Doctors will order additional tests if necessary.
- tarsal foot
- functions of the foot
- Causes of foot deformities
- Types of foot deformities
- diagnosis
- Which doctor treats?
- Osteosynthesis of the metatarsal bones and phalanges of the foot in the surgery center of the SM Clinic
- prevention
- What questions should you ask your doctor?
- Tips for the patient
- Features of the foot: bones, ligaments and tendons
- foot injuries
- Application of massage therapy
- Additional recommendations.
- ICD-10 codes
- Clubfoot in dystrophic dysplasia
- Treatment
- Fractures of the fifth metatarsal bone
- Fractures of the base of the 5th metatarsal
- Treatment
tarsal foot
The foot is a complex and very important part of the entire human skeleton. It consists of 26 bones, 107 ligaments and 20 different muscles and tendons. The foot is the 'foundation' of the body and carries the load of the entire body during movement.
The foot is made up of the bones that form its base (skeleton), the ligaments that move and connect the bones together at their joints, the muscles that move the foot, the blood vessels that carry the blood, the nerves that allow the muscles to work, and the skin that covers the foot.
The foot skeleton is divided into three parts: the tarsal bone, the metatarsal bone and the intermediate phalanges of the toes.
The most prominent points of the toe phalanges are called the toe arches.
The bottom of the foot is called the plantar surface and the top is called the dorsal surface.
The foot is supported at 3 points:
The foot has an arched structure. A distinction is usually made between two longitudinal vaults and one transverse vault.
The AC is the inner longitudinal arch (elastic);
Behind the metatarsals, in front of the toes, is the widest part of the forefoot, formed by the heads of the metatarsal and toe joints and called the transverse arch (AC arch).
– The inner arch (elastic) is formed by the heel, the talus, the scaphoid, the three sphenoid bones, the 1st, 2nd and 3rd metatarsals and is an arch running through the entire foot, which starts from the calcaneal tuberosity and is at the contact point of the head of 1;
These bones form a kind of arch, a spring, that can flatten and spread.
– The outer arch (load arch) is formed by the heel, the plumb line, the 4th and 5th metatarsal bones, also in the form of an arch that runs through the entire foot, starts from the heel bone tuberosity and reaches the support point of the head of the 5th metatarsal.
The transverse arch is perpendicular to the longitudinal arches over the metatarsal bones.
The arches of the foot can only be considered as separate elements, since in reality they are in constant interaction and function as a single mechanism.
functions of the foot
The main function of the foot is to provide support and support movement for the human body when standing.
The foot fulfilled three biomechanical functionsThree biomechanical functions: elastic, balancing and supporting.
function of shock absorption – Shock absorption when walking, running and jumping. It is made possible by the ability of the foot to cushion itself under stress and return to its original position. A foot cushioned from the front, outside and inside is able to change shape and move in three planes, like a boat on the waves of the sea, as the total load and the shape of the supporting surface change direction. This is important to absorb small unevenness in the floor.
When the arch of the foot is lowered, the tremor is transmitted more strongly to the joints of the lower limbs, the spine and internal organs, leading to impairment of their function, microinjuries and dislocations.
equilibrium function – Posture control during movement. It is realized by the ability to move the joints of the foot in three planes and by the wealth of receptors in the ligaments. A healthy foot digs out unevenness and people feel what surface they are walking on. If the bones and joints are realigned, the ligaments become deformed, so that movement coordination and stability suffer.
B support function manifests itself in the ability of the foot to provide support to the human body by counteracting the vertical load caused by body weight.
This is the foot's most complex function, as it uses both elasticity and balance.
All three functions of the foot are carried out one after the other when walking.
When the arch of the foot is lowered, all functions of the foot are impaired.
| The foot must be viewed in the 'foot - lower extremity - spine' system. In the supporting structures of the body, each upper joint depends on the lower one and vice versa. Foot diseases cause asymmetries throughout the body. The figure shows the most important positional abnormalities in flat feet. The flattening of the foot leads to a cascade of compensatory changes and overloads in the lower limbs, pelvis and spine. As the foot flattens and deviates outward, this results in external rotation of the tibia and compensatory internal rotation of the thigh. This reinforces the X-shape of the knees. On the other hand, aligning the upper body in relation to the foot can improve the arch of the foot. The foot plays an important role in developing posture. | 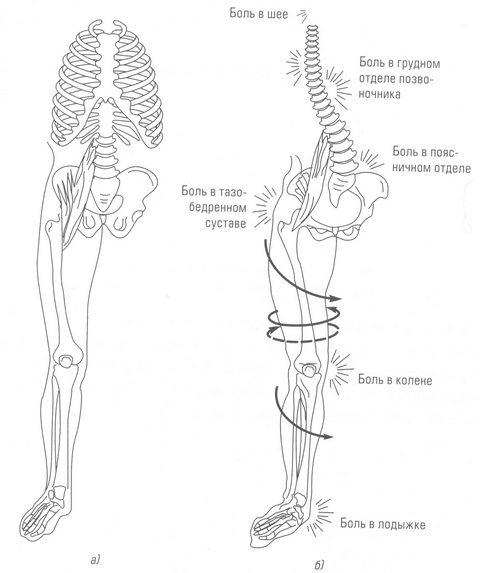 | |
| Changes in the upper body with foot deformities: | ||
| (a) normal foot | (b) Foot deformity | |
Causes of foot deformities
- traumatization
- overweight
- Connective tissue dysplasia
- Vitamin and mineral deficiencies
- Developmental abnormalities
- neurological disorders, brain damage
- destructive-dystrophic and autoimmune diseases (osteoarthritis, rheumatoid arthritis)
- metabolic disorders
- long-term immobilization
- genetic factors
- Posture damage.
The severity of clinical symptoms varies depending on the type of deformity and its cause: from mild discomfort when walking to claudication, persistent pain.
- Stiffness of the affected joints, redness of the skin over the inflamed area, swelling
- Pain syndrome
- Lameness, 'strange' gait
- a noticeable deformation - patients refer to it as a 'bump' - on the inside of the foot or big toe
- Changes in the shape of the foot
Deformities can affect the entire foot or be limited to a specific area of the foot, namely the toes.
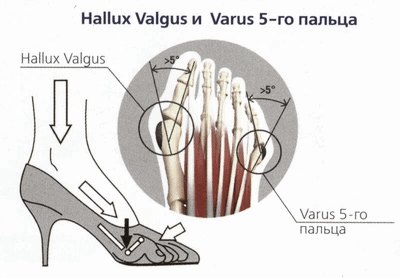
When wearing uncomfortable, tight shoes, constant trauma and pressure, the big toe moves inward and the joint at its base protrudes outward.
Claw-shaped deformation - the toes point downward, like a bird's claws.
Each type of inflammation goes through three stages - initially mild, exudative-tropic and chronic.
Types of foot deformities
Foot deformities can be caused by a single defect or multiple abnormalities.
In orthopedics and traumatology we can classify deformities:
Varus deformity – flattening of the feet and their 'bending' inwards.
Valgus deformity – the metatarsal bone is depressed, the heel is turned outward, and the inner edge is also depressed.
Abnormally high arch of the foot – occurs in one or both feet and causes significant pressure on the foot or heel when walking or standing. Pes cavus usually occurs against the background of an underlying neurological disease.
Clubfoot – The inner edge of the sole bends upward and inward from the long axis of the shinbone, the metatarsal bones pull apart and the foot becomes wider.
Flat feet – Flat feet are the most common pathology in which the arch of the foot is flattened on the inside, which has its origins in childhood. Flat feet can be longitudinal or transverse.
Longitudinal flatfoot occurs due to fetal malposition and sustained compression of the limbs and is characterized by a dorsiflexion position.
Equinus foot (equinus) – the foot points downward and the heel cannot be lowered to the ground due to shortening of the calf muscles. People with this deformity can only walk and stand on the forefoot and midfoot and are unable to roll smoothly from heel to toe.
diagnosis
If you feel very uncomfortable when walking, your feet tire quickly in your shoes, or you experience burning and itching, you should see an orthopedist. He or she will examine your feet and make a diagnosis. Before seeing a specialist, you can self-diagnose online by taking the self-diagnosis test on our website. This allows you to quickly assess any risks and recognize the severity of the problem.
During a direct examination by the doctor, the patient can receive recommendations:
| diagnostic methods | Time |
|---|---|
| X-ray of the foot | 10 mins |
| Blood and urine test | 10 mins |
| Foot ultrasound | 30 minutes |
| Computed tomography of the feet | 20 minutes |
| Magnetic resonance imaging of the feet | 20 minutes |
All of these methods help to understand why foot pain occurs and what causes it. As a rule, the doctor requires only a few procedures, so the cost of diagnosis rarely exceeds 5-6 thousand rubles.
Which doctor treats?
If you have pain in the sole of your foot, you should consult a doctor with the following specialization:
The prices listed on this page are not a public offer. Please call 8 (495) 255-37-37 for an estimate and to schedule an appointment.
Osteosynthesis of the metatarsal bones and phalanges of the foot in the surgery center of the SM Clinic
Spica osteosynthesis prevents recurring dislocations of bone fragments, which is particularly important for the 1st and 5th metatarsals and the associated toes. The patient is able to move the leg faster, which prevents muscle wasting and other problems.
After osteosynthesis, the patient remains in the clinic for 1-3 days, depending on the complexity of the procedure. After discharge, it is important to follow the doctor's instructions regarding medication and exercise. The leg should not be put under any weight until the bone has completely healed, as determined by x-rays. During the recovery period, the patient is prescribed massage and physical treatments, and in some cases, physiotherapy to speed up healing. Regular check-ups and follow-ups are also mandatory.
If you have any questions about foot osteosynthesis, please call the SM Clinic surgery center or leave a callback request on the website. The contact center specialists will answer all your questions and help you make an appointment if necessary.
prevention
The best way to prevent foot bone fractures is to follow workplace safety rules and avoid injuries at home and in the gym.
What questions should you ask your doctor?
How do you provide first aid if you suspect a broken foot?
Which diagnostic methods are the most informative?
What are the risks associated with a foot bone fracture?
Tips for the patient
All broken bones require medical treatment. The doctor will select the appropriate treatment tactics. Callus formation begins quite quickly, so you should not delay a visit to the doctor.
Features of the foot: bones, ligaments and tendons

The complete adult skeleton consists of 205 to 208 bones, 52 of which are in the foot - 26 in each foot. The bones of the tarsus (which end in the phalanges of the toes) form the convex arch of the foot; If this is missing or insufficiently pronounced, it is referred to as a flat foot. The structure of the foot of a healthy person is most pronounced in an adult, slender man, weaker in a young woman and practically absent in a child.
The tarsal foot consists of 7 bones that form a complex three-dimensional volumetric puzzle that provides the human body with stability during a variety of movements. There are a total of 20 joints in the foot, providing 24 degrees of mobility.
foot injuries
You cannot be immune to foot injuries. All you have to do is go outside and look under your feet. Spring is just around the corner, and it is becoming more and more common to find a thin layer of ice on the sidewalk in the morning and a crumb of water and ice in the evening that freezes again overnight. Another traditional place for injuries is the gym. It doesn't matter whether it's running, martial arts, acrobatics or dance. – The risk of injury is everywhere. After all, spring and summer are just around the corner - a time when thousands of people rush out of the city and on all sorts of trips. And if instead of smooth asphalt there is an unpredictable path or a rocky embankment under your feet, the risk of a foot injury increases many times over.
The most common injuries are the Achilles tendon (partial or complete tear) and the lateral and medial ligaments of the ankle. Fractures are less common, but they are often difficult to detect, especially on the foot. There have been cases where people have suffered phalangeal and metatarsal fractures but thought it was a sprain or bruise and did not seek medical attention. Only later did it become apparent that other treatment was required. A common type of these injuries is what is known as a stress fracture or stress fracture. At risk are older people in whom the process of bone destruction has already begun, summer hikers who have spent the whole year in front of the TV, fitness novices who do not know how to choose the right training shoes, etc.

X-rays show disorders of bone integrity, that is, fractures. Ligament sprains and tears, on the other hand, cannot be detected on an X-ray; This requires an MRI or ultrasound. There are also a number of special tests that a traumatologist can use to determine the nature of the injury.
The most common injury is an inward twisting of the foot.
The first symptom of a foot injury is pain. The second is swelling that usually spreads to the ankles and rear foot, where the tendon sheaths of the foot are also damaged by the injury. Swelling may develop more quickly in the case of a fracture and gradually in the case of a partial tear or dislocation. Massive hematomas on the foot can occur.
Application of massage therapy
Physiotherapy treatment can be combined with massage therapy.
Massage as a rehabilitation measure after a severe fracture of the 5th metatarsal bone is extremely useful and helps the foot recover faster. The most common type of massage is traditional massage or water massage.
Not everyone is able to attend a massage course in a specialized place, so massage can be done at home. The most important thing is that it is carried out gently and carefully.
- The foot is massaged with gentle circular movements, applying gentle pressure to the injured area.
- Tingling, stroking and kneading should also be carried out.
- The entire foot (outer and inner part) and toes should be kneaded.
After the massage, it is advisable to do a foot bath with herbs and sea salt. It helps to relieve tension in the limbs and relaxes. Water up to 40 degrees warm is recommended.
Danger!!! A massage combined with a foot bath can relieve swelling and pain, accelerate tissue regeneration and improve mobility of the feet.
The massage is used to develop the foot and improves blood circulation in the foot. The damaged tissue begins to be supplied with high-quality nutrients.
Additional recommendations.
If such a fracture occurs, flat feet may occur in the future.
After the injury, it is necessary to strictly follow the doctor's instructions. When rehabilitating after a metatarsal fracture, you should choose the right footwear.
- Do not wear high-heeled shoes, flat-soled summer shoes, or pumps.
- The shoes should be the right size, comfortable and firm, but not constricting. Comfort, natural, high-quality materials come first. Heel – up to 4 cm.
- You should wear orthopedic shoes where the sole is rigid. They can also attract supinators. Orthoses adequately cushion the foot when walking and protect against various complications. Before purchasing insoles, consult your doctor.
- Walk with extreme caution after an injury. The heel and over time the entire foot is used as support.
- Sometimes an elastic bandage is also prescribed.
- Swimming and water aerobics are also helpful.
- Swelling in the leg can be treated with Troxevasin or Lyoton 1000 ointment.
In addition to physical treatments, a nutrient-rich diet is also necessary to strengthen the bones. A natural, wholesome diet rich in calcium (e.g. dairy products), various vitamins and minerals should be consumed daily.
Average rating: 4.3 / 5. Number of reviews: 207
There are no reviews available. Be the first to write a review.
ICD-10 codes
- Q77.5 Dystrophic dysplasia.
- Q77.7 Spondyloepiphyseal dysplasia.
- Q77.8 Other osteochondrodysplasias with growth disorders of the long bones and spine.
- Q77.9 Osteochondrodysplasia with growth disorders of long bones and spine, unspecified.
- Q79.6 Ehlers-Danlos syndrome.
In multiple epiphyseal dysplasias, pseudoachondroplasias and late spondyloepiphyseal dysplasias, congenital functionally significant deformities are rare.
With increasing age, the contractures caused by deformative osteoarthritis of the ankles and feet worsen, valgus or supination deformities occur, and epiphyseal flattening progresses. Conservative treatment includes massage, physical therapy, physiotherapy, osteoarthritis medications, orthotics and orthopedic shoes. Surgical treatment is indicated for persistent deformities that lead to functional limitations.
In Ehlers-Danlos syndrome, Larsen syndrome, congenital spondyloepimetaphyseal dysplasia, congenital spondyloepiphyseal dysplasia and dystrophic dysplasia, most patients have congenital foot deformities. These tend to be stiffer and more pronounced than in isolated orthopedic pathologies. Their common feature is progressive bony deformities. The frequency of dislocations and subluxations of the ankle joints is high, and in epiphyseal dysplasia there is flattening of the epiphyses. Acute osteoporosis, degenerative-dystrophic changes, which increase rapidly with immobilization and the use of Ilizarov braces, are typical. An atypical attachment of the tibialis anterior muscle tendon to the diaphysis of the first metatarsal, provoking the development of anterior insertion recurrence, was noted in 30 % or more of the patients. However, the phenotypic polymorphism of ASD is extremely broad, and there are children with minimal or no clinical signs of foot deformity. Deformities in different SODAs differ significantly not only from non-systemic deformities, but also from each other and require different treatment approaches. The focus is on restoring the supporting function of the foot and not on restoring the disturbed anatomical conditions and functions.
Clubfoot in dystrophic dysplasia
- The ankle joint foramen is underdeveloped and its size does not correspond to the size of the talus (Fig. 110-9).
- Anterior subluxation (dislocation) of the ankle joint.
- Additive sphenoid bones, additional ossification nuclei; Enlargement and deformation of the sphenoid bone I.
- Dislocation of the tarsal joint I (up to 30 %).
- Varus foot, which is caused not only by subluxation of the Schopar and Lisfranc joints, but also by progressive varus deformation of the metatarsal diaphysis with wear and tear.
- Delta-shaped deformation of the first metatarsal bone, thickening of the proximal phalanx of the first toe.
- Brachyphalangy, symphalangy and clinodactyly.
- Subluxations and dislocations of the metatarsophalangeal joints occur and progress with age.
Treatment
Conservative treatment of severe deformity is ineffective. The thallium in the foramen of the ankle joint cannot be preserved, and the dislocation of the first metatarsophalangeal joint cannot be reduced. Aseptic necrosis of the femur is common when using step casts.
For relatively mild deformities, an early tenoligamentocapsulotomy with mandatory dislocation of the metatarsophalangeal joint I of the big toe, simulated resection of the oblique articular surface of the ischium I and displacement of the tibialis anterior tendon is indicated. For more severe deformities, tenoligamentocapsulotomy must be combined with the use of an Ilizarov brace, extending the possibility up to 2-2.5 years of age. Severe bony deformities require early resection of the foot. Postoperative immobilization takes place in a 15-20° hypercorrection position. For anterior dislocation of the ankle and talar deformity, early astragalectomy is the operation of choice. Corrective lavaloplasty of the ligament on the outside of the foot is indicated in all cases to prevent recurrence. From the age of 9-10 years, early arthrodesis of the subtalar and chopar joints is indicated.
Fractures of the fifth metatarsal bone
MD, University of California, San Francisco
Fractures of the V metatarsal bone can occur at its base or shaft (diaphysis). Diaphyseal fractures can be acute fractures or stress fractures. Because the treatment and prognosis of these fractures vary widely, an accurate diagnosis is important. The diagnosis is made radiologically. Treatment depends on the location of the fracture.
Pain, swelling, and tenderness on palpation are usually found at the exact point of the fracture.
The diagnosis of a fracture of the 5th metatarsal is made based on x-ray images of the foot in anteroposterior, lateral and oblique projections.
Fractures of the base of the 5th metatarsal
Fractures of the base of this bone are sometimes called dancer's fractures or pseudo-Jones fractures. Its mechanism is usually due to a crush injury or a tangential force pulling the tendon away from the fibula muscle. These fractures occur more frequently than acute diaphyseal fractures (Jones fractures).
Since the stalk, in contrast to the diaphysis, has an abundant peripheral blood supply, healing delays and healing disorders are rare.
Treatment
Treatment of fifth metatarsal fractures is symptomatic and may include wearing rigid-soled shoes or an orthosis and weight-bearing as tolerated.
Copyright © 2023 Merck & Co, Inc, Rahway, NJ, USA and its subsidiaries. All rights reserved.
Read more:- tarsal and metatarsal joints.
- The tarsal and metatarsal bones.
- tarsus.
- The tarsal of the foot.
- tarsus.
- pain in the tarsus.
- Metatarsal tarsal bones.
- Massage for flat feet.
