with an interview with the patient. The orthopedist must describe exactly how the injury occurred. If it is a fall from a great height, it is advisable to say from what height.
In addition, the doctor must be informed about chronic diseases and the use of medication. After a thorough medical history, the doctor will collect the first aid kit (bandages, splints, etc.) and begin the physical examination.
Physical examination
The trauma surgeon will first examine the condition of the skin for pallor, open wounds, abrasions or other abnormalities. The doctor then examines the injured area. He checks the pulse at the most important points of the leg to determine whether the blood flow is disturbed.
Characteristic symptoms of a broken heel are:
- severe swelling spreading to the foot and ankle;
- extensive bruising;
- instability of the ankle;
- optical deformation of the heel. inward concavity of the foot, bilateral extension;
- Restriction (or blockage) of joint mobility.
Acute, unbearable pain is characteristic of the injury. Fragment fractures of the heel bone are so severe that they can lead to unconsciousness.
If the heel is not broken, but there is a fracture, the ability to walk is preserved and the pain gradually increases. This process takes up to several weeks (sometimes months).
After a fracture, the foot loses the ability to support body weight, the musculoskeletal system can no longer cope with the load, and the patient cannot even stand with the foot resting on them. The pain increases with lateral compression. After the first examination, the doctor will refer the patient for further examinations.
visualization tests
To confirm the diagnosis, the patient is referred for an X-ray examination. The examination provides information about the type of fracture, the displacement and the number of fragments.
A CT scan (computed tomography) is also performed to examine the condition of the soft tissues and ligaments. Based on the results, the doctor decides how to treat the heel fracture.
Treatment methods for fractures depending on the type
In traumatology, there are two methods of treating this type of injury:
If the fragments are only slightly or not at all displaced, the first method is used: the injured leg is put in a plaster cast. The fragments are aligned beforehand. For uncomplicated fractures, a bandage is placed around the ankle, ankle, and calf (up to the knee). For skull fractures, the limb is cast in a cast up to mid-thigh. The knee is kept in flexion.
With a joint injury and bone displacement, an Ilizarov clamp is applied to the patient to stretch the skeleton: a spoke is passed through the heel bone and a 2 kg weight is hung from the upper part of the arch of the foot. The patient wears the splint for 1.5 months, then a plaster cast is applied (without breaking traction).
Indications for surgical treatment of a fracture
Most patients with a displaced heel fracture require surgical treatment. Goals of the intervention:
If the fracture is closed, the operation is performed after a few days, when the swelling and soft tissue inflammation have subsided. During this time, the leg must be elevated. Open injuries require immediate intervention to clean the wound and remove the damaged tissue. This prevents infection and necrotic changes.
The main surgical method is osteosynthesis. It is carried out in two ways:
- Percutaneous, where the fixation screws are inserted into the fracture site by puncture;
- Open repositioning. The surgeon makes an incision in the foot and inserts the metal structures.
The post-operative swelling subsides after two weeks and blood flow to the tissue begins again.
The operation is performed under general anesthesia. There are no age restrictions, but there are a number of contraindications to manipulation.
Treatment
Pre-hospital care
Heel injuries are immobilized with a splint, cold and painkillers are used. Inflammation of the tendons and ligaments, arthrosis of the tarsal joints limit the load, local anesthesia and anti-inflammatory drugs are used. Severe pain, deterioration in general condition, hyperthermia, local signs of inflammation and effusion are indications for immediate specialist treatment.
Conservative treatment
The conservative treatment of heel pain usually consists of a combination of drug and non-drug therapy. The following techniques can be used:
- security scheme. The degree of stress on the foot and the duration of the limitations are determined individually and range from 1-2 weeks for minor injuries to a year or more for chronic diseases. A cast, orthopedic shoes, crampons, and other aids may be used, as may walking on crutches or with a cane.
- Pharmacological treatment. With inflammatory processes, NSAIDs are prescribed, with infectious diseases, antibiotics are recommended. With trophic ulcers, drugs for aggregation disorders and venous disorders are indicated, and with diabetes, antidiabetic therapy is corrected.
- other methods.. With skin injuries, bandages are used, with hyperkeratosis, special foot treatment is performed, with injuries and inflammatory diseases, patients are referred to physiotherapy and physical therapy.
surgical treatment
The choice of surgical tactics depends on the type of pathology. The following open manipulations can be performed:
- injuries .Injuries: open osteosynthesis of calcaneus fractures, suturing of the Achilles tendon.
- infectious processes.Infectious processes: sequestration, opening of a horn abscess.
- Trophic Ulcers.Skin grafts, bypass surgery after healing, phlebectomy, miniflebectomy.
Symptoms of a heel bone fracture.
The patient complains of pain in the heel area. Examination shows swelling of the heel, which quickly spreads to the Achilles tendon, flattening and widening of the heel, hematoma in the midsole. The contours of the Achilles heel are flattened. The height of the foot decreases and the width at the back increases. Bruising sometimes occurs on the lateral surfaces of the foot (below the ankles) a few hours after the injury.
Supporting the foot is not possible. The mobility of the ankle is preserved. Palpation of the heel is painful. When the heel area is compressed laterally, the pain increases and becomes unbearable. Crepitus is not noted in compression fractures and injuries without fragment displacement. In other cases, the presence of bone crepitations is a variable symptom.
complications
The risk of complications increases in direct proportion to the displacement of the heel fragment and depends on the quality of the reduction - incomplete reduction and secondary displacement increase the risk of complications. In the long term, patients often develop post-traumatic flat feet. Intra-articular fractures of the heel bone often result in inflammation of the subtalar joint.
The diagnosis is made by the trauma surgeon based on history, physical examination, and imaging studies. Heel injuries sometimes go undetected in the face of spinal and ankle injuries, which are very symptomatic. Therefore, all patients with a characteristic injury mechanism (fall on the foot from a height of more than 1.5 m) should be evaluated to rule out a heel fracture. The investigation plan includes:
- External Examination. Deformation of the heel area, the presence of swelling and acute tenderness to pain indicate a fracture. A crunch of the bone is a pathognomonic sign.
- X-ray examination of the heel bone. To confirm the diagnosis and determine the degree of displacement of the fragment, an X-ray is taken in four projections: lateral, axial, oblique and front. The degree of pathological changes is assessed based on the changes in the Belair angle (angle of the calcaneus tuberosity) and Gissan angle (angle between the top edge of the lateral bone and the outer edge of the articular surface).
- Computed tomography of the heel bone. Allows the location of the primary calcaneus fracture line, the size, type and displacement of the fragment to be specified. Determined to choose the best treatment tactics. It is performed in axial, coronal and sagittal views.

Differential diagnosis of heel injuries is carried out with fractures of the heel bone. Imaging studies are crucial.
complications
The risk of complications increases in direct proportion to the displacement of the heel fracture and depends on the quality of the reduction - incomplete reduction and secondary displacement increase the risk of complications. In the long term, patients often develop post-traumatic flat feet. Intra-articular fractures of the heel bone often result in inflammation of the subtalar joint.
The diagnosis is made by the trauma surgeon based on history, physical examination, and imaging studies. Heel injuries sometimes go undetected in the face of spinal and ankle injuries, which are very symptomatic. Therefore, all patients with a characteristic injury mechanism (fall on the foot from a height of more than 1.5 m) should be evaluated to rule out a heel fracture. The investigation plan includes:
- External Examination. Deformation of the heel area, the presence of swelling and acute tenderness to pain indicate a fracture. A crunch of the bone is a pathognomonic sign.
- X-ray examination of the heel bone. To confirm the diagnosis and determine the degree of displacement of the fragment, an X-ray is taken in four projections: lateral, axial, oblique and front. The degree of pathological changes is assessed based on the changes in the Belair angle (angle of the calcaneus tuberosity) and Gissan angle (angle between the top edge of the lateral bone and the outer edge of the articular surface).
- Computed tomography of the heel bone. Allows the location of the primary calcaneus fracture line, the size, type and displacement of the fragment to be specified. Determined to choose the best treatment tactics. It is performed in axial, coronal and sagittal views.
Differential diagnosis of heel injury is carried out with fractures of the heel bone. Imaging findings play a crucial role in this.
Treatment of a fractured heel bone
Treatment usually takes place in the trauma ward and can be conservative or surgical. The treatment program depends on the type and severity of the calcaneus fracture and includes open or closed reduction (in the case of a dislocation), immobilization, anesthesia, a special regime, the use of aids (crutches).
Fractures without dislocation
Heel fractures without dislocation and marginal fractures of the tibia are treated conservatively. After the injury site has been anesthetized, a cast boot with carefully modeled arches is placed on the leg. In the first few days after the injury, painkillers are given intramuscularly to relieve the pain. The patient is referred for physical therapy and UHF is administered. The plaster cast is removed after 8-10 weeks. The patient is recommended to wear orthopedic shoes with supinators for at least 6 months.
Compression and comminuted fractures
The treatment of compound intra-articular fractures of the calcaneus presents great difficulties due to the difficulty of realigning the fracture and fixing it until healed. Depending on the type of fracture and the type of displacement, the following techniques can be used:
- Closed repositioning (Closed repositioning). This is carried out using special manual techniques. First, the longitudinal displacement is corrected, then the heel is flattened, and finally the lateral displacement of the fragments is corrected. The limb is immobilized with a plaster cast.
- Single stage skeletal traction. Allows for stronger traction and greater accuracy of manipulation. It is performed with one or two spokes inserted through the fracture. Clamps are attached to the spokes, the above techniques are used, additional spokes are used to immobilize the bone fragments, and a cast is applied.
- Repositioning with the 'Ilizarov apparatus. It is indicated for late heel injuries that cannot be corrected by a one-stage reduction. It is carried out for 1-2 weeks under regular X-ray control. Subsequent treatment follows the same principles as in single-stage traction.
Symptoms of a heel bone fracture
An open fracture is associated with extensive tissue damage and a bleeding wound, sometimes containing bone fragments. A closed fracture of the heel bone is characterized by the following symptoms:
These symptoms are also characteristic of severe bruises, so the patient may not even notice the fracture at first, which can later lead to serious complications. Therefore, if the heel area is severely bruised and the symptoms described above appear, an urgent visit to the doctor and an X-ray examination are necessary. In some cases, computed tomography is also performed to clarify the diagnosis.
Treatment of heel bone fractures

First, the patient needs a local anesthetic to relieve the pain. The doctor then inserts the deformed bone fragments manually if the fracture was accompanied by a dislocation. Once the initial swelling has subsided, a plaster cast is placed over the injury site up to the knee. You can walk on crutches, but light weight bearing on the forefoot is allowed after four weeks at the earliest. The plaster cast is usually removed after a month and a half, and the rehabilitation period should not be extended as normal limb support may be lost.

Severe intra-articular fractures of the heel bone can lead to permanent disability.
With the rarest of exceptions, it is an impact or a high-energy load of the heel on the back of the foot. fall. A wrong jump. For this reason, heel bone fractures are often combined with spinal fractures. Eventually, the power is transmitted through the lower limbs to the spine. And the greater the energy of the injury, the greater the likelihood that the spine will also be damaged.
The patient usually feels severe pain. Shortly after the injury, there is swelling and later bruising, which can extend to the fingernails and knee joint. X-rays are always taken. Computed tomography (CT) is performed in the following cases: with insufficiently clear X-ray images, with suspected fractures in certain areas of the heel, in order to accurately plan the operation (if surgery is indicated).
First of all, all fractures of the heel bone are divided into intra-articular and extra-articular fractures. Surgery is more indicated for intra-articular fractures. In other cases, the prognosis for rehabilitation is worse than for extra-articular injuries. There is also a 'duckbill' fracture (this is what the heel looks like on an x-ray seen from the side with this type of fracture). In this type of fracture, the strong Achilles tendon pulls part of the calcaneus shaft up past the insertion area. As a result, the heel splits in two and an X-ray reveals an image resembling an open duckbill. Duckbill fractures are one of the few situations in which emergency heel fracture surgery may be indicated. Because the Achilles tendon pulls and moves the broken part of the heel so much that it presses heavily on the skin from the inside, which can lead to necrosis.
anatomy
The condition, which manifests itself as pain on exertion, is distinguished on examination from possible fractures or fractures of the heel bone and tears of the connective tissue in the muscular apparatus of the foot.
In order to make a correct diagnosis, the compact component of the synovial membrane of the foot is carefully palpated. This is essentially a muscular formation located between the heads of the metatarsal bones and the base of the heel bone. Its function is to form the longitudinal arch of the foot, which cushions the body as it moves.
Since the transverse arch and the heel bone, which has a natural point, are also present, the greatest pressure occurs at the point of attachment.
In traumatic situations, in the event of overload or metabolic disorders, this leads to the formation of a bony outgrowth on the surface of the caudal tubercle, which causes pain. This is called a heel spur, which looks like a sharp spike on X-rays.
causes
This distortion of natural anatomy is usually caused by degenerative changes throughout the body. Due to the disruption of internal homeostasis, 'plantar fasciitis' is most common in the elderly.
In young and middle-aged people, it can be the result of physical overload, e.g. B. through athletic training, competitions or the type of activity with long periods of standing or lifting heavy weights.
Uncomfortable, tight shoes with high heels, traumatic damage to the ligament apparatus as a result of a fall, sprain or serious bruise, and obesity also contribute to the symptoms of the disease. In people with an intact immune system, the body is usually able to activate compensatory mechanisms itself in order to heal micro-injuries.
With age and degeneration-related changes in the metabolic processes, there is a proliferating reaction, e.g. B. with heel calluses in the area of the bone head, which lead to an excruciating pain syndrome due to the increased irritation of the nerve bundles.
Diagnosis of heel pain
When you visit the doctor, you will be examined according to a specific plan. The doctor will question you in detail about your symptoms, determine the type, extent and location of the pain and perform an examination of the painful area. If necessary, he will order a series of laboratory and instrumental examinations. This includes:
- A general blood test. It is needed to detect an inflammatory process, a decrease in hemoglobin in anemia, or a change in platelet count in clotting problems.
- blood chemistry. It shows changes in metabolism and helps to identify diabetic changes, rheumatic diseases, cystic fibrosis and infections caused by pathogenic streptococci.
- tumor marker tests. It is needed if bone tumors are suspected.
- Culture of purulent secretions to detect flora. Required in the presence of purulent lesions, selection of antimicrobial drugs.
- X-ray examination of the bones and soft tissues of the foot. Helps diagnose inexplicable pain in the heel, including after trauma, against the background of degenerative processes.
- Ultrasound for arthritis, bursitis, neuroma, tunnel syndrome and localization of inflammation.
- Puncture of the bone or synovial membrane when an infection or tumor is suspected.
- CT or MRI examination for the precise diagnosis of changes in the structures in the foot and heel area.
Treatment methods for heel pain
When it comes to heel disorders, attempts are made to treat them conservatively, but this is not always possible. If conservative treatment is ineffective, then this is an indication for surgery. Surgical treatment quickly and permanently eliminates the cause of the pain in the heel area. Modern surgery is based on minimally invasive, outpatient techniques with minimal trauma and short recovery time.
heel spur
Surgical treatment of the heel spur is indicated if conservative treatment is unsuccessful within 6 months. The types of surgeries for heel spurs are osteophyte removal and plantar fasciotomy.
These procedures are performed under local anesthesia. Through a small incision, the surgeon inserts an endoscopic probe and microsurgical instruments. Under the microscope, he removes the bony process and, if necessary, the inflamed fascia. A thick piece of the adductor muscle of the big toe is cut away to prevent further nerve compression.
If heel spur pain is not caused by osteophytes but by excessive tension on the soleus tendon, a tenotomy — a partial severing of the tendon — is done. The intervention is performed without incisions, through punctures, using high-frequency current (radiofrequency tenotomy).
bursitis
Bursectomy - the surgical removal of the joint capsule - is indicated when bursitis cannot be treated conservatively. The operation is performed without incisions using an arthroscopic technique.
Microsurgical instruments and a miniature video camera are inserted into the joint through 2-3 punctures with a diameter of 4-5 mm. This is followed by dissection and removal of the joint capsule. The incisions are covered with a sterile bandage. The operation takes about 30 minutes. The recovery time is 2 days.
Haglund's deformity
If conservative treatment of Haglund's deformity is unsuccessful, surgery is indicated. During the endoscopic procedure – without incisions – the bony process is removed from the surface of the calcaneus tubercle and the posterior capsule of the calcaneus is excised. This procedure restores the mechanical function of the Achilles tendon and eliminates the cause of the pain.
Read more:- tibia and fibula.
- Structure of the human heel.
- bones in the heel.
- Bones of the human ankle.
- heel bone injury.
- Structure of the heel.
- Bones of the tarsal bone of the hand.
- bones of the foot.
