Electroneuromyography (ENMG) of the lower limbs is used as an adjunct to the examination: the problem is indicated by a decrease in the pulse speed of the sensory fibers behind the medial malleolus.

- tunnel syndrome
- causes
- Definition of the disease. causes
- Symptoms of tarsal tunnel syndrome
- complications
- Treatment
- treatment methods
- Results
- Diagnosis of carpal tunnel syndrome
- Treatment of carpal tunnel syndrome
- What is the tarsal canal in the foot?
- Causes of tarsal tunnel syndrome in the ankle
- RISK FACTORS AND PREVENTION
- Treatment of tarsal tunnel syndrome
- What can I do if I have leg pain?
- classification
- diagnosis
tunnel syndrome
For people who do the same job for a long time, e.g. For example, if you sit at the computer for a long time, you may experience pain in your hands. This is then a tunnel syndrome. Not only people who work on computers, but also drivers can be affected by this problem because their hands are in the same position for a long time.
Tunnel syndrome is caused by the tissue around the tendon swelling, putting pressure on the nerve. This causes the patient to experience tingling in the hand and numbness in the fingers. The muscles become weak and the fingers may swell.
Carpal tunnel syndrome is related to the tunnel that runs between the transverse ligament and the bones of the wrist. The median nerve is located in the center of the carpal tunnel. Any disease, injury or pathology causes narrowing of the canal and affects the nerve, resulting in the syndrome.
causes
Tunnel nerve syndrome is both a congenital anomaly and a disease related to a person's activities and lifestyle.
The main causes of tunnel joint syndrome include:
- Adopting an awkward hand position for a long time (this may be related to professional activities, such as working on a machine);
- genetic predisposition;
- Hormonal imbalance due to pregnancy and menopause;
- Inflammatory processes;
- Benign, malignant tumors in the area of the ear canals.
Causes of tunnel syndrome include diseases such as osteoarthritis, diabetes, arthritis and thyroid disease. This problem can occur in patients with metabolic disorders, after bone fractures, frequent trauma or bruises.
Definition of the disease. causes
Tarsal syndromeThe tarsal syndrome (tarsal.) canalicular – is a peripheral mononeuropathy of the lower limbs caused by compression of the tibial nerve, causing pain in the ankle joint on the inside of the foot.

There are several other names for this pathology: tibial nerve entrapment syndrome, Richet's canal syndrome, tarsal canal syndrome. [9]
The onset of compression is independent of age and gender, since most cases are associated with trauma to the ankle joint or with subclinical and then decompensated neuropathy.
Nerve compression can occur for various reasons:
- valgus deformity of the foot;
- Soft tissue tumors – sarcomas of muscle, fat and tendons;
- Tumors of the nerve and its covering;
- vascular pathology (varicose veins);
- benign bony formations in the tarsal tunnel (exostoses);
- Trauma to the joint or muscles as a result of inward rotation of the foot;
- Complications during ankle surgery.
Statistically, about 1/4 of patients with tarsal tunnel syndrome have a history of trauma to the ankle joint. [11]
Certain systemic diseases are risk factors for the development of the syndrome or the exacerbation of the syndrome:
Hypothyroidism can cause tissue swelling and thickening due to a buildup of glucosaminoglycans and hyaluronic acid and is accompanied by fluid retention. [13]
Diabetes has a detrimental effect on peripheral nerves due to the chronic increase in glucose levels. This leads to the formation of sorbitol, a byproduct of glucose utilization. It accumulates in high concentrations, increasing the osmotic pressure in the cell and causing swelling. Angiopathy and narrowing of the peri- and intraluminal vascular lumen during diabetic debulking are also considered mechanisms of nerve damage. [14]
Symptoms of tarsal tunnel syndrome
Damage to the posterior tibial nerve can be bilateral. When it is compressed, the following symptoms occur
- pain in the posterior shin region;
- Tingling and burning in the soles of the feet and toes (paresthesia);
- Reduction in muscle strength when flexing the toes;
- Changes in gait - it becomes painful, delicate and the patient tends not to put any weight on the injured foot.
Pains In this syndrome, the peripheral nerve is the main symptom. It manifests itself in the form of a burning sensation or pain that radiates to the back of the lower leg. It can occur in the sole, foot, toes, and anywhere along the course of the tibial nerve.
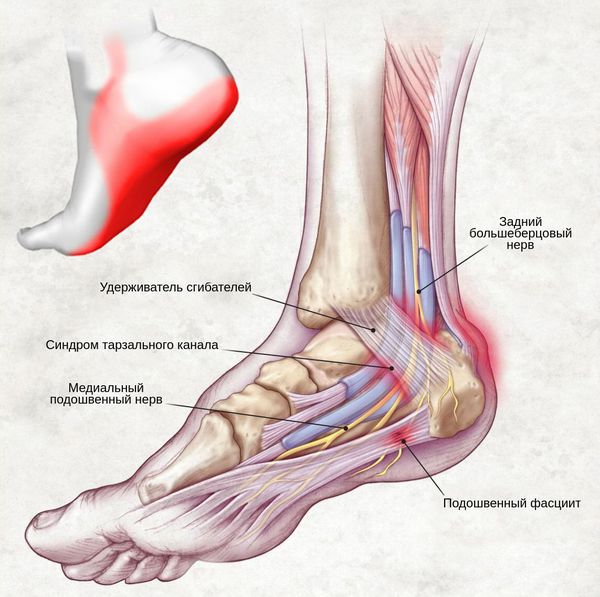
The painful feeling is caused by pressure on the canal, movement, walking, tapping and various movements of the ankle joint - landing, pushing off and extending the foot. It can also be uncomfortable at night.
Painful paresthesias – A constant feeling of numbness, tingling, burning or stinging that worsens when walking and occurs in the area of the toes and sole innervation:

This is also not uncommon with this syndrome. Mild paresis of the toe flexors ('cat's paw') and Trophic changes in the skin Changes in the skin on the feet.

The nerve compression weakens the neuromuscular signal and makes it difficult to extend the fingers to the side. This leads to hypotrophy and sometimes atrophy of the finger flexor muscles.
complications
Untreated tarsal tunnel syndrome leads to permanent and irreversible nerve damage. Because the nerve damage affects the leg, pain occurs.
The diagnosis of tarsal tunnel syndrome is made by a neurologist. During the examination, the neurologist asks about the onset of symptoms and a history, e.g. B. after trauma in this area. He or she will examine the foot and ankle, looking for physical features that could indicate tarsal tunnel syndrome. A Tinel test is performed in which the tibial nerve is lightly tapped. If the patient feels tingling or pain during this test, this indicates tarsal tunnel syndrome. The neurologist may also recommend additional tests to determine the cause, including electromyography, a test to detect nerve dysfunction, and an ultrasound scan of the nerve. An MRI scan of the ankle and foot is indicated if the doctor suspects that a tumor or bone hypertrophy may be the cause of tarsal tunnel syndrome.
Treatment
Tarsal tunnel syndrome can be controlled with a wide range of treatments. Regardless of the underlying condition, early treatment is important to prevent irreversible damage to the nerve. Anti-inflammatory medications can be taken at home to reduce inflammation. Rest, cooling and compression reduce swelling and inflammation.
Steroid injections may be given to reduce swelling in the affected area. In some cases, splints are used to immobilize the foot and limit movements that compress the nerve. For naturally flat feet, special shoes can be ordered to support the arch of the foot. In severe, long-term cases, the neurologist will recommend surgery in which the surgeon makes an incision from the ankle to the arch of the foot and releases the ligament. Some surgeons also use minimally invasive procedures that involve making much smaller incisions in the ankle. The surgeon uses instruments to stretch the ligament. Because there is less injury to the tissue, the risk of complications and recovery time are lower.
treatment methods
Treatment of pathology can be conservative or surgical. Non-steroidal anti-inflammatory drugs are the first measure to eliminate swelling and pain, and the doctor also selects drugs to improve trophism and promote nerve regeneration.
It is very important to choose the right footwear and use spinal insoles. These support the foot in the supination position and prevent pronation.
If symptoms are severe, cortisone may be prescribed. Injecting into the flexor tendon canal helps relieve inflammation and swelling and reduces irritation to the nerves.
If conservative treatment is ineffective, surgery may be indicated. The tibial nerve is released from the canal. This allows its compression to be eliminated. The operation is carried out under general or spinal anesthesia - an incision is made in the back of the inner ankle and the bursa is severed along its entire length. During the healing process, connective tissue forms and the flexor heals in a relaxed position.
Results
The doctors at the Zdorovya Clinic on Kurskaya are very experienced. They quickly and correctly make a diagnosis and prescribe the appropriate treatment. The process of restoring the tone of the foot flexor muscles takes a long time, but complete recovery is possible. The health clinic has all the necessary diagnostic equipment, which is very convenient - once you pass the equipment diagnosis, you can go directly to the doctor with the test results and start treatment.
To speed up the recovery process after treatment, the doctor prescribes special exercises to maintain muscle tone. Physiotherapy is also indicated to relieve pain and swelling. Physiotherapy can be combined with anti-inflammatory ointments.
Diagnosis of carpal tunnel syndrome
On neurological examination, an area of hypoesthesia corresponding to the innervation of the median nerve, a certain reduction in strength in the muscles innervated by the median nerve and autonomic changes in the skin of the hand (coloring, temperature and marbling of the skin) are noted. Further tests are done to determine: Falen's sign - paresthesia or numbness in the hand with passive flexion and extension for one minute, Tinel's sign - tingling in the hand when tapping in the wrist area. The exact topography of the lesion can be determined by electromyography and electroneurography.
To investigate the development of carpal tunnel syndrome, a blood test for RF, blood chemistry, x-rays of the wrist and carpus, an ultrasound examination of the wrist, a CT or MRI scan of the wrist, and, if indicated, a puncture of the wrist should be performed. A consultation with an orthopedist or traumatologist, endocrinologist or oncologist is possible. Carpal tunnel syndrome must be differentiated from radial nerve neuropathy, ulnar nerve neuropathy, upper limb polyneuropathy, vertebrogenic syndromes due to cervical spondyloarthropathy, and osteochondrosis.
Treatment of carpal tunnel syndrome
The main goal of treatment is to eliminate carpal tunnel stenosis. These include correction of dislocations, immobilization of the hand, correction of endocrine and metabolic abnormalities, control of inflammation, and reduction of tissue swelling. Conservative treatment is carried out by a neurologist, if necessary in collaboration with other specialists. The surgical treatment is determined by a neurosurgeon.
Conservative treatment is limited to immobilizing the affected hand with a splint for about 2 weeks and anti-inflammatory, analgesic and anti-edema pharmacotherapy. NSAIDs are used (ibuprofen, indomethacin, diclofenac, naproxen); in severe cases, corticosteroids (hydrocortisone, prednisolone) are prescribed; For severe pain syndromes, therapeutic wrist blocks with the introduction of a local anesthetic (lidocaine) are used. Edema is treated with diuretics, mainly furosemide. Vitamin therapy with Gr. B, mud treatment, electrophoresis, ultraphonophoresis and dimethyl sulfoxide compresses have a positive effect. Vascular therapy with pentoxifylline and nicotinic acid can reduce median nerve ischemia. After clinical improvement, physical therapy, hand massage and myofascial hand massage are recommended to restore nerve function and hand muscle strength.
If conservative measures are ineffective, carpal tunnel syndrome must be treated surgically. The operation consists of cutting the transverse carpal ligament. It is performed on an outpatient basis using an endoscopic technique. If there are significant structural changes in the carpal tunnel area, an open operation is performed because the endoscopic technique is not possible. This widens the carpal tunnel and relieves compression of the median nerve. Two weeks after the operation, the patient is able to perform hand movements that do not require significant strain. However, it takes several months for the hand to heal completely.
What is the tarsal canal in the foot?
First, we need to understand what the tarsal canal is and where it is located. The tarsal nerve is a branch of the sciatic nerve that branches in the cervical fossa. The tarsal canal of the foot is located on the inner (medial) side of the ankle joint. It is formed by the flexor tunnel (a structure made of dense fibrous tissue). Inside the tunnel there are blood vessels and nerve fibers. It emerges from the plantar part of the foot. Another name for this tunnel is Richet's heel canal.
Tarsal tunnel syndrome can be caused by an abnormal deformation of the internal tissues or by pressure from the heel bone, talus, deformed tendons, etc. Malposition of the foot and valgic (X-shaped) deformity of the shinbone are important factors in the development of this pathology.
A comprehensive treatment approach is used to determine the possible cause. The doctor will do everything necessary to eliminate their negative effects.
Causes of tarsal tunnel syndrome in the ankle
Tarsal tunnel syndrome is more commonly diagnosed in overweight patients who have problems with foot positioning. An inflammatory etiology of this disease occurs in approximately 30 % cases. The secondary form due to tumor growth and cyst formation occurs in 5-7 % of patients. Trauma, including ankle ligament sprains, dislocations, fractures, and breaks of the heel, one of the tarsal bones, and the talus, can contribute to tunnel syndrome.
Other causes of tarsal tunnel syndrome include the following risk factors:
- X-shaped tibial deformity;
- Flat or clubfoot, which causes deformation of the metatarsal and tarsal bones;
- Shortening and scarring of the ankle tendon;
- overweight;
- excessive physical stress on the foot (heavy lifting, heavy carrying, physical work, long standing);
- unsuitable footwear for daily wear and sports.
The exact cause of tarsal tunnel syndrome in the foot often cannot be determined. Therefore, treatment aims to restore the physiological permeability of the canal. If the cause is known, treatment is initially aimed at eliminating it. For example, if a patient has been diagnosed with flat feet and valgus deformity of the lower leg, the osteopath will correct the position of the foot. Once the correct position is restored and the tibial curvature is eliminated, therapy to restore the patency of the tarsal canal can be performed.
RISK FACTORS AND PREVENTION
Tarsal tunnel syndrome is known to occur more often in people who stand on their feet for long periods of time. Intense physical activities that involve plantar flexion of the foot can also cause symptoms characteristic of tarsal tunnel syndrome. A predisposing factor for the development of tarsal tunnel syndrome is flat feet.
Obesity doubles the risk of mechanical overload of the foot and is often accompanied by diabetes (a complication of which is neuropathy, which makes the nerves more sensitive to even minimal pressure).
It is also thought that tarsal tunnel syndrome is often associated with rheumatoid arthritis, hypothyroidism and gout.
Treatment of tarsal tunnel syndrome
The main goal of treating tarsal tunnel syndrome is to eliminate the causes of the pressure and allow the area to heal, thereby reducing pain and inflammation. Cold treatment can relieve joint and muscle pain, including in the foot.
Before resorting to invasive procedures (surgery and procedures), long-term conservative treatment should always be attempted, but in some cases it is the only option. Direct conservative measures can include:
– Weight loss (this reduces stress on the area)
– Nerve mobilization (the doctor can stretch the tibial nerve and reduce the pressure in the area of compression)
What can I do if I have leg pain?
1. General exercise and activity are recommended, but remain within the pain limits. Two walks a day of 20-40 minutes are good for the body and sore muscles.
2. Trigger points/massage balls are highly recommended – they come in different sizes so that you can target all areas of the body. There is no better self-help than this! We recommend the following (click image below) - it is a complete set of 5 trigger point/massage balls in different sizes:


Applies to restless feet, plantar fasciitis and heel spurs? Balls are particularly useful in treating these diseases too!
3. Training: Targeted training using training techniques from different opponents (such as this set of 6 knitted balls with different resistances) can help train strength and function. Knit training often involves more specific training, which in turn can lead to more effective injury prevention and pain reduction.
4. Pain relief means cooling: Biofreeze is a natural product that can relieve pain by gently cooling the affected area. Cooling is particularly recommended if the pain is very severe. Once they have calmed down, heat treatment is recommended - so it is advisable to use both cooling and heating.
5. Pain relief – warming: Warming the muscles can improve blood circulation and relieve pain. We recommend the following reusable hot/cold pad (click here to learn more) - which can be used for both cooling (can be frozen) and warming (can be microwaved).
classification
Classification of peripheral neuropathies according to etiological and pathomorphological features (WHO, 1982)
B. Acquired by or consumed by:
1. exogenous poisons and drugs:
– Metals: arsenic, mercury, gold, alkenes, aluminum, zinc, thallium;
– Solvent: hexane, carbon tetrachloride, carbon disulfide, methyl and butyl ketone, acetylacetone;
– Drugs of different groups: acrylamide, leptophos, organophosphates, carbon monoxide, nitrogen dioxide, 2,4-dichlorophenolacetic acid, chlordecone;
– Medications: Vincristine, Nitrofuranton, Isoniazid, Adriamycin, Clioquinol, Danson, Phenytoin, Amitriptyline;
– Poisons from invertebrates: botulinum toxin, black weaver spider venom, tick venom.
2. Metabolic disorders: diabetes mellitus, renal failure, liver failure, porphyria, hypoglycemia, myxedema.
3. in connection with deficiency symptoms: thiamine (in case of alcohol abuse), vitamin B12, pyridoxine, niacin, pantothenic acid, riboflavin, in case of protein-alcohol deficiency.
4. Other causes and types of neuropathy: malignant tumors, myeloma, 'senile' neuropathy.
1. Idiopathic infectious or post-infectious:
For collagen vascular disease, other vascular diseases, diabetes, atherosclerosis.
During compression (position), stretching, detachment.
Classification of diseases of the peripheral nervous system (All-Union Commission on Diseases of the Peripheral Nervous System, 1982-1984)
Vertebrobasilar lesions
1.1.2 Cervicocranialgia (posterior neck sympathetic syndrome, etc.).
1.1.3 Cervicocranial pain with musculotonic, autonomic-vascular or neurodystrophic symptoms
1.2.1 Discogenic (vertebrogenic) lesions ('radiculitis') of the radial roots (please specify which).
diagnosis
Diagnostic Criteria
Mononeuropathy is an isolated lesion of individual nerve trunks. The disease is caused by direct external trauma or compression at a certain level of the nerve trunk. The predisposing factor is the superficial location of the nerve on the bone or its passage in channels formed by bone and ligamentous or muscular elements. Under these anatomical conditions, the affected parts of the nerve trunks are particularly sensitive to occupational chronic or sports trauma, compression of the limbs during deep sleep, etc.
In atherosclerosis, diabetes, periarteritis nodosa and other collagenous mononeuropathies caused by ischemia (ischemic neuropathies), direct infection of individual nerves is rare (leptospirosis, leprosy). The only exception is the involvement of cranial nerves in herpetic infections.
In many cases, the etiology of neuropathy remains unclear. Paralysis of the main trunk leads to the loss of all its functions. More distant foci cause only partial impairment. The clinical picture also depends on the extent of nerve fiber damage.
Complaints and anamnesis
Complaints such as limitation of active movements of the paralyzed limb, weakness of the limb, pain syndrome, decreased muscle tone, decreased tendon reflexes, abnormal positioning of the paralyzed limb, changes in sensation. The cause is determined based on the anamnesis: trauma, infection, illness – diabetes.
Physical examination: Movement disorders – limitation of movement of the paralyzed limb, pain syndromes, sensory disorders, decreased tendon reflexes, hypotrophy of the paralyzed limb, decreased muscle tone.
Radial nerve neuropathy. When the radial nerve is damaged as a result of paralysis of the supinators of the forearm and the extensors of the hand and fingers, the hand is pronated and semi-flexed, the hand hangs down. The hand is bent irregularly: the little finger is particularly bent, the ring finger is less bent, the middle finger is even less bent, etc. Impairment of extension of the forearm, wrist and fingers, abduction and extension of the thumb, atrophy of the triceps muscle brachioradialis, the extensor muscles of the hand and fingers, reduced or absent reflexes - radial and from the triceps brachioradialis muscle, impairment of sensation on the dorsal surface of the fingers I, II and partially III. Positive Beck's sign - when the radial nerve is damaged, passive adduction and rotation of the hand cause pain at the point where the radial nerve enters the humeral groove.
Read more:- tarsus.
- Syndrome of the tibial nerve.
- Innervation of the lower leg muscles.
- What is supination and pronation of the hands?.
- Tibialis posterior muscle.
- median soleus nerve.
- Long fibula muscle.
- Medial tibial strain syndrome.
