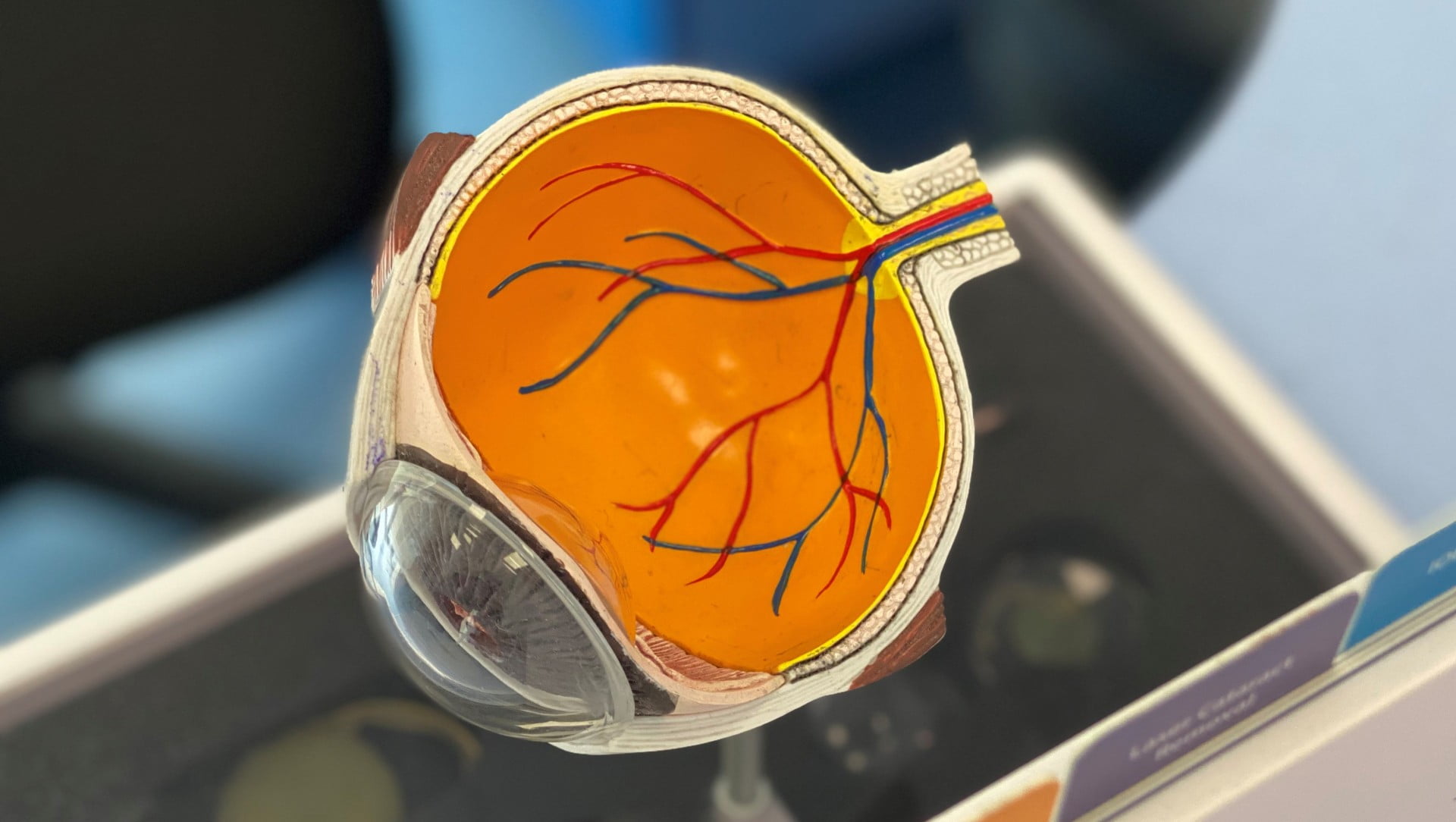
The decision on how surgeons perform an eye amputation depends on the patient's clinical situation and the disease requiring enucleation. This procedure is only used in the most extreme cases, when the life of a person with advanced eye cancer is at stake.
Lower limb bypass surgery

In addition to varicose veins, there are a number of other diseases that can cause varicose veins in the legs. As a result, the vessels can narrow to a critical point and stop supplying nutrients to the tissue.
The phlebologist performs bypass surgery to restore normal blood flow. A shunt (part of the vessel) is inserted to bypass the damaged area of the vein so that blood flow can return to the tissue and the tissue is provided with necessary nutrients.
Where the shunt is inserted depends on the extent of the damage to the vessel. Areas of vein damage:
- thigh area. An incision is made in the groin, the edge of the shunt is inserted into the abdominal aorta, and the other part of the shunt fits into a section of the healthy vein in the thigh.
- Thigh and hamstring tendon. In this case, an incision is made in the groin and the back of the knee. The shunt connects a healthy vein in the thigh area and an artery that runs below the knee.
- Thigh and shin area. Your own vein is used here, connecting the great saphenous vein to the arterial blood supply. A small incision is made in the groin and shinbone.
- Bypass technology. When all vessels in the affected area are only partially supplied with blood. Then the doctor inserts a shunt into several healthy sections of the vein to normalize blood flow.
- Foot area. Performed to restore blood flow to the toes. Part of the great saphenous vein is used as a shunt.
- Biological (natural) shunts. The biological shunt is very powerful: it can stop arterial blood flow. A biological shunt is often used in medicine because the body's own tissue adapts better. The material for the shunt is taken from the patient's femoral veins.
- Mechanical or synthetic shunts. Are used for extensive vascular lesions. They are made from safe polymers. They are used for major vascular bypasses.
When bypass surgery is performed on the vessels.
Bypass surgery on the lower extremities is strictly indicated for the following indications:
- Peripheral arterial aneurysms (enlargement of a vessel due to damage to its walls);
- Atherosclerosis of the veins (deposition of cholesterol deposits on the vascular walls);
- Chronic diseases with damage to the arteries of the lower limbs;
- varicose veins;
- thrombosis and thrombophlebitis;
- Primary manifestations of gangrene of the lower limbs;
- Ineffective drug treatment.
Lower extremity bypass surgery is not performed if:
- angioplasty is possible;
- The patient is completely paralyzed;
- poor test results;
- the function of individual organs is impaired.
Symptoms and diagnosis.
The symptoms of lower limb peripheral artery disease are easy to recognize in the early stages of the disease.
Those affected may complain of difficulty walking. Intermittent claudication is the most likely symptom of lower extremity arteritis. This phenomenon is characterized by pain in the affected person's calf muscles.
Those affected by arteritis of the lower extremities have a feeling of coldness in the legs and trophic ulcers appear. It is customary to divide the symptoms of the disease into different stages depending on the severity. Specialists distinguish four main stages in the development of arteritis of the lower limbs:
- Stage 1 of the disease is characterized by leg pain, sensitivity to cold, and frequent cramps. The patient feels burning, tingling sensations in the fingertips. He feels constantly tired and may have an aversion to work.
The extremities become pale in color and feel cold. Pain in the calf muscles becomes noticeable after intense physical activity. Pain often occurs in the thighs (if the femoral artery is affected), shins, feet, and knees. The stage of the disease can be determined using the 'walking test'.
- Stage 2 of obliterative atherosclerosis is called the subcompensation stage. The skin on the legs loses its elasticity and the pain in the limbs increases rapidly (especially after intense exertion). The patient's nails grow slower, become brittle and turn brown. It is important to respond appropriately to such symptoms and not to delay seeing a doctor.
In the affected areas of the legs, hair stops growing, muscle and tissue loss occurs in the foot, and the aorta no longer supplies the arteries of the limbs with the required amount of blood.
Treatment of lower limb arteriopathy
The information on this page is intended to help determine the symptoms and causes of narrowing of the veins or blood vessels in the legs. However, within the scope of this article it is not possible to present in detail all the treatment methods for the pathology in question.
The treatment options for leg osteoarthritis are diverse.
Treatment includes complete smoking cessation, a sparing diet, special health walks and taking medications.
Surgery can also be performed. Leg artery disease develops over a long period of time, year after year, bringing suffering and pain to people.
Pharmacotherapy consists in taking antiplatelet drugs (Aspirin-Cardio, Cardioagnil), which should always be available at home. The doctor should prescribe statins to combat the formation of atherosclerotic plaques. Some medications are used to lubricate the affected area. The medication should only be used on the recommendation of the vascular surgeon.
From stage 3 onwards, when leg pain becomes unbearable, surgical intervention is indicated. Through surgical intervention, the lumen of the extremity arteries can be expanded using a shunt. In critical cases, amputation of the affected organ is necessary because the patient is no longer able to endure the pain.
Endovascular therapy is used to expand the lumen of the artery. This therapy is very effective. A wire is inserted through a small hole in the artery, allowing a stent to be inserted to help expand blood flow.
symptoms
- Lameness localized to the hock;
- limb ischemia;
- incomprehensible pain, even at night;
- paresthesias;
- Chills;
- Cramps.
Further investigations show an abnormal reaction of the vessels to human movements (wall narrowing instead of dilation).
diagnosis
Obstruction of the iliac artery or femoral artery most commonly occurs in the legs. A vascular surgeon will tell you what it is and what first aid measures are needed for the body.
Prolonged vascular occlusion of the lower limbs has serious consequences for the body, up to amputation of the leg, so any suspicion requires a thorough examination in the hospital:
- The surgeon visually inspects the site of the suspected vascular occlusion and looks for swelling, dryness, and other skin changes.
- A vascular scan helps narrow down the affected sections.
- If the picture is unclear, an X-ray or angiography is prescribed, during which a contrast agent is injected into the artery.
- The ankle-brachial index helps assess the circulatory system.
What are eyeball implants made of?
The implants are made from biocompatible materials that are environmentally friendly and gentle on tissue. Production technology has now advanced so much that artificial eyes are as close to the real eye as possible. Patients have no concerns about how they look or feel.
During the rehabilitation period after removal of the eyeball, the patient must follow all the doctor's recommendations. The list of recommendations usually includes anti-inflammatory drops and taking medications with an antibiotic.
The rehabilitation period depends on the disease and the method used to remove the eyeball. If the implant shifts, further surgery may be necessary. To avoid this, it is important to follow all the recommendations of your ophthalmologist, pay attention to physical activity during the rehabilitation period and take all necessary medications.
Complications of enucleation
In addition to the displacement of the implant that may occur after surgery, the procedure can also cause other complications: ptosis of the upper eyelid, drooping of the lower eyelid, poor mobility of the eye prosthesis. The good news is that these inconveniences can be corrected.
Read more:It should be added that enucleation is not performed if there is a high risk of infection, purulent encephalitis. The doctor takes into account the objective data about the patient's condition before carrying out the operation.
- incision on the leg.
- The reamputation is.
- Hip Amputation Surgery Code.
- Where amputated limbs go.
- The bone where the ankle is located.
- stump care.
- Plastic amputation of the tibia according to Pirogov.
- X-ray of the foot.
