'I just try to stick to the simplest principles. I tell my patients that we need to strengthen what is weakened and weaken what is tense. Because we don't want other muscles to work too hard.' Rina Pandya.
- Foot paralysis: causes, symptoms, treatment of the horse's foot
- causes
- ankle capsule
- tendons of the ankle
- Bad habits that worsen the health of the musculoskeletal system
- Foot exercises for the teenager
- Muscles of the ankle-foot system
- pronation
- causes and symptoms
- Treatment
- Consequences of weakness and overwork
- The importance of posture
- Levels of movement
- sagittal plane
- Frontal plane.
- Transverse (horizontal) plane
- ICD-10
- causes
- Symptoms of foot paresis
- Other symptoms include:
- Complications associated with foot paralysis
- Classification and forms of pathology
- How is a diagnosis made?
Foot paralysis: causes, symptoms, treatment of the horse's foot
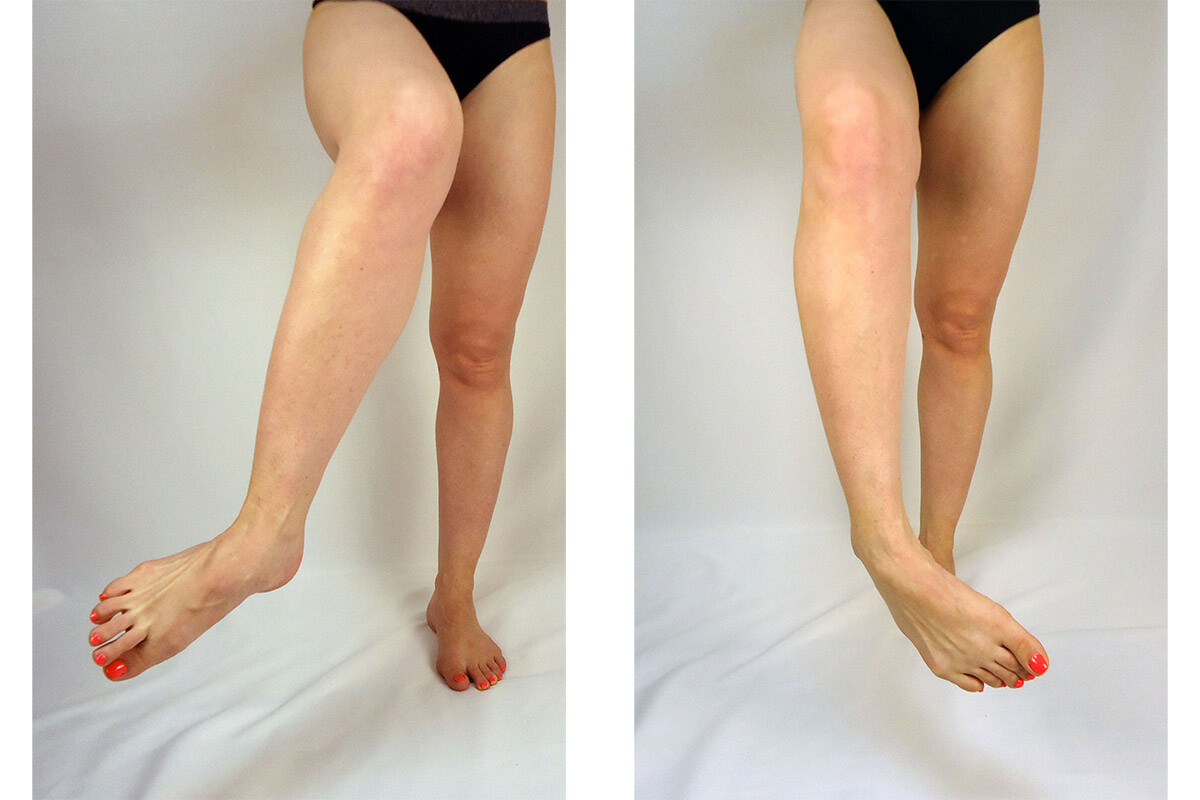
Foot paralysis is a defect in which the foot does not straighten and bends when walking. It is also known as 'horse foot'. This paralysis occurs as a result of a foot injury, a herniated disc, damage to the sciatic nerve, and other conditions. The doctors at the health studio have been treating foot paralysis using conservative methods since 2003.
Foot paralysis is a severe weakness of the leg muscles. Because of this defect, the foot does not lift and wobbles when walking. Other names for this condition are 'drop foot' or 'horse foot' and 'foot paralysis'.
The disease often begins with a stabbing pain in the back and then extends below the knee. Soon the pain subsides and the foot no longer moves and hangs when walking. The affected person has to lift their foot up so that it doesn't drag on the floor. The foot can twist outward or inward, making walking difficult and increasing the risk of a fall. A person with foot paralysis cannot stand or walk on their heels.
causes
- Intervertebral prolapse. This disease causes compression and even death of the spinal cord nerve roots that supply the foot muscles.
- Damage to the sciatic nerve resulting from trauma, a car accident, or an improperly performed injection. A person with this diagnosis has a panting foot and may have paralysis of all the muscles of the leg except the muscles of the anterior surface of the thigh.
- 'Cauda equina syndrome - compression of the nerve roots in the spinal canal.
- Paralysis of the lumbosacral plexus.
A person with foot paresis has a 'cockcrow': the patient lifts the leg up or drags it along the ground. People can adapt in another way: they put one foot on their toes and lift their thighs up. Or he spreads his legs too far apart so that he doesn't have to lift his thigh. Due to the extensor paralysis, the foot does not lift, it folds when walking and bends to more than 90 %.
ankle capsule
capsuleThe capsule surrounding the ankle joint is divided into four parts (ligaments): anterior, posterior, lateral and medial. The capsule is weak anteriorly and posteriorly, but is reinforced by ligaments on the interior and exterior. The anterior ligament is thin and connects the anterior surface of the tibia to the tibial head and is usually injured along with extensive tears of the collateral ligament.

The talus bone is wider at the front
Rear ligament The anterior ligament is shorter than the collateral ligament and runs from the posterior edge of the tibia to the posterior surface of the talus. The collateral ligament is divided into three main bundles, which are among the most commonly injured ligaments in the human body. Between the lateral malleolus and the femoral neck is the anterior fibular ligament, which is most commonly injured in ankle joint injuries.

During dorsiflexion, the wide anterior portion of the talar block enters the foramen of the ankle joint, preventing movement of the ankle joint. During plantar flexion of the ankle, the narrow posterior portion of the block is located within the foramen of the ankle and allows for significant reversal movement in the joint.
Between the outer ankle Between the lateral malleolus and the talus bone (which is sometimes presented as a separate unit and called the talus bone) is the posterior talofibular ligament, and the calcaneofibular ligament extends from the lateral malleolus to the calcaneus. Proximal to the lateral ligament group, the fibula is connected to the tibia by a series of strong fibers that together form what is known as the intertibial syndesmosis. This syndesmosis consists of an intertibial membrane that connects the tibia and fibula along its entire length. In the lower part, the web is reinforced by two thickened fiber bundles: the anterior inferior intertibial ligament and the posterior intertibial ligament.
tendons of the ankle
Superficial to the joint capsule Above the joint capsule of the ankle joint are the tendons, which do not attach to the joint itself, but all run over the joint, which is important when considering injuries related to this joint. These tendons are divided into two groups: the extensor and flexor tendons of the foot. The extensor tendons run along the front of the ankle joint, while the flexor tendons run along the back of the inside of the ankle. The third group is the tendons of the fibula muscles, which run behind the lateral malleolus. These tendons are surrounded by synovial sheaths; some are up to 8 cm long.
Superficial tendons On the surface of the tendons are three spreading bundles of fibers that hold the tendons in place and prevent them from moving. These bundles are classified similarly to tendons. A distinction is made accordingly between the extensor tendon bundle, the flexor tendon bundle and the fibula tendon bundle. The extensor tendon is divided into the upper and lower tendons. The flexor tendon bundle consists of a single bundle of fibers that runs behind the medial malleolus. The fibularis retainer is divided into two parts – the upper and lower fibularis muscle tendon retainers.
Bad habits that worsen the health of the musculoskeletal system
Figures 17-22 show some examples of abnormal (left) and normal (right) daily postures and movements in children and adolescents.
| ❌ ✔ | ❌ ✔ |
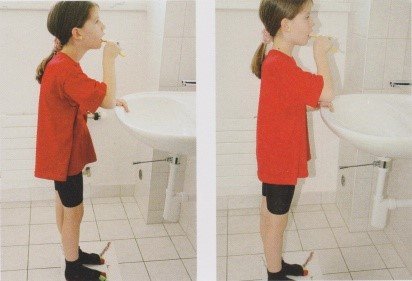 | 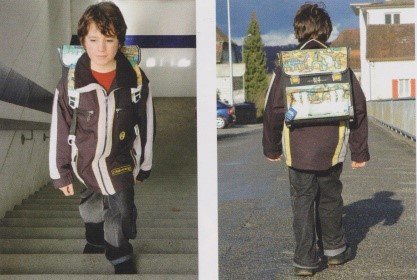 |
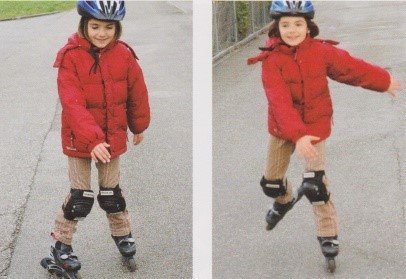 | 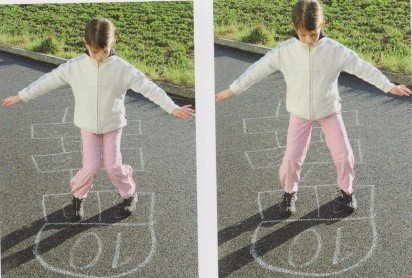 |
 | 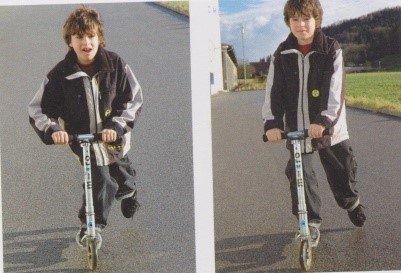 |
Foot exercises for the teenager
Fig. 23-33 shows a training for older teenagers:
| Training according to the spiral dynamic principle by Christoph Larsen (Switzerland) for dynamic foot stabilization with felt exercises (Fig. 23) | 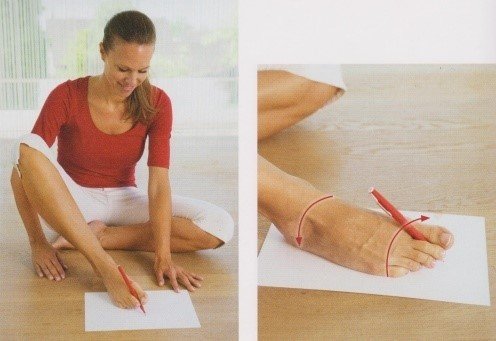 | |
| Training according to the spiral dynamic principle of Christoph Larsen (Switzerland) with latex bands with different muscle densities, which are involved in maintaining the longitudinal arch of the foot (Fig. 24) |  | |
| Training with an unstable surface (balancing cushion) to dynamically load not only the muscles involved in maintaining the longitudinal arch, but also the entire body posture (Fig. 25-26); recommended for hypermobility of the ligamentous system in children. The task is to maintain balance with your feet parallel to the floor (on two feet, then on one) for 1-5 minutes. | ||
| Training the ligament-tendon apparatus of the foot and lower leg with an elastic band (Fig. 27) helps to train the small muscles of the foot, as well as the calf muscle and biceps muscle. |  | |
| Training the muscles of the foot and long fibula, which are involved in maintaining the longitudinal arch of the foot, using a massage ball (Fig. 28) |  | |
| Training the inner and outer head of the biceps muscle on the stairs (as an example) to achieve correct stabilization of the heel bone on the foot, especially in cases of valgus (Fig.29) | 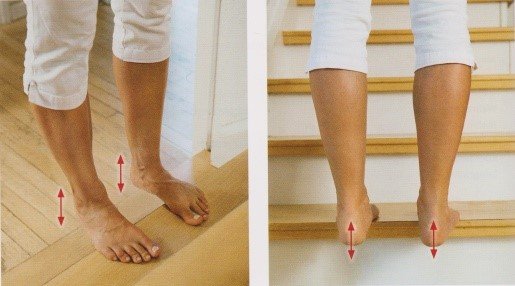 | |
| Training the body's postural stabilization system in space on a flexible and unstable surface (Fig. 30) | 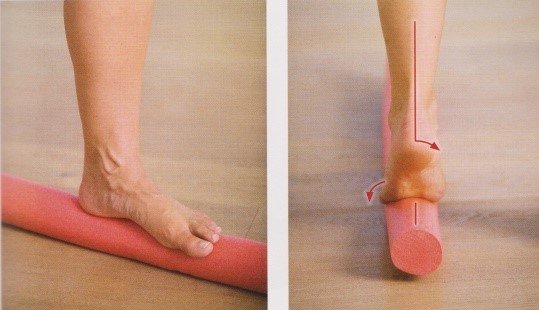 | |
| Training long flexion and extension of the thumb and toes (Fig.31); the exercise is suitable for all types of flat feet. Press your thumb to the floor with your palm and try to lift it, and vice versa, extend your thumb and try to bend it, holding it with your palm. Then press the 2nd and 5th fingers to the floor with your hand and raise the 3rd and 4th. | 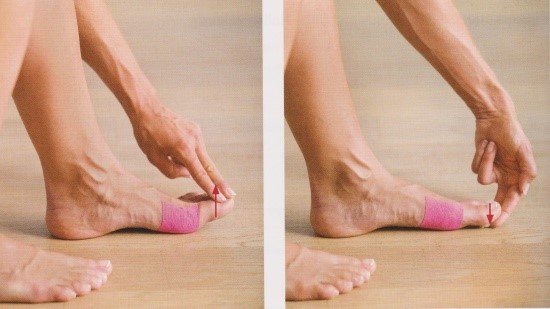 | |
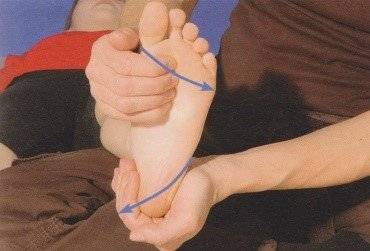
| Kneading the ligaments/tendons of the ankle joint while sitting/studying (Fig. 32) | 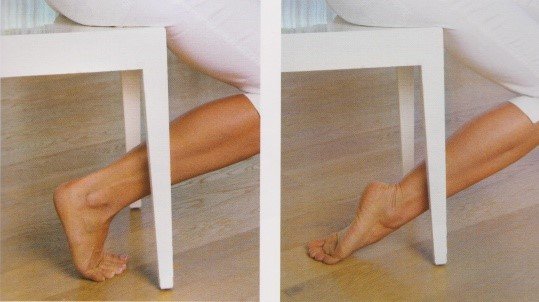 | |
| Example of a very important exercise for the development of the foot muscles, especially for combined and transverse flat feet (Fig.33) | 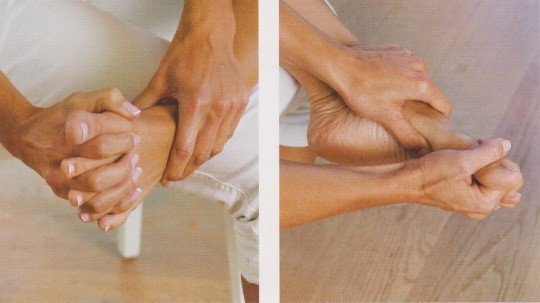 | |
Muscles of the ankle-foot system
The human ankle-joint complex plays a fundamental role in walking and other activities of daily living. It is a very complex anatomical system. Any injury, damage or neuromuscular disorder to this complex system affects the interaction of muscles, bones and ligaments and leads to dysfunction, instability or reduced mobility.
This is primarily due to the extremely complex muscular interactions involved in the movements of the ankle and foot. An important fact is that all of the muscles that move these joints begin on the shinbone, some on the thigh, and end on the foot.
- musculus tibialis anterior;
- The long extensor of the big toe;
- The long toe extensor and third fibular toe are responsible for dorsiflexing the foot and extending the toes.
Lateral muscle groupThe lateral muscle group consists of the long toe, the short toe and the third fibula and ensures the pronation of the foot.
Deep posterior tibialis muscle groupThe muscle group of the posterior tibia, the longus of the toes and the longus of the toes are particularly responsible for the supination of the foot and the flexion of the toes.
The soleus flexion of the foot is provided by the superficial muscles of the posterior group - the calf muscle, the cambioideus muscle and the placialis muscle. The calf and placialis muscles are connected to the heel bone via the Achilles tendon. The calf muscle and soleus muscle begin above the knee joint, at waist level, while the cambioideus muscle begins at shin level. This distinction is important for understanding the interaction between knee and ankle joints.
What movements are performed at the ankle?
The movements of the foot affect the whole foot or specific parts of the foot. Dorsiflexion or plantar flexion of the foot is possible in the sagittal plane.

pronation

- M. peroneus longus
- Short Fibula – M. peroneus brevis
- Third fibula – M. peroneus tertius
In the horizontal plane, abduction and adduction are possible (not to be confused with outward or inward rotation of the knee and/or hip joint, although in practice these movements are often combined).
Abduction – the forefoot is tilted outward.

Abduction (adduction) – the forefoot deviates inward.

In practice, there is an automatic combination of three types of movement:
Abduction, pronation and extension together form the eversion of the foot. Pictured left.
- Tendon of the long toe – M. extensor digitorum longus
- Fibula longus – Peroneus longus muscle
- Short Fibula – M. peroneus brevis
- Peroneus tertius: third fibula
Adduction, supination and flexion combine to form the inversion of the foot.
- Musculus tibialis anterior – M. tibialis anterior
- Flexor of the long toe – M. flexor digitorum longus
- Flexor of the long toe – flexor hallucis longus
- Musculus tibialis posterior – M. tibialis posterior
causes and symptoms
Paralysis of the foot is called clubfoot, clubfoot, or clubfoot. The condition is caused by damage to the root of the 5th lumbar nerve, which innervates the extensor muscles of the foot. Patients with foot paralysis feel more comfortable in boots or stiff, high boots because they prevent the foot from sagging. Walking in high-heeled shoes is problematic. Patients often have to use a walking stick. Getting into a car or going up and down stairs is uncomfortable.
On the other hand, foot paralysis caused by damage to the root of the first spinal-sacral nerve can manifest itself in a slightly different way. Patients cannot stand on their toes. You walk resting on the painful foot and have difficulty stepping on car pedals.
The cause of these complaints is usually a lumbar disc herniation, which leads to compression and partial or even complete atrophy of the nerve roots. In the Yusupov Hospital, the cause of the foot paresis is clarified with the help of an MRI scan. The examination is carried out using the most modern CT scanners from the world's leading manufacturers.
Mild positional gastroparesis develops when sitting with the foot on the thigh. It disappears immediately after changing posture or walking. Diabetes, a cause of diabetic polyneuropathy, can lead to foot paresis without the presence of a previous pain syndrome. Foot paresis develops with alcoholic neuropathy or trauma to the lower limbs. Doctors at Yusupov Hospital can easily determine the above causes of foot paresis with the help of an MRI scan, which does not reveal a herniated disc or compression of the spinal cord root.
Treatment
Patients often ask: 'What should I do if foot paralysis is diagnosed?'. Foot paralysis with a herniated disc cannot be treated with conservative methods. Only a neurosurgical procedure, during which the hernia is removed and the affected root is freed from compression, can save the damaged nerve or create the best possible conditions for restoring its function. This procedure is carried out under the operating microscope (microdiscectomy) by leading neurosurgeons in partner clinics.
The appropriate time to perform the procedure is limited. The maximum duration is 7-10 days. Operations performed after a month or more do not show significant clinical improvement. Can foot paralysis be cured? It is an absolute mistake to recommend long-term conservative treatment to patients. This category of patients should be treated by neurosurgery specialists. The neurologists, neurologists, spine surgeons and specialists in unconventional therapies at the Yusupov Hospital are immediately called in for consultations with neurosurgeons. It takes 6 to 12 months for foot function to recover after surgery.
Has anyone cured foot paralysis without surgery? Foot paralysis that is not caused by compression of the spinal nerve roots can be treated conservatively. Neurologists at Yusupov Hospital prescribe individual therapy, taking into account the cause of the disease, age, gender and physical characteristics. The therapy consists of at least five treatments.
How long does it take to treat foot paralysis? The foot recovers within 4-6 weeks. The patient undergoes treatment 2-3 times a week. The course of treatment consists of the following treatments:
- decimetric resonance wave therapy;
- Acupuncture;
- intra-articular injections of the cartilage-protecting preparation Fermatron;
- exercises on simulators;
- Joint and spinal blocks with local anesthesia.
Physiotherapy for foot paresis includes electrical stimulation of the affected muscles and nerves. Treatment of foot paralysis in Yusupov Hospital restores the correct position and mobility of the foot, normalizes metabolism and blood circulation, and strengthens the muscles and ligaments of the legs. At the end of the course, the rehabilitation doctor gives the patient a manual with exercises that they can do independently at home.
Consequences of weakness and overwork
Consequences of weakness of the long extensor digitorum muscle
As the main extensor muscle of the metatarsophalangeal joints of the lateral toe phalanges, weakness of the long digitorus extensor reduces the affected person's ability to lift the toes off the ground during the transfer phase of gait and, like the long digitorus extensor, controls the lowering of the toes to the ground when the heel hits the ground touched.
Consequences of tension in the long toe extensor
The tension of the long toe flexors has similar effects on the lateral phalanges as the tension of the long toe flexors on the big toe. The metatarsophalangeal joints of the big toes become hyperextended, and usually the proximal and distal interphalangeal joints become flexed due to overloading of the long finger flexors. Similar to tension in the long flexor of the big toe, the resulting claw-like deformity is painful and functionally limiting.
The importance of posture
Posture is the relative position of the head, shoulder girdle, spine, pelvis, hips, knees and ankles to one another.
In order for a person to maintain an upright posture, every part of their musculoskeletal system must be perfectly balanced, so that the muscles need to be stressed as little as possible. Thanks to lumbar and cervical lordosis, thoracic kyphosis, and the correct alignment of the shoulder and pelvic girdles as well as the lower limbs, humans are able to stand still and walk.
If this is not the case, abnormal posture of the body parts can lead to severe balance and gait problems (Hasegawa, 2017). Changes in posture can be caused by muscle tension or weakness, e.g. B. Changes in the longitudinal tension of the hip flexors and hamstrings affect the pelvic position. According to Janda, 'muscular imbalance is an imbalance in the relationship between muscles that tend to tense or shorten and muscles that tend to inhibit' (Page, 2010).
Levels of movement
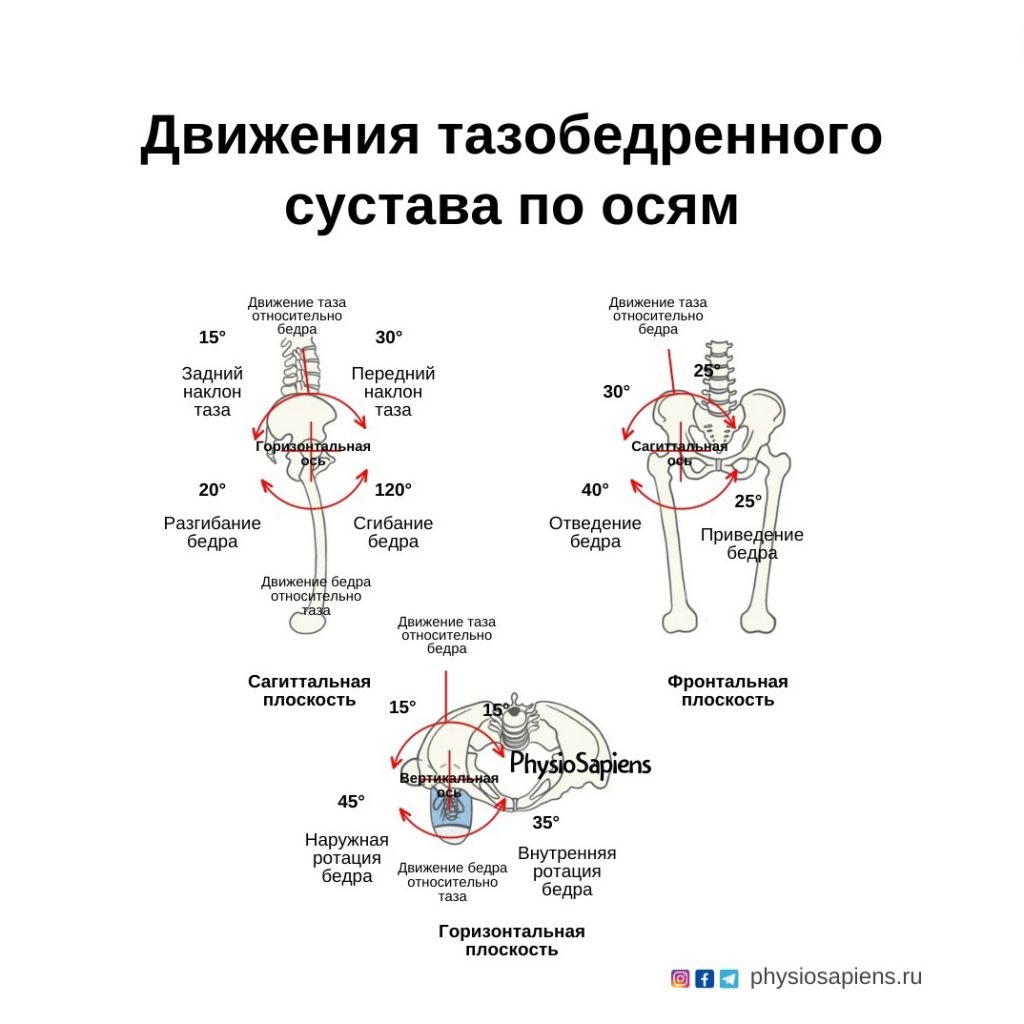
Movement in the hip joint occurs in three planes:
- Flexion/extension in the sagittal plane;
- adduction/extension in the frontal plane;
- External/internal rotation in the transverse (horizontal) plane.
sagittal plane
- The extension and flexion movements of the hip can be assessed using the modified Thomas test and the straight leg raise test (Rose-Dulcina, 2022).
- The straight leg raise test allows the doctor to assess the flexibility and elasticity of the hamstrings.
- The modified Thomas test is a reliable indicator of hip flexion contracture, but only if lumbar motion is controlled during the test (Vigotsky, 2016).
Frontal plane.
- The functional role of the hip adductors is to stabilize the hip in the frontal plane during the single-leg support phase of the gait cycle.
- The posterior head of the adductor major muscle assists the hamstrings in hip extension, while the other adductor muscles assist in hip flexion (Neumann, 2010).
Transverse (horizontal) plane
- When the hip joint is in flexion, the following external rotators become internal rotators of the hip: gluteus medius, posterior fibers of gluteus medius, anterior fibers of gluteus medius.
- The range of hip rotation during gait varies between 2.8 and 11.8 degrees and tends to be greatest during the leg support phase (mid stance phase). The smallest range of hip rotation is observed at the end of the support phase (Uemura, 2018).
- Hip internal rotation is necessary for hip extension at the end of the gait cycle (Dawson, 2022).
ICD-10

Tendinitis of the foot is an inflammation of the synovial membrane of tendons located on the dorsal or plantar surface of the foot. Primary tendinitis develops as a result of sports or occupational overload of a certain muscle group, secondary as a result of a spreading infection (in purulent processes and infectious diseases) or reactive toxic inflammation (in rheumatic diseases).

causes
Primary tendinitis of the foot is usually caused by microtrauma of the tendon sheaths as a result of increased stress or by a violation of the anatomical relationships of the individual structures of the foot. Primary tendinitis of the foot is often diagnosed in skiers, figure skaters and ballerinas, as well as people with flat feet and other congenital or acquired foot deformities.
Acute purulent tendinitis of the foot is caused by contact or hematogenous spread of infection from a purulent focus (infected foot wound, panaritis, purulent arthritis, arthrosis, abscess, phlegmon, etc.). Chronic tendinitis can develop in a variety of specific and nonspecific infectious diseases: tuberculosis, gonorrhea, brucellosis or influenza. In rheumatic diseases (Reiter's syndrome, Bechterew's disease, systemic scleroderma, rheumatism and rheumatoid arthritis), chronic tendonitis of the foot arises from reactive inflammation of a toxic nature.
Symptoms of foot paresis
With this defect, the patient's foot cannot grow together and becomes limp when walking.
A periarticular 'growling' gait is characteristic of foot paresis. The patient may drag their toes on the ground or attempt to lift the foot higher than normal with each step to avoid damage to the foot.
This condition is also known as 'panting', 'horse foot' or 'foot paralysis'.
With foot paresis, it is also characteristic when the patient puts the foot on the toes and sharply raises the thigh in order to avoid sharp contact between the damaged foot and the ground.
Paresis can also be indicated by a gait with excessive leg abduction in order to avoid sharp lifting of the thigh.
Patients with dysesthesia (dysaesthesiae - dys + Greek aisthesis feeling) of the nerve fibers in the soles of the feet have a gait similar to that of patients with foot paresis. These movements, reminiscent of walking barefoot on hot sand, cause very strong sensations of pain. An accurate diagnosis can only be made by examining the patient.
Other symptoms include:
- Tingling, numbness and mild pain in the foot, a symptom indicating a problem in the lumbar spine with damage to the sciatic nerve, probably caused by a herniated disc in the lumbar spine;
- Difficulty with all activities involving the foot – climbing stairs;
- inability to curl toes;
- problems walking on heels;
- Muscle wasting in the legs (characteristic of a herniated disc and spinal dysfunction).
Complications associated with foot paralysis
Without proper treatment, foot paresis leads to increased symptoms that can lead to complications:
- Decreased muscle strength in the legs;
- Deformation of the foot. (At the beginning of the disease, the patient finds it easy to put the foot in the correct position, but over time this becomes increasingly difficult, which can lead to ossification of the foot in an abnormal position). To prevent foot deformity, it is necessary to diagnose and determine the cause of the defect: intervertebral hernia, muscle spasm or another cause.
- Paralysis of the foot occurs when the form is severe. In this case, it is very important to fix the foot in the correct position, for which orthopedic shoes can be used.
By seeking qualified medical help in treating the vestibular foot, the patient will be able to move freely again.
Classification and forms of pathology
Depending on the etiology, tenovaginitis is divided into the following types of lesions:
- Septic or infectious diseases, which, depending on the pathogen, are divided into nonspecific and specific diseases
- Non-infectious, occupational or reactive in nature
Depending on the severity and intensity of the symptoms, they can be divided into acute, subacute and chronic.
Depending on the type of inflammatory process, they are divided into serous, serous-fibrinous and purulent forms.
Each type of inflammation has three stages: the initially benign, the exudative serous and the chronic form.
How is a diagnosis made?
To make the correct diagnosis, laboratory and instrumental studies are carried out. Laboratory tests include blood tests, a pus swab to detect pathogens, antibiotic sensitivity tests, synovial fluid and a biopsy sample.
X-rays or CT scans are used to differentiate the disease from osteoarthritis, arthritis or osteoarthritis.
MRI is the preferred instrumental method, as it most informatively shows the location and tissue coverage of the inflammatory process, the presence of degenerative changes and the condition of the tendon-tendon apparatus.
The specialists of the MRI clinic diagnose tendonitis of the foot based on the images obtained, which speeds up the process of making the correct diagnosis and helps to develop effective treatment tactics for tendinitis of the tendon sheath, ligaments and tendons on the foot
Read more:- The long section of the big toe.
- hindfoot.
- lower leg muscles.
- pronation and supination.
- ligaments and tendons of the foot.
- muscles and tendons of the foot.
- tendons of the ankle.
- flexor muscle of the big toe.
