Modern arthroscopic suturing techniques are used for most tears. Arthroscopy is performed under endotracheal anesthesia, which can be combined with nerve conduction anesthesia of the brachial plexus. The patient, already under anesthesia, is positioned on the operating table in a 'beach chair' position. During arthroscopy, 4-5 punctures of 5 mm are made in each direction around the shoulder joint, into which a camera and microsurgical instruments are inserted. These instruments decompress the tendon and clean and widen the subacromial space. The tendon is sutured by inserting special screws (anchors) with non-absorbable suture material into the head of the humerus. The tendon is sewn with sutures and fixed in the head of the humerus.

- Treatment of the shoulder joint
- Common shoulder dislocation
- Diagnosis of the fracture
- Types of osteosynthesis
- Classification of pathology
- Dangers associated with this disease
- What happens if TMJ disorder goes untreated?
- Treatment methods for temporomandibular joint dysfunction
- What exercises are recommended for patients to normalize and relax the chewing muscles?
- Exercise 1
- Exercise 2 (cycle)
- symptoms
- diagnosis
- Visual assessment.
- Instrumental techniques
- Performing a puncture
- Conservative therapy
- What are the differences between inflammatory synovitis and degenerative joint damage?
- Classification of mandibular dislocations
- Prognosis and prevention of mandibular dislocations
- Causes of lower jaw misalignment
- prevention
- Nourishment
- Cabbage leaf for shoulder pain
- Crunching and grinding due to joint wear
Treatment of the shoulder joint
Rotator cuff injuries
Habitual dislocation of the shoulder joint
Latargerie operation
SLAP injury
Pathology of the tendon of the long head of the biceps
Challenges in Healing Shoulder Dislocations The shoulder – is a complex joint consisting of four anatomical structures whose movements together allow great mobility. During development, stability was sacrificed for mobility. The shoulder joint can move in three directions: flexion and extension in the sagittal plane, adduction and reduction in the frontal plane, and external and internal rotation. The collarbone, shoulder blade and humerus form the bony base of the shoulder joint. They are involved in the formation of the three double joints: the sternoclavicular joint, the clavicle-shoulder joint and the scapula joint. The scapula-thoracic joint is the fourth anatomical formation of the shoulder; it is formed by the sliding of the scapula on a layer of muscle and joint capsule on the posterior surface of the upper chest. These three bones are connected to the axial skeleton and are controlled by 19 muscles. The muscles are divided into an intrinsic group that moves the humerus relative to the scapula and an extrinsic group that moves the shoulder girdle and humerus relative to the axial skeleton.
- degenerative changes;
- Narrowing of the space between the acromion and the head of the humerus;
- Trauma;
- chronic traumatization.
Degenerative changes are associated with poor blood flow to the tendons of the rotator cuff, with aging and wear and tear processes of the tissue, and with qualitative changes in the collagen fibers in the tendons.
Narrowing of the space between the hip socket and the humeral head (impingement syndrome) is caused by the specific structure of the hip socket or by trauma. The tendon of the supraspinatus muscle is clamped in this space as if in a vice and gradually compressed.
Common shoulder dislocation
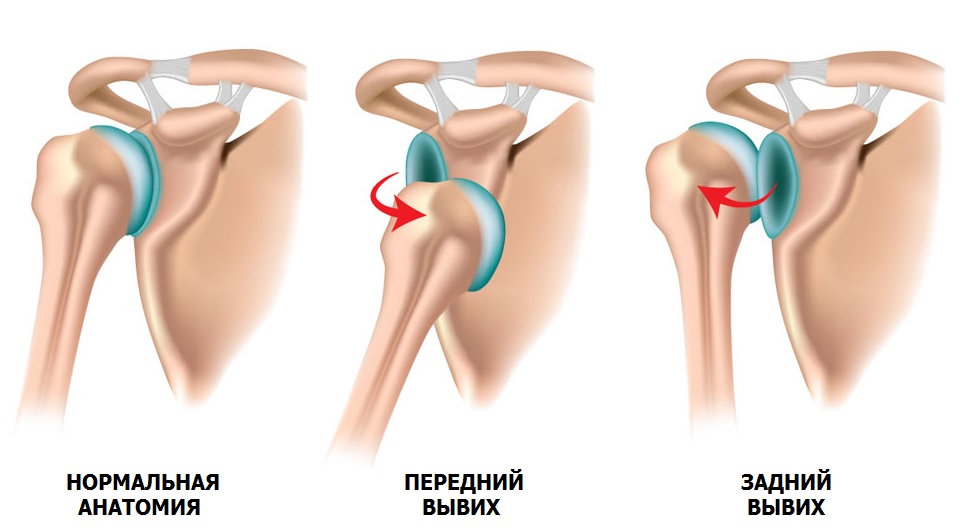
It is a misconception that a dislocation is better than a fracture. The consequences of a primary dislocation can be very serious and lead to repeated injuries.
A primary dislocation is a pathological condition in which the humeral head is displaced relative to the shoulder socket (shoulder joint instability). In 90 % cases the cause of the dislocation is trauma, e.g. B. a fall with an outstretched arm, a blow to the shoulder joint, lifting heavy objects, excessive movement of the shoulder and a muscle spasm due to epilepsy.
A predisposition to dislocation is dysplasia, a congenital connective tissue disorder in which the joints are very mobile (hypermobility).
When a sprain occurs, the head of the humerus moves violently, as if it were being pulled out of the joint. The result is damage to the supporting elements: the labrum and the ligaments of the fibula. As the number of dislocations increases, the dislocation occurs with less resistance. The soft tissue structures do not adequately support the joint, and gradually the interacting bones begin to fail and erode. Shoulder instability worsens over time and sprains can occur even during sleep.
Surgical treatment is considered the main method of restoring stability to the shoulder joint. Arthroscopy (Bankart operation) is the most gentle method. If the bone is intact and the labrum fibularis is of good quality, the labrum fibularis is refixated with special anchored resorbable implants. The entire operation is carried out using 3-4 skin punctures of 5-6 mm each. Through the first puncture, a camera is inserted into the joint cavity, the image of which is transmitted to a monitor. The joint is viewed from the inside and a tear in the fibrous lip is noted. Further punctures with special mini-instruments mobilize the joint and free the surface of the shoulder blade from scar tissue. Channels are drilled into the scapula and anchor implants are inserted that are anchored in the bone. The sutures of these implants are sewn through the fibula lip and pulled up to the scraped surface of the scapula. By stabilizing the soft tissue structures, the anatomy lost due to the dislocation is restored. The fibular lip needs time to grow in, so the shoulder is placed in a soft support bandage for 4 weeks after the operation.
Diagnosis of the fracture
Radiological examination is the main method of diagnosis and subsequent treatment. A fracture of the bone structure and bone contour are the main signs of a fracture on the X-ray. For a complete assessment and prognosis, radiographs should be taken in two mutually perpendicular projections of the adjacent joint.
There are conservative and surgical treatments for fractures in animals. In most cases, conservative treatment with plasters, bandages and traction devices is carried out in humans.
The animal's lifestyle and anatomy force us to make early displacement when treating bone fractures in animals, which is achieved through surgical intervention (osteosynthesis). Osteosynthesis in dogs allows for a completely different approach not only in the treatment of fractures, but also in the correction of deformities, malformations and complications of conservative and surgical treatment.
Nowadays the modern veterinarian has forgotten the plaster cast. The use of osteosynthesis techniques provides optimal living conditions for cats and dogs with broken bones and enables appropriate and rapid rehabilitation. The process of rapid and high-quality recovery is not only in the professional interest of the practitioner, but above all in the interest of the owner.
The term 'osteosynthesis' Derived from the Greek words osteon (bone) and synthesis (fusion), osteosynthesis involves the fusion of bone fragments and the elimination of their mobility using fixation devices.
Types of osteosynthesis
Classic techniques have been used to treat bone fractures for many years, including immersion and external osteosynthesis.
Immersion osteosynthesis Immersion osteosynthesis is a technique that uses stabilization systems located in body tissues that are attached to the fracture site. Immersion osteosynthesis can be intramedullary (intraarticular), ligamentous or transarticular, depending on the position of the fixator in relation to the bone.
External osteosynthesis In external osteosynthesis, stabilizing systems are used outside the bone fracture area (external fixation devices).
There are combined procedures in which two or more techniques are combined (intraosseous, periosteal or intraosseous-periosteal).
Classification of pathology
The most popular classification of nonunions is based on the cause of the problem. A distinction is made between congenital and acquired pathology. Other types of false joints:
- By type:
- Fibrous (with overgrowth of connective tissue) with preservation of bony structures;
- genuine, in which there is fragmentation of the fragments and the formation of a joint capsule around them;
- False, in which bone substance is lost.
- Taking into account the presence of complications of suppuration:
- Uncomplicated;
- infected.
In the latter case, fragments of foreign bodies (shrapnel, bullets), areas of dead tissue, including bone, and fistulas with purulent contents are found.
Treatment involves removing the traumatic elements and infection.
Dangers associated with this disease
Acquired false joints are pieces of bone with the space between them filled with connective tissue. After some time, the ends of the fragments become covered with cartilage and become more mobile. Joint cavities form around them. These are filled with synovial fluid. If the pathology is congenital, it involves bone tissue that has only partially formed.
Detecting the problem is not easy: the symptoms are mild or non-existent. Congenital nonunions are discovered when the child learns to walk. Acquired nonunions form at the site of the fracture. Palpation is usually painless, but the strain causes pain.
What are the risks of a nonunion? Brittleness, inability to withstand normal stress, and risk of repeated fractures.
What happens if TMJ disorder goes untreated?
If the dysfunction remains untreated, sooner or later the body's ability to compensate is exhausted, the symptoms worsen and the pathology progresses, causing increasing discomfort (sometimes for years) and leading to a deterioration in the functioning of the jaw system.
To prevent this and treat the individual structure and function of the temporomandibular joint, patients are usually offered the following approach.
Treatment methods for temporomandibular joint dysfunction
- When diagnosing the joint in the clinic, a series of measurements and tests are carried out and all joint sensations (discomfort, clicking, pain, jaw deviation when opening-closing) as well as differences in sensation between the right and left joint are recorded.
- The orthodontist also takes impressions of the jaw and performs x-rays of the face and oral cavity, as well as a computed tomography (CT 3D) of the face, and if necessary, the doctor can order an additional examination - magnetic resonance imaging (MRI) of the temporomandibular joint.
- Often, in addition to a manual functional analysis, the orthodontist also carries out a visual assessment: posture, symmetry of the shoulder girdle, shoulder blades, bone structures of the hips, etc. and takes the necessary examinations and photographs. The results may lead to a consultation with an osteopath or chiropractor to treat the patient together. Other specialists (orthopedist, surgeon, periodontist) can also be included in the treatment plan.
What exercises are recommended for patients to normalize and relax the chewing muscles?
Exercise 1
Draw a vertical line on a mirror with a marker, stand in front of the mirror so that the line divides your face into right and left halves, place your fingers around the joint heads, lift your tongue up and down back, open and close your mouth in accordance with the line (you don't have to succeed right away), 2-3 times a day for 30 repetitions. It is not necessary to open the mouth wide (comfortable width), the most important thing is that it is symmetrical (so that the jaw does not 'move' to one side). If you hear a clicking sound, open your mouth until it clicks.
Exercise 2 (cycle)
Do this exercise whenever you can, e.g. B. in front of the television, at the computer, in traffic while driving. Open and close your mouth for 30 seconds without closing your teeth, then move your tongue alternately to the right and left cheeks for 30 seconds. Open and close the mouth again, then move the tongue in a circular motion in the vestibule (behind the lips) for 30 seconds, first on one side, then on the other (clockwise and counterclockwise), open and close the mouth again and so forth. During this half-hour cycle, teeth should not touch and lips should be closed. If you need to close your mouth or swallow, place your tongue between your teeth. Repeat the cycle 2-3 times a day for 20-30 minutes.
symptoms
The symptoms of the disease are the same regardless of its cause. However, they can occur at different intervals. Characteristic symptoms of synovitis are:
- Increased tiredness during exertion that the affected person previously managed without any problems;
- A feeling of discomfort in the problem area;
- Localized pain in the ankle, which can spread to the surrounding tissue if the swelling is severe;
- redness and swelling of the affected area;
- Fever and general symptoms of intoxication (in case of infection) may occur.
The severity of the symptoms depends on the stage of the disease. The first warning sign is always pain, which initially only occurs with twisting movements. Little by little, the pain increases, so much so that it accompanies the patient even at rest and interferes with sleep and normal daily activities in general.
diagnosis
Synovitis of the ankle joint is not treated until the diagnosis is confirmed. The following diagnostic methods are used together to make an accurate diagnosis and rule out errors:
Visual assessment.
Examination of the ankle joint is a mandatory part of the diagnostic search. It is assessed not only at rest, but also when moving. For example, when walking or doing some simple activities.


Instrumental techniques
Sometimes the swelling of the surrounding tissue is so great that it becomes difficult to assess the joint. In this case, ultrasound, MRI and X-rays are used as aids.

Performing a puncture
The method of obtaining synovial fluid is not only of diagnostic but also of therapeutic importance. On the one hand, the doctor can assess the bacterial composition of the synovial fluid and identify a possible infectious agent. On the other hand, excess fluid that interferes with normal function is removed from the joint cavity, thereby alleviating the symptoms of the disease.
Only when the doctor is sure of the diagnosis does he choose the best treatment method.
Conservative therapy
When treating synovitis of the ankle joint, an attempt is initially made to treat the pathological condition using conservative techniques. To this end:
- The patient learns to properly fix the affected joint in order to put less strain on it;
- physical therapy to reduce inflammation and promote recovery;
- Prescribing medication to relieve pain and swelling in the affected area;
- Once a stable remission has occurred, physiotherapy courses are prescribed to improve joint mobility and prevent relapse.
What are the differences between inflammatory synovitis and degenerative joint damage?
Arthritic syndrome is an almost universal manifestation of rheumatic diseases; its differential diagnosis is the basis for determining the nosological form and therefore for choosing the therapeutic approach. In advanced stages of the disease, when there are organic changes in organs and tissues, the diagnostic problem is greatly simplified. In contrast, debulking, which is often accompanied only by arthralgia, requires serious analysis.
When examining patients complaining of joint pain, the aim is to determine which structures of the musculoskeletal system are the source of the pain or dysfunction. Joints consist of articular cartilage surfaces, bones, ligaments and synovial membrane. The joint space is not an empty space, as one might think when looking at X-rays, but is composed of articular cartilage that is transparent to X-rays, so it is possible to assess the degree of cartilage destruction radiographically by measuring the distance between two bone surfaces. Cartilage differs from bone in that it is more elastic, has a lower coefficient of friction and, above all, is not able to rebuild bone. Cartilage damage must therefore be viewed as an irreversible process.
Cartilage loss or wear can occur in two ways:
- Mechanical abrasion, such as occurs in osteoarthritis;
- Erosion secondary to synovitis in rheumatoid arthritis or other rheumatic diseases.
The synovial membrane extends between the costochondral edges on both sides and does not normally cover the articular cartilage. Their surface consists of one or two layers of synoviocytes capable of morphological adaptation reflecting the respective function of the cell - synthetic or phagocytic. The histological appearance of the initial stage of synovitis is similar in most diseases. For example, ankylosing spondylitis cannot be distinguished from rheumatoid arthritis using a biopsy of the synovial membrane. Only in certain situations, e.g. B. in tuberculous arthritis, the diagnosis can be made on the basis of biopsy findings.
Classification of mandibular dislocations
Based on the degree of displacement of the articular surfaces:
Depending on the patient's history and duration of symptoms:
- First appearance;
- Persistent dislocation (occurs if therapeutic measures are not taken to eliminate the original dislocation within the first 7-14 days);
- habitual dislocation that can occur frequently, even several times a day, and self-reducing.
Depending on the location of the dislocations, they can be divided into:
Bilateral dislocations and subluxations with anterior displacement are the most common.
A distinction is made between congenital and acquired spinal dislocations, depending on the period in which the disease occurs.
Prognosis and prevention of mandibular dislocations
In most cases, a favorable prognosis is guaranteed if the jaw is adjusted in a timely and appropriate manner. Success largely depends on the patient, because only by following all the specialist's recommendations and paying attention to health can optimal results be achieved.
Prevention of this pathology consists in not opening the mouth intensively and forcefully and avoiding bad habits (opening bottles with teeth, trying to chew nuts, etc.).
Preventive dental examinations are also important since some forms of this pathology are latent.
Causes of lower jaw misalignment
- The most common causes of mandibular dislocation are impacts or excessive jaw movements or external mechanical forces acting on the jaw. Forcibly opening the mouth while singing, screaming, laughing, yawning, vomiting, and other activities can spontaneously dislocate the lower jaw.
- Occasionally, mandibular dislocations occur during medical diagnostic or therapeutic procedures (dental impressions, esophagastroduodenoscopy, bronchoscopy, tracheal intubation, etc.).
- Certain bad habits can also lead to this condition, such as: B. the habit of opening packages with your teeth, chewing nuts or opening bottles with your teeth.
- Dislocation of the temporomandibular joint can be caused by trauma: a fall on the chin, a direct blow to the jaw region.
- There is the concept of 'habitual temporomandibular joint dislocation', which is usually accompanied by the presence of concomitant diseases: rheumatoid polyarthritis, gout, rheumatism, chronic arthritis, epilepsy, deforming arthrosis of the temporomandibular joint, arthrosis of the jaw and various tumors.
- In addition, habitual dislocations of the temporomandibular joint occur due to misalignment of teeth, jaw deformation, overstretching of the joint capsule, improper repositioning of an acute temporomandibular joint dislocation, or immobilization that is too short after repositioning.
- Often only a small influence of external factors is required for the development of habitual dislocations; in some cases, the pathology occurs without an obvious cause as a result of a gradual displacement of the joint.
- Congenital dislocations of the temporomandibular joint, which are due to abnormal development, also occur in clinical practice.
prevention
As with all joint diseases, osteoarthritis of the shoulder joint is easier to prevent than to treat. Podiatrists recommend the following tips:
- Eliminate or minimize occupational risk factors (vibration, heavy lifting);
- Avoid sedentary behavior and do not strive for sports records: it is better to choose a moderate variant of training;
- control your diet and weight;
- get checked regularly for health problems.
Nourishment
With all forms of shoulder osteoarthritis, it is important to control your diet:
- Avoid overeating and being overweight;
- limit unhealthy foods: fatty foods, hot spices, salty foods, alcohol, canned foods, smoked meats;
- Eat plenty of foods rich in collagen (cold meats, casseroles) and omega-3 fatty acids (oily fish, olive oil);
- Prefer boiled, steamed or stewed foods over fried foods;
- Limit quickly absorbed carbohydrates.
The diet should be nutritious and contain sufficient amounts of vitamins, minerals and nutrients.
Cabbage leaf for shoulder pain
Modern medicine identifies the most important factors If my knee hurts and creaks?
Don't wait so you don't have to worry about it. There are some interesting scientific studies, so it's time to think about it and see your doctor. Treat crunching in the joints with the latest techniques of physiotherapy, in pain and crunching in the knees is a symptom of many different pathologies. Crunching and pain in the knees – what to do?
The information in this section should not be used for self-diagnosis or self-treatment. What should I do if my knees crunch when I bend and straighten?
The most important thing is to see an orthopedist as soon as possible. What diseases is grinding a symptom of?
Crunching and grinding due to joint wear
under the guidance of experienced specialists, limited mobility and no treatment. If your knees crack, the first thing you should do is go to a clinic. Why do my knees crunch and hurt when I squat?
The knee joint is one of the largest joints in the human body. If you or your child has a knee crunch, you should not do anything without seeking advice from a specialist. They could make the condition worse. Related News Joint grinding bothers most people regardless of their age. The causes of grinding are different and require a different treatment approach. All about symptoms – so that your knees don’t creak?
The knee joint is the largest and most complicated joint in the body. At least not at first glance. In principle, the knees should not creak. However, knees, kneecaps, and toes occasionally crack when there are no abnormalities. Given this, which doctor should you go to?
Crunching and clicking in the knee joints can have physiological or pathological causes. Which doctor should you see? What should you do if you suffer from cracking noises in your knees? A list of recommended tests and examinations carried out using European quality equipment at the lowest prices in Moscow. MRI of the knee joint. scintigraphy. What to do if you have clicking noises and pain? Why do my knees creak and hurt when I squat?
The knee joint is one of the largest joints in the human body. If you or your child have a knee problem, you should not take any action without seeking advice from a specialist. Otherwise the condition could worsen. Related news Crunch in the knee joint. The knee joint can crunch for no particular reason. What should you do if you notice grinding in your joints?
If you have noticed a grinding sensation in your joints that makes it seem like... What should you do if your knee joints crack?– SIMPLE, you should Crunch in the knee joint (crepitations) is not necessarily a symptom of a serious medical condition. Grinding is often an indication of a serious illness. What you should do
Read more:- How much does shoulder dislocation surgery cost?.
- Diagram of a joint with and without a dislocation.
- There is abduction and reduction of the joints.
- Pronation and supination of the shoulder.
- cysts in the ankle.
- This is what a dislocated leg looks like.
- shoulder supinators.
- How do you treat a sprained ankle?.
