In 25 % cases, the cause of tarsal tunnel syndrome remains unknown. It is a painful but treatable condition. However, sometimes it has more serious consequences, such as loss of sensation or joint mobility.

- Tarsal tunnel syndrome
- What is the tarsal canal of the foot?
- causes
- What diagnosis is required?
- causes
- Interesting facts.
- Treatment
- rehabilitation
- Rehabilitation after conservative treatment
- Rehabilitation after surgery
- Treatment techniques for SCT
- Costs
- Symptoms and diagnosis of tarsal tunnel syndrome
- Conservative treatment of tarsal tunnel syndrome
- Causes of tarsal tunnel syndrome
- Symptoms of tunnel foot syndrome
- Treatment of tarsal tunnel syndrome
- surgical treatment
Tarsal tunnel syndrome

Pain in the ankle and ankle joint area is often a sign of destructive pathological changes, which, as a result of scarring, can lead to a serious complication - tibial nerve neuropathy. This condition is called tarsal tunnel syndrome and tarsal tunnel syndrome. The clinical diagnosis of this disease is difficult because, due to the long period in which the symptoms appear, it is not possible to associate the ankle injury with the subsequent negative manifestations. Therefore, many doctors are inexperienced in diagnosing and treating the pathology of the joint itself (arthritis, osteoarthritis, plantar fasciitis, etc.). In reality, the pain is caused by damage to the tibial nerve and its trophic disorder. It loses the ability to fully innervate the soft tissues of the foot. This leads to pain, stiffness, poor blood supply and other negative symptoms of the disease.
Tarsal tunnel syndrome is a pathology that develops as a result of increased internal pressure in the tarsal tunnel. An obstacle arises in the tarsal region that puts pressure on the tibial nerve that runs there. As a result of the sustained pressure and ischemia, the nerve fiber begins to lose function. The patient experiences pain, a burning sensation in the foot area and limited mobility in some of the toes. In the early stages, the unpleasant symptoms only appear after prolonged exposure. Later, when the ear canal narrows, pain and burning may occur even when walking short distances.
These symptoms often prevent a correct diagnosis from being made in a timely manner. The patient is told that a heel spur has formed, so symptomatic nonsteroidal anti-inflammatory drugs should be used to relieve pain. Only shockwave therapy can help. In reality this is not the case. Rather, persistent neuropathy of the tibial nerve leads to destructive changes in the area of the talus and heel bone. This can promote the appearance of heel spurs. However, if medical attention is sought in a timely manner in this situation, the development of this condition can be avoided.
What is the tarsal canal of the foot?
First, we need to understand what the tarsal canal is and where it is located. The tarsal nerve is a branch of the sciatic nerve that branches in the cervical fossa. The tarsal canal of the foot is located on the inner (medial) side of the ankle joint. It is formed by the flexor tunnel (a structure made of dense fibrous tissue). Inside the tunnel there are blood vessels and nerve fibers. It arises from the plantar part of the foot. Another name is Richet's heel canal.
Tarsal tunnel syndrome of the foot can arise both from a pathological deformation of the internal tissues and from the pressure exerted by the heel, talus, deformed tendons, scars, etc. The malposition of the foot and the valgus deformity (X-shaped) of the lower limbs are of great importance in the development of this pathology.
With a comprehensive treatment approach, it is possible to determine the possible cause. The doctor does everything necessary to eliminate the negative effects.
causes
A large proportion of cases (around 30-40 %) have idiopathic causes; Other triggers for tarsal tunnel syndrome include:

– Frequent and prolonged stress in the vicinity of the tibial nerve canal – standing, running, prolonged walking;
– Trauma – sprains, broken bones, dislocations;
– overweight;
– A valgus or labral heel;
– fibrosis;
– Tendonitis;
– Tarsal abnormalities – osteophytes, edema, swelling, varicose veins;
– systemic diseases that cause inflammation of the ankle joint or impair its innervation – arthritis, diabetes.
What diagnosis is required?
The diagnosis is made based on the clinical picture, medical history and physical examination. The characteristic diagnostic sign of tarsal tunnel syndrome is a feeling of shooting through the nerve when felt with the finger at the level of compression.
– Blood sugar test to rule out hyperglycemia;
– EMG, ENMG – to detect nerve conduction abnormalities;
– X-rays – to assess the condition of the phalanges (no wear) and to determine whether there is a fracture or not;
– MRI of the joint – is an important test to rule out soft tissue tumors in the foot.
The Kurska Health Clinic has all the equipment necessary for diagnosis. Above all, a state-of-the-art MRI machine.
causes
The development of tarsal tunnel syndrome is triggered by various causes and processes.
- Trauma. This is the most common cause. Tarsal tunnel syndrome usually occurs after sprains, fractures of the inner part of the ankle, talus, or heel bone. All of these diseases lead to thickening of the annular ligament and resulting compression.
- Overload. This is caused by repetitive movements in the ankle area, both during daily activities and during sports.
- Foot defects. Flat foot creates biomechanical abnormalities that cause stretching of the internal structures and cause tarsal tunnel syndrome.
- Inflammatory processes. Particularly tenosynovitis of the flexor tendons or the posterior tibial plateau.
- Diseases of the tendons or veins. Varicose veins can put pressure on the nerves. Another factor may be a cyst on a tendon.
- Systemic diseases. Occur in about 10 % cases. The most commonly affected diseases: diabetes, arthritis, hyperthyroidism, hyperlipidemia.
- No clear cause. In 25 % cases the cause of tarsal tunnel syndrome is unknown.
Interesting facts.
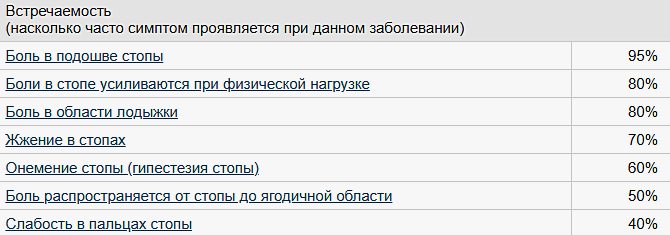
The main symptom of tarsal tunnel syndrome is pain in the foot. It is localized around the ankle, almost always somewhere in the middle. The discomfort spreads to the toes and worsens when walking. In later stages, the pain persists even at rest.
The pain is a burning sensation, usually accompanied by a tingling or cramping sensation. Initially they are only noticeable when standing, walking or wearing certain shoes. The pain most often occurs at night, after an active day. They can be partially relieved by moving the ankle, foot, or the entire leg.
A feeling of numbness and weakness in the muscles of the foot, toes, or ankles is also common. In the most severe cases, this weakness is noticeable and can lead to foot deformities.
With appropriate treatment, complete healing is possible. Only a minority of those affected experience consequences such as partial or complete loss of feeling or mobility. It should also be noted that the condition recurs in a small percentage of patients.Published by econet.co.uk
PS And remember: just change your mind - together we change the world! © econet
Did you like this article? Write your opinion in the comments.
Subscribe to us on FB:
Treatment
Tarsal tunnel syndrome can be managed with a wide range of treatments. Regardless of the underlying condition, however, it is important to seek early treatment to prevent irreversible nerve damage. Anti-inflammatory medications can be taken at home to reduce inflammation. Rest, cooling and compression reduce swelling and inflammation.
Steroid injections may be given to the affected area to reduce swelling. In some cases, splints are used to immobilize the foot and limit movements that compress the nerve. For naturally flat feet, special shoes can be ordered to support the arch of the foot. In severe, chronic cases, the neurologist recommends surgery in which the surgeon makes an incision from the ankle to the arch of the foot to release the ligament. Some surgeons also use minimally invasive procedures that involve making much smaller incisions in the ankle. The surgeon uses instruments to stretch the ligament. Because there is less injury to the tissue, the risk of complications and recovery time are lower.
rehabilitation
Rehabilitation after conservative treatment

As soon as conservative therapy is prescribed, improvement can occur within a few days. Anti-inflammatory medications are usually prescribed for up to 10 days. To achieve a lasting treatment effect, spinal orthoses should be used for several months.
A physical therapist will develop specific exercises to maintain muscle tone, particularly for the muscles that support the arch of the foot.
Physiotherapy is recommended by the physiotherapist. The treatment aims to reduce pain and, above all, swelling. In addition to pure physiotherapy, physiotherapy can also be prescribed together with anti-inflammatory ointments.
Rehabilitation after surgery
Pain is usually reduced immediately after surgery, although some pain in the area of the surgical wound may persist for many months.
In the postoperative period after surgery, swelling of the ankle and foot may occur. To prevent swelling, do not lift your leg out of bed often and stay in an upright position. If the swelling has progressed, the leg can be elevated by placing it on a pillow.
The bandages are applied according to the doctor's instructions. The stitches are removed on days 10-14. The surgeon may recommend the use of a cast or plastic splint and crutches for up to 10 days to promote healing of the surgical wound.
After stitch removal and immobilization, more active exercises are recommended to restore tone to the muscles that support the arch of the foot. The load and difficulty of the exercises are gradually increased. During the exercises, pronation of the foot must be avoided, i.e. there should be no tension in the area of the surgical wound. The main goal of the exercises is to imitate everyday activities such as walking, standing on tiptoes, and climbing and descending stairs.
Treatment techniques for SCT
If any type of mass contributing to the development of SCT is detected in a patient, professionals recommend its immediate surgical removal. In cases where no such masses are present, the patient is treated primarily conservatively.
The main goal of eliminating the defect by conservative methods is to reduce the pulling effect on the various anatomical elements of the foot (including the nerve).
- Using specially selected regular or orthopedic shoes and insoles to distribute the load on the foot as evenly as possible;
- reducing obesity;
- Physiotherapeutic treatments and exercises;
- Restriction of certain motor functions;
- Topical administration of corticosteroids to temporarily reduce swelling and many others.
In cases where conservative treatment is ineffective, surgery is indicated.
Surgical treatment of the vagus nerve is rarely recommended and, as mentioned above, is indicated when cysts, benign tumors, and other types of masses are present that compress the nerve.
During such operations on the tarsal canal, the specialist performs an excision of the vagus volaris to expose the nerve as well as its branches in the adjacent areas.
Costs
Initial visit to the specialist’s office
- Recording the history of the disease (anamnesis), determining the patient's main complaints, etc.
- Clinical examination
- Symptoms of the disease
- Examination of hematological findings, X-ray data (ultrasound, MRI, CT)
- diagnosis
- Treatment visit
Repeat visit to the specialist's office
- Analysis of the results of the diagnosis made at the first visit to the specialist's office
- Clarification (refinement) of the diagnosis
- prescription of treatment
Blockage (without costs for dipropane)
- Consultation visit
- Blood draw
- Collection of platelet-rich plasma
- Injection of the obtained plasma into the affected area
Arthroscopic surgery for tarsal sinus syndrome
- stay in the clinic
- Application of epidural anesthesia
- Arthroscopic surgery
- Consumables (surgical material)
- Clinical examination and plantoscopy
- Making shoe insoles
- consumables
- Advice on preventing ankle and foot diseases
Postoperative visit to the doctor's office
- Postoperative clinical examination
- Postoperative X-ray, MRI and CT findings
- Advice on rehabilitation
- Intra-articular injection of hyaluronic acid (if necessary)
- Removal of surgical stitches
Symptoms and diagnosis of tarsal tunnel syndrome
Symptoms of tarsal tunnel syndrome include pain in the back of the ankle, plantar tingling, and a burning sensation in the toes. The patient has an altered gait, deformity of the toes, and muscle dysfunction in the foot. In advanced cases, this can lead to muscle loss.

During the examination, the doctor looks at the condition of the ankle joint. An MRI scan is performed to determine whether the person has other medical conditions. If there are bony protrusions or osteophytes, x-rays are taken.
Conservative treatment of tarsal tunnel syndrome
Treatment for tarsal tunnel syndrome depends directly on the cause of the symptoms. Non-steroidal anti-inflammatory drugs or glucocorticosteroid injections (dexamethasone, dipropane) are usually used for conservative treatment of tarsal tunnel syndrome. These relieve swelling and reduce compression of the posterior tibial nerve. The pain subsides when lying down, so bed rest is recommended.
Orthopedic shoes are prescribed to limit movement of the foot and not worsen symptoms. Doctors who treat this syndrome include neurologists, podiatrists, osteopaths, rheumatologists, traumatologists and rehabilitation therapists.

Laser therapy is used to improve the biochemical processes in the body. It renews the tissue, regenerates its activity and activates the self-regulation mechanisms. Magnetic therapy is also used to stimulate blood flow to tissues and relieve pain.
In addition, conservative treatment uses ultrasound therapy and physiotherapy such as phonophoresis, electrophoresis and UHF therapy.
Causes of tarsal tunnel syndrome
Causes can include varicose veins surrounding the nerve, tendinitis (tendonitis), bone or soft tissue tumors such as lipomas or fibromas.
Occasionally, nerve compression is caused by soft tissue swelling resulting from trauma (such as ankle ligament injuries or ankle fractures) or from diseases such as diabetes or rheumatoid arthritis.
Another common cause of tarsal tunnel syndrome is flatfoot, a valgus deformity of the foot. As a result of the flattening of the arch of the foot, the heel moves outward and pulls on the posterior tibial nerve, which is compressed in the tarsal tunnel. Tarsal tunnel syndrome is very similar to carpal tunnel syndrome in the hand.

Symptoms of tunnel foot syndrome
If a person develops tunnel foot syndrome, they may experience tingling, burning, or numbness in the medial ankle area, which may spread to the inside of the foot. It often feels like you are standing on high heels and can cause stabbing pain that feels like an electric shock.
As the pain progresses, it spreads from the heel to the buttocks and increases when the foot is flexed.
The pain usually increases during the day as tension increases and is relieved by resting at home in the evening, watching TV with feet elevated, and light massage. Then the pain, burning, numbness and tingling in the foot stops and often occurs at night. Weakness develops in the toes and walking on tiptoes is impossible.
The symptoms of tarsal tunnel can occur with increased physical exertion (sports) or prolonged static stress (leg work, long walks). If the above symptoms occur, you should not delay seeing a doctor. If symptoms persist over a long period of time, permanent damage to the nerve may occur.
Treatment of tarsal tunnel syndrome
When treating tarsal tunnel syndrome, a distinction is made between conservative and surgical treatment. Except for acute cases, surgical treatment should be performed when conservative methods are not effective.
Conservative treatment depends on the underlying cause of the syndrome.
The most effective treatment for biomechanical causes of tarsal tunnel syndrome is to choose comfortable footwear and use orthotics that support neutral foot position. And for tendonitis, a local corticosteroid injection should be given. In conservative treatment, stabilization of the leg, bandages and varus stockings, ice packs, special exercises to reduce pressure in the canal and relax the nerve, as well as muscle-strengthening exercise programs are important.

The illustration shows the location of numbness and compression of the tibial nerve in tarsal tunnel syndrome.
surgical treatment
Surgical treatment is recommended if a mass or foreign body is found compressing the tibial nerve in the tarsal tunnel cavity. Only after three months of unsuccessful conservative treatment can surgical treatment be considered. Some authors report that this period can be extended to six months. The Lamin technique is usually used during the operation. This technique involves making an oblique incision that runs through the posterior surface of the medial malleolus to its center. This incision opens the deep fascia above the flexor muscles. The aim of this operation is to expose the upper and lower areas of the tarsal tunnel. In the lower area, the canals above the adductors of the first toe must be loosened by about 3 cm, as the lateral and metatarsal branches of the tibial nerve run through them. The fibular ligaments, if present, should also be severed and the inner heel area secured. Failure to pay attention to the anatomy of this area can result in unsatisfactory decompression and recurrence of symptoms.

The figure shows the incision of the flexor muscle sheath in which the tibial nerve is located
The operation can be performed under general anesthesia, local anesthesia, or light anesthesia. A tourniquet used during surgery to stop bleeding is not recommended in this case. Different surgical techniques have been described in idiopathic cases: incision of only the flexor muscle sheath and exposure of the canal; Posterior tibial nerve dissection; arterial and venous relaxation.
If the surgical results are unsatisfactory, MRI is the most valuable diagnostic method. The literature recommends reoperative tarsal tunnel loosening if the first attempt fails. The result of reoperation is significantly better if there is no thickening of the supraspinatus nerve. In Campbell reoperation, a superficial ear vein graft shows signs of thickening of the supraspinatus and a reduction in the number of reoperations.
Read more:- Tarsal Tunnel Syndrome.
- The tarsal of the foot.
- The tarsal and metatarsal bones.
- tarsus.
- tarsus.
- tarsal and metatarsal joints.
- pain in the tarsus.
- Tibialis posterior muscle.
