In this type of injury mechanism, the tendon that attaches to the base of the fifth metatarsal contracts and tears off part of the base of the bone. Such a fracture is called a detachment fracture.

- Fractures of the metatarsal bones
- Dancer's fracture (burst fracture of the base of the 5th metatarsal)
- ICD-10
- causes
- Symptoms of a metatarsal fracture
- Principles of Diagnosis
- Treatment
- Additional investigation methods
- Physical examination
- Additional investigation methods
- signs
- Causes of March Fracture
- Which doctor should I see?
- Fifth metatarsal fracture symptoms
- causes of injury
- Which doctor should I see?
- General characteristics of the problem: description, types of metatarsal fractures.
- causes and symptoms
- Advice after plaster removal
- Possible complications during rehabilitation
Fractures of the metatarsal bones
Fractures of the metatarsal bones are relatively common injuries to the foot, resulting from direct impacts or indirect injuries (wrenching the foot). Many of these fractures can be treated relatively easily and with good results. However, when misaligned or misaligned, these fractures can cause severe metatarsalgia and metatarsal arthritis. The tarsal bones are a common site for stress fractures and can be combined with injuries to other parts of the foot.
The tarsal bones are short, slightly curved tubular bones in the forefoot. Every bone has a head, a neck, a diaphysis and a base. Each metatarsal bone is named numerically from 1 to 5 in the inside-out direction (largest to smallest). The base of each metatarsal bone is connected to one or more tarsal bones, and the head is connected to the phalanx. The bases of the metatarsal bones also join to form interphalangeal joints. Functionally, all five metatarsal bones form a forefoot bearing complex. The three medial radii serve as a rigid lever when walking, while the two lateral radii ensure a certain degree of mobility, e.g. B. when walking on uneven ground is required.

The first metatarsal is the largest compared to the others and is the most important for the loading and balance of the foot. A fusion in an incorrect position or lack of fusion of this bone is the worst for the patient. This bone does not share ligaments with the adjacent second metatarsal, so they move independently.
The second, third, and fourth metatarsal bones are thinner and may present a localized stress fracture or trauma as a result of direct or indirect trauma.
Dancer's fracture (burst fracture of the base of the 5th metatarsal)
A burst fracture occurs at the base of the 5th metatarsal (Zone 1) where the short fibular tendon and plantar fascia attach. This injury is often referred to as a 'dancer's fracture' because it results from a missed landing after a jump or a foot roll after a jump. In this situation, the ankle is twisted and at the same time the short fibula is contracted, resulting in detachment of the base of the fifth metatarsal.
The original description of this term came from the legendary orthopedic surgeon Sir Robert Jones, who diagnosed himself with such a burst fracture in 1902 as a result of an injury sustained while dancing.

Fig. X-ray of a dance fracture (burst fracture) in zone 1 of the 5th metatarsal.
ICD-10

March foot (reconstructive foot disease, march fracture, Deutschländer's disease) is a condition caused by pathological remodeling of the metatarsal bones as a result of excessive loading. It can be acute or chronic, but is more often chronic at first. With conservative treatment by specialists in traumatology and orthopedics, it leads to a full recovery.

causes
Marching foot occurs in soldiers, athletes, and people whose occupation involves long periods of walking, standing, or carrying heavy loads. The likelihood of it occurring increases with wearing uncomfortable footwear and having flat feet. Studies from different countries have found that people with low levels of physical activity are more likely to develop walking after strenuous physical activity. It is believed that this is due to reduced bone strength. It is no coincidence that another category of such patients increasingly today are female tourists - office workers who actively 'run' around tourist attractions in uncomfortable shoes during their vacation.
Deichlender disease involves changes in the medial (diaphyseal) part of the metatarsal bone. In this case, the pathological remodeling of the bone tissue is caused by changed mechanical and static-dynamic factors. This process most often affects the 2nd metatarsal, less often the 3rd, and even less often the 4th and 5th. This distribution is due to the load on the foot when standing and walking, since in such cases the inner and middle parts of the foot are more loaded become. The 1st metatarsal is never injured. This is probably due to its greater density and strength.
Usually a single bone is affected, although multiple bones in one or both feet can be affected simultaneously or sequentially. It has been proven that the pouch foot is a special type of bone lesion that is not associated with cancer or inflammation.
However, experts still disagree on the nature of this lesion. Some believe that bone remodeling is associated with an incomplete fracture, or what is known as a microfracture. Others believe that the term 'march fracture' should be considered outdated and inappropriate as there is only local resorption of bone tissue which is then replaced by normal bone without the formation of a bony callus.
Symptoms of a metatarsal fracture
The severity of the symptoms depends to varying degrees on how severe the injury was. Often there are no visible signs of a fracture, and a person confuses a fracture with a simple bruise. However, there is some indirect evidence pointing to a closed fracture:
- Pain in foot after exercise.
- Spontaneous swelling of the metatarsal region.
- Reducing pain at rest.
- Occurrence of abnormal grinding and stabbing pain.
- Abnormal position of the toes.
- Swelling with hematoma and pain.
- An open fracture is characterized by more pronounced symptoms:
- The occurrence of bleeding.
- tearing of soft tissues.
- Expansion of the bone through the torn wound.
- Significant pain.
Principles of Diagnosis
All patients are first visually examined by a specialist. The doctor assesses the extent of the damage and prescribes additional diagnostic procedures. These include MRI, CT, or X-rays. After the examination is completed, a preliminary diagnosis is made. A plain x-ray (anteroposterior, lateral, and oblique) is usually sufficient to diagnose a fracture. CT or MRI scans are used to rule out other injuries and, if necessary, to determine the type of fracture. In some cases, a comparison with the opposite lower extremity may also be necessary.
Treatment
A metatarsal fracture requires special treatment. The method of treatment is selected and adjusted individually by the doctor. Conservative treatment is only used if the fracture has not displaced. Treatment procedures generally depend on the type and complexity of the injury and include.
- Symptomatic treatment Taking painkillers and antipyretics and wearing a soft protective bandage.
- Repositioning of the fracture under anesthesia
- Applying a short plaster cast to the injured limb.
- Therapeutic measures Wear immobilization shoes.
- Physiotherapeutic treatment
Additional investigation methods
To diagnose the fracture, the doctor will recommend further tests.
X-rays. With the help of X-ray images, we can assess the condition of compact anatomical structures, such as B. the bone, see and judge.
Most fractures are clearly visible on standard radiographs. Stress fractures can develop as microscopic abnormalities in bone structure and may not be visible on plain x-rays.
In many cases, a stress fracture only becomes visible on X-rays after several weeks, when a so-called callus has formed at the fracture site.


(Left) In this x-ray, the line of a recent stress fracture of the 3rd metatarsal in this patient is barely visible (arrow). (Right) A few weeks later, bone marrow formation is visible at the fracture site.
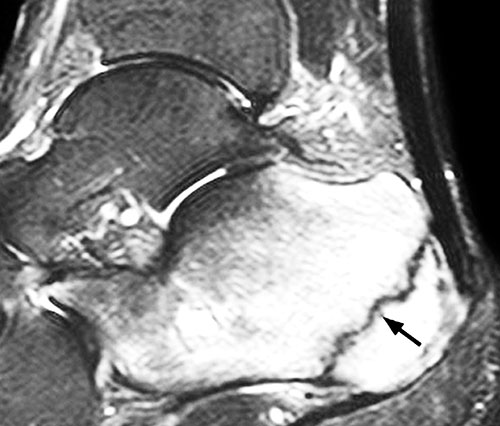
Magnetic resonance imaging (MRI). If there is a suspicion of a stress fracture that cannot be seen on x-rays, the doctor may recommend an MRI scan. This type of exam uses a magnetic field and radio waves to create images of the anatomical structures of different parts of the body.
Because MRI is more sensitive than X-rays, it can detect changes in bones that could indicate a fracture. Unlike X-rays, MRI does not involve ionizing radiation. The examination usually lasts about 40 minutes and is usually scheduled separately from the doctor's appointment.
Treatment of toe fractures varies:
Although toes are quite small, toe fractures are very, very painful.
Physical examination
Your doctor will discuss with you details about your medical condition, your job, your level of physical activity, your diet and any medications you are taking. It's important that your doctor is aware of any risk factors for stress fractures that you may have. If you've had a stress fracture in the past, your doctor may recommend a full physical exam to rule out a calcium or vitamin D deficiency in your diet.
After discussing all the points described, your doctor will examine your foot and ankle. During the examination, the doctor will determine where there is local pain. Often the key to diagnosing a stress fracture is pain from direct pressure on the injured bone. This pain is usually confined to the injured bone and does not extend to the entire foot.

Additional investigation methods
These can be recommended to confirm or rule out the diagnosis.
X-ray. With the help of X-ray images, the densest anatomical structures, such as e.g. B. the bone can be made visible. Since the integrity of the bone is only slightly compromised in a stress fracture, it is often not visible on the first x-rays. You can only see them after a few weeks, when the fracture has healed. After a few weeks, a 'cloud' called a callus appears on the x-rays at the fracture site. In many cases, the fracture line is also visible here.


(Left) This x-ray of a patient complaining of 2nd metatarsal pain shows no signs of a stress fracture. (Left) This x-ray shows callus formation in the area of a stress fracture 3 weeks later in the same patient.
Other research methods. If your doctor suspects you have a stress fracture but x-rays don't show it, they may recommend a scintigraphy or magnetic resonance imaging (MRI).
Scanning is less specific than MRI in locating a stress fracture, but both are more sensitive than an X-ray and can detect a stress fracture earlier.
Treatment goals include controlling pain, healing the fracture, and returning to full physical activity. By following the advice that is given to you, you can get back to your daily life as quickly as possible and prevent further damage to your bones.
signs
A metatarsal fracture is difficult to spot at first glance, even on an X-ray. The difficulty is that it is a 'green branch': the internal bone tissue is damaged first while the surface remains intact. It takes 4-5 weeks for the injury to become clearly visible. The presence of an injury can be recognized by the accompanying symptoms, which include a sharp pain when the foot is palpated. Other symptoms are:
The symptoms of the injury may not be very obvious, especially in the early stages. However, without treatment, the signs of a fracture will become more and more obvious. However, it is important to seek help at the right time, when therapy is most effective and does not last too long. It is therefore important to carry out diagnostics when a metatarsal fracture is first suspected in order to avoid serious consequences. This includes:
Such complications lead to increased stress on other parts of the musculoskeletal system, especially the spine. This situation leads to rapid wear and tear, resulting in pathologies of varying degrees of severity. Disorders caused by damage to the metatarsal bone require longer and more complex treatment, which is not always successful.
Causes of March Fracture
This injury is caused by heavy loading of the forefoot. In this case, the arch of the foot is disturbed and the metatarsal bone is damaged. Risk groups include military personnel, athletes, and people with an active lifestyle. The stress fracture of the marching foot is caused by factors such as the following in most cases
- unfamiliar footwear;
- Excessive use of the feet;
- Prolonged standing on feet;
- Carrying heavy loads;
- flat feet.
Injuries are not uncommon in physically fit people. This is the case, for example, with athletes who train intensively for competitions. Diseases can be triggered by professional activities when a person has to stand for a long time: hairdressers, shop assistants, lecturers. These people need to rest their legs by sitting down between jobs whenever possible. New employees are at risk. With them, the fatigue of the march can be caused by the type of military service:
In 5 % of the recruits, a combination of these causes leads to a marching fracture. In most cases, namely in 50 %, the second metatarsal is injured. The third and fourth metatarsal bones each account for 25 %.
Which doctor should I see?
A march fracture is difficult to detect in its early stages, but its consequences lead to more serious injuries. Despite the mild symptoms, diagnosis is important even when pathology is suspected. This is about the diagnosis and treatment of the disease:
Fifth metatarsal fracture symptoms
The symptoms of the pathology are very different depending on the type of pathology. In some cases, e.g. B. in stress fractures, the patient may confuse the symptoms with a simple bruise. It may be that there is no pain at all, and the pathology is diagnosed only on circumstantial evidence. A stress fracture of the metatarsal presents with the following symptoms:
A traumatic fracture is more pronounced. In these cases, after the injury to the bone, a characteristic crunching sound is clearly heard, which automatically indicates deformation. Pain appears almost immediately afterwards. Other symptoms of a traumatic fracture are.
- The appearance of a strong swelling with a hematoma after a few hours;
- abnormal position of one or more fingers;
- pain that subsides, followed by an increase in pain on exertion.
An open metatarsal fracture is characterized by tearing of soft tissue and bleeding. This leads to a strong pain syndrome that is difficult to miss. The ends of the metatarsal emerge to the surface and are easily discernible visually through the torn skin. A metatarsal fracture requires urgent treatment, even if the symptoms are very mild, as it can lead to serious complications.
causes of injury
There are two types of fractures, each caused by different factors. The stress fracture is milder and often heals spontaneously. It is caused by prolonged excessive stress on the foot. These can occur when:
In these cases, the foot is loaded for a long period of time, which leads to microfractures in the bone tissue. Traumatic fractures have more obvious causes. They are caused by external mechanical influences on the forefoot. These situations can occur when:
With the traumatic form of the pathology, the 5th metatarsal is most often broken. broken metatarsal. The next most common deformities are the first and second bones. The situation is particularly serious with a Jones-type fracture: the fifth bone is destroyed in an area with a restricted blood supply.
Which doctor should I see?
When the foot suffers trauma, it loses many of its cushioning properties. This means that the load is shifted to other parts of the musculoskeletal system, which can certainly lead to new diseases. Therefore, when a metatarsal fracture occurs, treatment is crucial. The diagnosis of the disease and its treatment will be discussed:
General characteristics of the problem: description, types of metatarsal fractures.
A metatarsal fracture is often associated with a direct impact or twisting of the foot.
Even if first aid is provided, patients are advised to contact an orthopedic trauma surgeon who can carefully examine the foot after a metatarsal fracture.
Doctors classify the problem according to the following characteristics:
- Traumatic fracture. It is associated with the aftermath of acute trauma and is located in the midfoot or forefoot.
- stress fracture. With prolonged physical exertion and repeated minor trauma.
There may be functional limitations with or without a shift. A distinction is also made between a closed and an open fracture of the metatarsal bone. Regardless of the type of fracture, a medical examination is essential.
causes and symptoms
There are many causes of a metatarsal fracture. For example, the patient may unhappily fall from a great height or be involved in an accident. Orthopedic surgeons also cite the following causes as important:
- the effects of intense and prolonged exercise;
- a lack of calcium in the bones, which affects their weakening;
- dropping a heavy object on the leg;
- Injuries resulting from a car accident.
When this problem occurs, a number of symptoms appear that can easily be mistaken for something else. However, the main signs of joint and bone dysfunction include:
- the gradual onset of pain, aggravated by exertion;
- the appearance of primary swelling of the foot;
- the appearance of subcutaneous bruising.
A patient with these symptoms begins to feel acute and obvious pain. In some cases, a grinding or clicking noise can be heard at the point of fracture. The resulting pain causes patients to limp, drag their feet, and experience significant pain that disrupts the normal flow of life. An obvious symptom of a metatarsal fracture is swelling of the foot that builds up over the day after the injury and gradually expands. As soon as night falls, however, it goes back again. In severe cases, patients are not always able to see the obvious deformity.
Advice after plaster removal
After a metatarsal fracture and cast removal, the patient must carefully monitor the condition of the limb. Strenuous exercises are strictly prohibited. To ensure the smooth course of rehabilitation, it is necessary to follow the doctor's recommendations:
- Crutches should be used immediately after the cast is removed. The joints become sluggish and immobile and the muscles atrophy. This can lead to a fall and another fracture.
- From the very beginning of rehabilitation, a person must learn to walk properly. Otherwise, it may be that the person affected hobbles for a long time until the end of his life.
- Salt and warm water baths can relieve muscle and joint pain.
- Once the cast is removed, therapeutic insoles should be used and shoes should be worn for at least a year.
- After a metatarsal fracture, pain always occurs. One should not sit or lie down. You should still walk, even if it hurts.
Physical activity should be increased gradually. It is not necessary to undertake kilometer-long marches. A few walks a day, to shop, to the park, etc. are sufficient.
Possible complications during rehabilitation
Some patients may experience complications during rehabilitation. These often occur when patients do not adhere to their individual rehabilitation program. Without professional help, they can lead to disabilities.
- Persistent pain in the foot area;
- synovitis;
- sesamoiditis
- arthritis of infectious origin;
- neuropathy;
- abnormal anastomosis of bone fractures.
Immediately after the end of the immobilization, the affected person must regain mobility of the foot. The treatment of the spine and joints must be supervised by a doctor. All treatments and exercises are strictly individualized. A gradual increase in the load on the foot, its immobilization and sports activities will help restore mobility and prevent complications.
Read more:- Fracture of the 5th metatarsal.
- Cracked metatarsal.
- Metatarsal tarsal bones.
- Fractures of the tarsal bones.
- The tarsal bone hurts from above - what to do?.
- bones of the foot.
- metatarsal bones.
- tarsal bone in Latin.
