CONTRACTILE TENDON

- Achilles tendon: anatomy, cellular structure, surgical treatment of injuries
- Achilles tendon anatomy
- ICD-10
- causes
- Our courses are suitable for both beginners and experienced trainers and offer income growth and career development.
- Types of joint tendinosis
- Tendinosis of the shoulder tendon
- Hip joint tendon and hip joint
- Free medical advice and diagnosis
- tendinosis of the knee
- Popliteal fossa and heel tendon
- Diagnosis of injury to the subacromial region
- Treatment
- How to get rid of the symptoms
- prevention
- Why does my heel hurt?
- Less common causes of heel pain
- Diagnosis of heel pain
- Material and methods.
- Results
- What is the cause of foot pain?
- Poorly fitting footwear
Achilles tendon: anatomy, cellular structure, surgical treatment of injuries
The English surgeon John Hunter is considered the author of the first major studies on the pathogenesis, mechanisms of rupture and treatment of Achilles tendon injuries. In his memoirs, the doctor described his own Achilles tendon rupture, as well as the course of treatment and detailed outcome. He also conducted a series of studies on dogs with torn tendons. He initially treated them conservatively and then killed them at various times to determine the regeneration stage of the tendon tissue.
The works published by Hunter remained relevant for 150 years. The numerous studies on Achilles tendon rupture generally did not contain any new information, but simply offered various options for immobilization with small differences in time.
The first authoritative comparative study that statistically demonstrated the validity of surgical treatment was published in 1929 by J. Qenu and 8. M. Stoianovitch. The study included 68 patients, 29 of whom underwent surgical treatment. The long-term results showed no statistical difference in treatment results, but the authors gave preference to the surgical method in their conclusions. This study has significantly advanced surgical treatment of the Achilles tendon.
The general principles of tendon suture, which are still relevant in the 21st century, were first formulated in 1936 by our compatriot Justin Julianovich Janelidze:
'The suture must be simple and easy to produce, it must not impair the blood supply to the tendon, for this purpose a minimum number of tendon bundles must be tied into knots and loops. The suture should provide a smooth, gliding surface to the tendon, with a minimal amount of suture remaining on the gliding surface, holding the ends in place and not unraveling the tendon.'
Achilles tendon anatomy
Via the Achilles tendon, the triceps tendon transmits force to the heel bone, which in turn transmits it to the foot, enabling walking, running and an upright posture. It is one of the anti-gravity muscles, just like the pelvic and spinal muscles. They are dominated by slow (white) muscle fibers, which are not capable of fast and precise movements, but have greater endurance compared to fast (red) fibers.
Each skeletal muscle has fibers of both types, and the ratio depends on the function performed. Fast muscle fibers predominate in the eye and hand muscles. In the antegrade muscles, slow fibers predominate, allowing long-lasting work with constant force.
The point where the tendon attaches to the bone is called the enthesis and has a specific anatomical and histological structure in antegrade muscles. The Achilles tendon is a combination of the tendons of the gastrocnemius and soleus muscles and forms the triseps surae muscle. The two heads of the calf muscle join together to form a thin, flat tendon at the level of the middle third of the tibia. They adhere to each other with the anterior surface of the calf aponeurosis and the posterior surface of the cambial aponeurosis. There are no connective tissue bridges between them, so they fuse to form the Achilles tendon at the lowest part of the calf tendon. The length of the calf tendon is variable and varies between 12 and 26 cm.

In 5 % cases there is a third head of the calf muscle that grows together with the medial head, and in 7 % cases the function of the medial head is taken over by the shoulder muscle. It does not form its own tendon, but rather connects to the calf muscle in the lower third of the aponeurosis. In rare cases, the lateral head merges into its own tendon and forms a separate calf bone system.
ICD-10

Tendinitis of the foot is an inflammation of the synovial membrane of the tendon, which is located on the dorsal or plantar surface of the foot. Primary tendinitis occurs as a result of sporting or occupational stress on a specific muscle group, secondary as a result of a spreading infection (in purulent processes and infectious diseases) or reactive toxic inflammation (in rheumatic diseases).

causes
Primary tendinitis of the foot is usually caused by microtrauma of the tendon sheaths as a result of increased stress or anatomical abnormalities of the various structures of the foot. Primary tendinitis of the foot is often diagnosed in skiers, ice skaters and ballerinas, as well as people with flat feet and other congenital or acquired foot deformities.
Acute purulent tendinitis of the foot is caused by contact or hematogenous spread of infection from a purulent source (infected foot wound, panaritis, purulent arthritis, osteitis, abscess, phlegmon, etc.). Chronic tendinitis can develop in a variety of specific and nonspecific infectious diseases: tuberculosis, gonorrhea, brucellosis or influenza. In rheumatic diseases (Reiter's syndrome, Bechterew's disease, systemic scleroderma, rheumatism and rheumatoid arthritis), chronic tendinitis of the foot is caused by reactive inflammation of a toxic nature.
Our courses are suitable for
Suitable for both beginners and experienced trainers, offering income growth and career development.


The User purchasing the Services on evotren.ru, hereinafter referred to as the “Customer”, on the one hand, and Evotren LLC, hereinafter referred to as the “Contractor”, represented by the CEO FG Kapishev, acting within the framework of the Charter, on the other hand, have entered into this Agreement (hereinafter referred to as 'contract') for the purchase of the contractor's services as follows
1. TERMS AND DEFINITIONS USED IN THE CONTRACT
1.1. customer – natural person, sole proprietorship or legal entity, regardless of its legal form, who has placed an order with the Contractor in accordance with the terms of this Agreement and purchases the Services of the Contractor.
1.2. contractor – is the legal entity that provides services to the Customer under the Agreement.
1.3. Services – Services consisting in providing access to the study of the distance learning material indicated in the description of the information courses.
1.4. site – The contractor's information resource, located on the Internet at: edu.evotren.com
1.5. The client's personal account – The program interface on the website for studying information materials and other necessary information, which is accessible to the customer after authorization via login and password.
1.6. Order – An automatically generated document listing the services requested by the customer. The order is drawn up by filling out the necessary forms on the contractor's website -www.evotren.ru.
1.7. Acceptance of the terms of the contract – The acceptance of the contractual conditions by the customer takes place by paying for the services in cash or by non-cash or electronic means of payment. Acceptance of the terms and conditions of the contract is deemed to have occurred when the customer has paid for the services in cash or by non-cash or electronic means of payment.
Types of joint tendinosis
Tendinosis can be diagnosed in its late stages by palpation, X-ray or MRI. During the examination, changes in the tendon fibers and traces of salt deposits become visible.
Tendinosis of the shoulder tendon
It occurs at the junction between the pinion, trapezius and rhomboid muscles in the cervical and thoracic spine. The condition often develops as an occupational deformity in weightlifters. The pathology severely limits the range of motion of the shoulder girdle. It is no longer possible to lift the arm or move it from side to side. Pain, cracking and popping noises occur when moving.
Strains or dislocations of ligament and tendon fibers can lead to post-traumatic tendinosis of the shoulder joint in the rotator cuff area. By delaying a visit to the doctor, the patient damages the muscle cortex in the shoulder area. This muscle structure begins to atrophy due to limited mobility and lack of exercise. A timely visit to the orthopedist at the first sign of symptoms is therefore essential.
Hip joint tendon and hip joint
The pathology must be treated under the guidance of a specialist, otherwise the likelihood of complications is high, which will lead to almost complete immobilization of the patient. As a result of the lesions, the adductor tendon fibers are damaged. Pain during physical activity radiates to the socket region and the cartilage tissue is affected.
Without medical supervision, deforming osteoarthritis can develop within 1-1.5 years, leading directly to disability. The hip joint tendon can cause loss of hip and leg rotation ability. Pain in this area can spread to the inside of the leg and up the leg, affecting the lower back.
Free medical advice and diagnosis
During the consultation, we carry out a thorough diagnosis of the entire spine and individual spinal segments. We determine exactly which segments and nerve roots are affected and cause the pain symptoms. Following the consultation, we provide detailed treatment recommendations and prescribe additional diagnostics if necessary.
We carry out a functional diagnosis of the spine
We carry out a manipulation that leads to significant pain relief
We set up an individual treatment program.
tendinosis of the knee
Often occurs in athletes. The classification tendinosis of the knee is diagnosed in track and field athletes, jumpers, volleyball and basketball players. All of these athletes put a lot of strain on their knees. The cruciate ligaments that are most often damaged are those that are completely torn or have minor tears.
Scarring of the tissue during fusion triggers the deposition of calcium salts, causing further damage. The hamstring tendon is manifested by pain when bending the leg and during movements that extend the lower extremity. When you move, you can hear a creak, crunch, or click. Sometimes it feels like the knee joint is blocked and is losing its normal function. Despite the internal changes, the knee has a healthy appearance.
Popliteal fossa and heel tendon
The cause of abnormalities in this area are repeated injuries to the tendon resulting from repeated sprains or bruises. Severe pain in the heel is the first sign. The painful sensations increase when the foot is moved. Long-term tendinosis can lead to functional flat feet. This generally affects the anatomy of the joints in the foot.
The ankle, knee and hip joints also gradually deteriorate. The lesions travel up the spine and eventually deform the lumbosacral spine. Achilles tendonosis is the most sensitive disease. Although the pain impulses are imperceptible at rest, they become unbearable at the slightest attempt to take a step. The diagnosis is most often made in people with flat feet and club feet.
Diagnosis of injury to the subacromial region
How to diagnose an ankle injuryThe initial diagnosis of an ankle injury requires an X-ray or MRI of the foot, followed by a consultation with an orthopedist. As an additional examination, the doctor may recommend a computer tomography of the foot and ankle.
Which doctor treats plantar injuries: If you have symptoms of a plantar injury, your first priority should be to see an orthopedist.
The ankle joint has the functions of flexion and extension. During flexion, the soleus muscle is lowered, which is done by the triceps muscle on the shinbone. This movement is called plantar flexion (flexion of the sole of the foot). The natural range of motion in this position is different for every person. Several muscles control plantar flexion. Any injury to these muscles limits range of motion.
Plantar flexion involves several muscles of the ankle, foot and leg. This includes:
The calf muscle. This muscle runs along the back of the shinbone, from the knee to the Achilles tendon at the heel. It is one of the most important muscles involved in soleus flexion.
supporting muscle. It is one of the muscles of the calf of the hind leg. It connects to the Achilles tendon on the heel. This muscle is needed to push the foot off the ground.
Plantar muscle. This long, slender muscle runs along the back of the leg from the end of the thigh to the Achilles tendon. It works with the Achilles tendon to flex the ankle and knee.
Posterior tibial plateau muscle (tibialis posterior). Located deep in the leg. Runs down the shinbone to the big toe. Helps flex the big toe while walking
Flexor muscle of the long toe. This is another deep muscle of the shinbone. It is initially thin, but becomes wider as the leg progresses. It helps flex all toes except the big toe.
Posterior tibial muscle (tibialis posterior). This is a smaller muscle located deep in the lower leg. It is involved in both soleus flexion and inversion, in which the sole of the foot turns inward towards the other foot.
Treatment
Minor injuries to the soleus muscle are usually treated at home with the following tips:
- Relax
- Ice. Cover an ice pack with a cloth and hold it on the injured area for about 20 minutes.
- Compression. Place an elastic bandage around the injured area.
- Elevate. Prop the injured ankle on a pillow to raise it above heart level.
An ankle injury usually heals within a few days or weeks. More serious fractures require surgery.
Strengthening the ankle, leg and foot muscles that help flex the sole can keep the foot flexible, protect the ankle and prevent injuries. Wearing appropriate footwear will also help prevent injuries. Avoid high heels, especially those that do not properly support the ankle.
How to get rid of the symptoms
Treatment for tingling in the legs depends on the cause of the symptom. If the discomfort and pain are due to venous insufficiency, the following measures are recommended:
- correction of lifestyle;
- avoiding bad habits;
- increasing physical activity;
- use of compression stockings;
- pharmacological treatment.
For severe varices, surgical treatment using safe and minimally traumatic techniques (endovascular venous sclerotherapy) may be indicated. Systemic endocrine diseases (diabetes, thyroid diseases) and autoimmune diseases (rheumatism, vasculitis) require comprehensive treatment, which in turn reduces the severity of paresthesias.
prevention

To avoid paresthesia pain, tingling and heaviness in the legs, it is recommended to lead an active lifestyle, eat sensibly and give up harmful habits. If symptoms of illness occur, it is important to seek medical help in a timely manner and not to resort to self-medication.
If you notice pain, burning or tingling in your feet that does not go away on its own, contact MedProsvet. Our specialists will help you find the cause of your discomfort and create a treatment plan to restore your health and improve your quality of life as quickly as possible!
Why does my heel hurt?
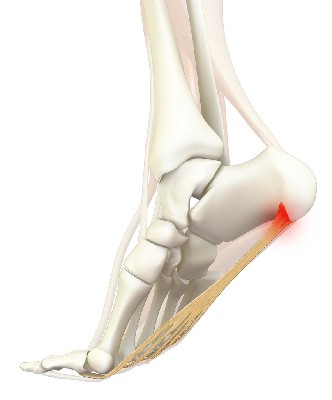
The most common cause of heel pain (about 80% of cases) is plantar fasciitis. This is damage and thickening of the heel fascia, the thick bundle of fibers that connects the heel bone to the rest of the foot. Damage to the heel fascia can occur in the following ways:
- an injury, e.g. B. running or dancing, which is more common in young and physically active people;
- Gradual wear and tear of the plantar fascia (plantar fascia) is common in people over 40 years old.
The risk of gradual wear and tear of the plantar fascia is increased in people who are overweight or obese, in people who spend most of the day on their feet, and in flat-soled shoes such as flip-flops or flip-flops.
With plantar fasciitis, heel pain is more likely to occur after sleeping. After a while they become easier, but by midday, with prolonged walking, the heel pain increases again.
Less common causes of heel pain
heel spur – is a bone outgrowth in the form of a spur in the heel. A heel spur is often a result of plantar fasciitis, but can also develop spontaneously without causing heel pain.
Stress Fracture (Stress Fracture) It is caused by prolonged excessive strain on the heel bone while walking, running, jumping, etc. It occurs more often in people who exercise. Less commonly, it occurs in osteoporosis, when the heel bone loses strength and even simple walking or jogging can cause its structure to deteriorate. A stress fracture is accompanied by a stabbing pain that increases when pressure is placed on the heel. A slight swelling may occur at the fracture site.
Atrophy of the fat pad – Thinning of the fat layer under the heel bone due to excessive pressure on it. The layer of fat between the foot bones and the skin plays an important role as a shock absorber when walking, absorbing the impact on the ground. The risk of developing fat pad atrophy is higher in women who walk in high heels for long periods of time and in older people. In rare cases, fat pad atrophy of the foot occurs after corticosteroid injections into the joints and after bone fractures. Orthotics can help with this cause of heel pain.
Diagnosis of heel pain

To diagnose heel disease, you should see an orthopedist/traumatologist. In most cases, this is the specialist who will take care of your further treatment. If it is difficult to get an appointment with this specialist, you can first contact a surgeon. During the examination, you may need to consult other doctors: a rheumatologist to rule out systemic joint disease and a neurologist to rule out nerve disease of the foot.
There are some additional signs that can help you and your doctor identify the cause of your heel pain. For example, a feeling of numbness or tingling in the foot is more likely to be an indication of nerve damage. This could be the tarsal tunnel syndrome described above or a symptom of general peripheral nerve damage, such as: B. in diabetes. If the foot feels hot and swollen, it may be a soft tissue or heel bone infection. In such cases, the help of a surgeon is required. Restricted movement and pain in the ankle joints indicate the possible development of arthritis - an inflammation of the joint.
Your doctor may recommend the following tests to confirm the diagnosis:
- blood tests;
- X-rays, which use a low dose of radiation to reveal abnormalities in the bones;
- Magnetic resonance imaging (MRI) or ultrasound – methods used to examine the soft tissues in more detail.
Material and methods.
Between 2005 and 2017, 37 patients with long-standing Achilles tendon rupture were treated in the No. 1 Trauma and Orthopedic Department of Samara State Medical University Hospital. The diastasis between the ends of the Achilles tendon in the neutral position of the ankle was more than 10 cm. Due to retraction of the triceps muscle, the tendon cannot be closed through, requiring repair of the diastasis between the distal and proximal ends.
Group 1 (control) included 21 patients who underwent autoplasty with reverse flaps (according to Chernavsky, Krasnov) and VY-plasty. Group 2 consisted of 16 patients who underwent the new surgical treatment we proposed [4]. In all patients of the main and control groups, there was a significant difference (more than 4 cm) in the circumference of the symmetrical areas of the upper third of the tibia, indicating pronounced hypotrophy of the triceps muscle. The two groups were comparable in age, gender, mechanism of injury, and time of referral to the Department of Traumatology and Orthopedics No. 1 of the Samara State Medical University Clinic, where surgical treatment was performed.
Before the operation, the patients were examined in the biomechanics laboratory of the SamSMU clinic (electromyography, podometry, measurement of foot flexion strength) and ultrasound diagnosis of the injured area was performed.
The team of authors from the Department of Traumatology, Orthopedics and Extremity Surgery of the Samara State Medical University. AF Krasnov, Russian Academy of Sciences. RAS AF Krasnov received Russian patent No. 2537888 dated 11/13/14 for the invention of a new method of surgical treatment of patients with chronic Achilles tendon rupture with pronounced diastasis of its ends (more than 10 cm), in which the tendons of the short fibula and the posterior The shin muscle can be moved to the distal end of the Achilles tendon under optimal tension [4].

The proposed method is presented graphically. Figure 1 shows the proximal (1) and distal (2) ends of the Achilles tendon. The tendon (3) of the short fibula (4) is selected and held. The tendon (5) of the posterior tibialis muscle (6).
Results
Treatment results in control patients (n=21), who underwent plication of the Achilles tendon defect (according to Chernavsky, Krasnov, VY-plasty), we found that the strength of the soleus flexor muscles (Lovett scale) on the injured side was on average 3.43 points, compared with 4.63 in the control group. Muscle strength 5 in the main group had 62.5 % of patients and 14.3 % in the control group.
In the analysis of the podometric indices, features of step timing such as the duration of the double step, the time of foot transfer, the duration of single and double landing, and the order of contact between the foot part and the support were examined. Individual limbs were compared using the subjects' gait asymmetry index, which was defined as the ratio between longer and shorter support times minus one multiplied by 100 %. Based on this ratio, gait asymmetry up to 5 % was considered normal, 5 to 10 % was considered latent claudication, and above 10 % was considered overt claudication.
Gait asymmetry up to 5° was 81.25 % in the main group and 14.3 % in the control group. A gait asymmetry of 5-10 % was 18.75 % in the main group and 71.43 % in the control group. There was no asymmetry over 10% in the main group and 14,27% in the control group.
The results suggested that the main group had the best gait performance.
As the determined functional indices show, the control group patients had a significant decrease in the strength of the plantar flexor muscles on the injured side and persistent gait asymmetry in the late postoperative period. The fact that even a high-quality Achilles tendon defect replacement (plication) cannot completely compensate for normal active flexion at the ankle joint with significant hypotrophy of the triceps tendon was the reason for the development of the new method.
What is the cause of foot pain?
Pain in the soles of the feet, under the toes and elsewhere can have many different causes, including injuries, deformities, unsuitable footwear, viruses and illnesses. Injuries caused by external factors
A common cause is a misalignment of the foot, which leads to a disruption in the vector forces acting on it. Wearing shoes with stiff bottoms or high heels, or shoes with heavy lacing, can also cause bruises at the pressure point, often causing pain in the bunion area under the big toe and elsewhere.
Ligament and muscle strains and fractures
These usually occur suddenly. They lead to tension in the foot muscles. Ankle sprains occur when the ligaments that hold bones together are strained and their fibers are overstretched. A weakening of the ligaments in the joints causes the padding on the foot under the big toe to hurt when walking.
Overstretched, bruised or torn muscle
These occur, for example, when you hit something with a sharp object. This causes the muscular skeleton and fascia of the foot to be overloaded. This can cause pain in the big toe and other areas of the foot when walking. Various diseases can be diagnosed. Achilles tendonitis is an injury to the tendon that attaches to the heel bone at the back of the heel. Metatarsalgia is a pain that occurs under the heads of 2-3-4 metatarsals.
Pressure injuries or injuries caused by sudden withdrawal of the foot. Can cause stress damage to bones and joints. Blunt pressure trauma, e.g. B. when someone steps on your foot, cause damage to muscles and ligaments. This leads to pain in the sole of the foot near the toes and other areas.
Direct trauma caused by a blow to the foot can cause bruises, skin injuries, and even broken bones.
Metatarsalgia is a pain that occurs under the heads of 2-3-4 metatarsals. Nail trauma can result in the accumulation of a hematoma under the nail and temporary or permanent loss of the nail. Repeated trauma to bones, muscles, and ligaments can result in bony and cartilaginous growths called spurs or exostosis.
Poorly fitting footwear
Footwear can also be a source of pain in the lower limbs. Wearing tight-fitting shoes for short periods of time can cause abrasions, blisters and chafing on the feet, causing pain when stepping on the balls of the feet. Prolonged wearing of these shoes causes bunions, hyperkeratosis, nerve and joint irritation, toe dislocation and micro-injuries. If foot pain occurs, you should see a podiatrist immediately.
Warts are usually located on the surface of the soles and can cause irritation and pain when exerted. They are caused by viruses.
A common cause of foot pain in the big toe area is an ingrown toenail. It causes irritation and sometimes triggers an infection.
Diabetes mellitus, Hansen's disease and gout are common diseases that affect the lower limbs. Diseases of the nerves in the legs can cause numbness and a burning sensation; this is called peripheral neuropathy.
Read more:- shin tendinitis.
- Tendon of the tibialis anterior muscle.
- Heel bone tendon sac in Latin.
- Lamb Muscle Soreness.
- shin tendon.
- Triceps femoris muscle.
- Tibialis posterior muscle.
- Long fibula muscle.
