This condition is treated by a neurologist.

- Treatment of longitudinal flatfoot with Kalix implants
- Indications and contraindications for Kalix subtalar arthroplasty
- Advantages of technology with modern implants:
- How can external signs indicate an indication for surgery?
- How is it diagnosed?
- information
- sources and literature
- information
- Rehabilitation process
- Reviews and effectiveness
- For practitioners
- Dislocated shoulder
- Causes of ankle ligament injuries
- Types of ankle injuries
- Types and degrees of joint instability
- Symptoms of joint instability
- Tarsal Sinus Syndrome – Cure
- conclusion
Treatment of longitudinal flatfoot with Kalix implants
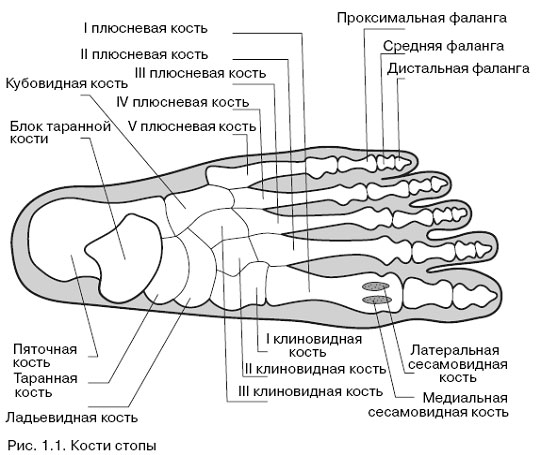
Walking is a complex cyclic movement that uses a variety of muscles in the shoulder, pelvic girdle, and lower limbs. The foot, the distal segment of the lower limbs, has supportive, resistant, balancing and elastic functions during walking. The latter function ensures a smooth gait by absorbing the shock of the body when walking, running and jumping. This function is realized by the arch structure of the foot.
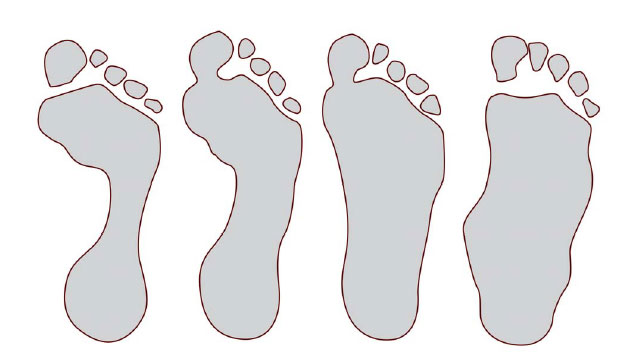
Flat foot is a deformity of the foot characterized by a flattening of the longitudinal and/or transverse arch. Longitudinal flatfoot in children accounts for about 75 % of all forms of flatfoot.
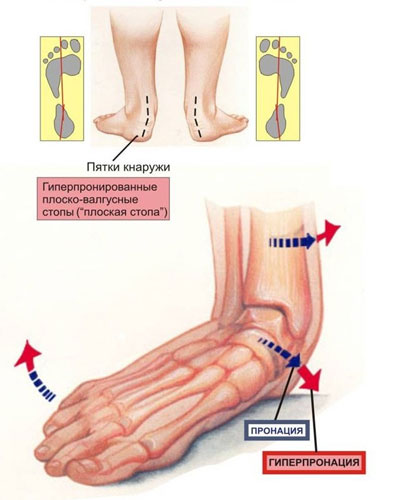
The clinical picture of longitudinal flatfoot is characterized by a reduction in the height of the longitudinal arch of the foot, which is clearly visible on the plantogram as a reduction in the space between the feet, a valgus deviation (internal deviation) of the hindfoot and an external deviation of the forefoot. The inner part of the foot is overloaded, which leads to overloading of the tibialis anterior and posterior muscle groups involved in maintaining the longitudinal arch, which is manifested by rapid fatigue when walking. In addition, the flattening of the arch of the foot leads to compression of the supporting nerve by the head of the heel bone, causing pain on the inner surface of the sole of the foot. The reduced cushioning of the foot also leads to impaired function of the knee and hip joints as well as the spine.
Conservative treatments such as massage, physical therapy, and orthotics are usually aimed at preventing progression of the deformity and improving the strength and muscular endurance of the affected muscle groups. Experience shows that it is not possible to completely eliminate the deformity using conservative means.
Indications and contraindications for Kalix subtalar arthroplasty
The main indication for this technique is:
- Longitudinal dysplastic flatfoot in children and adolescents;
- Congenital flat feet;
- Ineffective long-term conservative treatment (shoes, orthoses);
- Instability of the supporting joint;
- Deformities with insufficiency of the posterior tibialis muscle.
Contraindications include:
Advantages of technology with modern implants:
- Reducing pain symptoms and foot and leg fatigue.
- Low risk of infectious complications
- Does not require immobilization (walking on crutches) Bone or cartilage is removed
- No holes need to be drilled in the bone to insert the prosthesis
- No bone cement is required for fixation
- The implant can be removed if necessary.



How can external signs indicate an indication for surgery?
If the condition of your feet does not improve with age or continues to worsen with conservative treatment, you should consult your podiatrist for advice. Your doctor will recommend flat foot correction surgery because it will help eliminate your pain, allow you to lead a more active life, improve your quality of life, and avoid more complex surgeries in the future.
The implants do not need to be removed. However, some patients may experience persistent pain, which may be a reason for implant removal.
How is it diagnosed?
Synovitis of the ankle joint needs to be treated in a timely manner, so you should consult your doctor as soon as the first symptoms appear. The doctor asks the patient about the symptoms and collects anamnestic information to determine risk factors. He examines the affected limb and feels it. It assesses the severity of the impaired motor function of the joint.
To make a diagnosis, the following tests must be carried out:
Visualization. Depending on the indication, the doctor orders X-rays, ultrasound, CT or MRI.
Puncture of the joint. An ultrasound device is used to insert a needle directly into the joint cavity to obtain a fluid sample and further examine the material in the laboratory.
Laboratory diagnosis: biochemical and general blood tests, as well as serological tests to identify the infectious agent.
MRI is the most reliable imaging method that allows the doctor to obtain high-resolution images of the anatomical structures layer by layer.
information
sources and literature
- Minutes of meetings of the Joint Commission on Health and Consumer Protection. Quality of medical services of the Ministry of Health of the Republic of Kazakhstan, 2018.
- 1 Tamoev SK Subtalar arthroeresis as a method for correcting static flatfoot deformity in adults // Proceedings of the 14th Russian National Congress 'Man and his health', 20-23 October 2009.-C19. 2 Zagorodniy NV, Protsko VG Subtalar Arthroeresis in posterior tibial tendon dysfunction of II degree // Proceedings of the 14th Russian National Congress 'Man and his health', 20-23 October 2009. 3 Dubovik GO. Osteotomy of the calcaneus in the complex treatment of static flatfoot deformities in adults // Proceedings of the 5th Congress of Traumatologists of the Republic of Armenia, 1-3 October 2010. 4. sultanov EM, Zagorodnyi NV, Khamokov ZH Subtalar arthroresis for posterior tibial tendon dysfunction // Vestnik Traumatologii i Ortopedii im. Приорова.-2011.-№1.-С.15-19. 5. Eidelman M., Katzman A.,Treatment of the arthrogyotic foot with the Taylor space frame // Pediatr.Orthop.2011.Vol.31, No4.S.429-434. 6. Butaev VG Modern methods of surgical correction of flat valgus foot deformity in patients with os tibiale externum / / Traumatology and Orthopedics of Russia -2011.-№2.- P.70-75
information
List of protocol developers:
- Tazhin Kairat Bolatovich – MD, PhD, Head of the Department of Orthopedics ¹2 RGP at PCV 'Research Institute of Traumatology and Orthopedics';
- Sultangereev Aslan Bakhytovich – Candidate of Medical Sciences, Head of the Center for Polytraumatology, Endoprosthetics and Kombustiology of the RGP at PCV 'City Hospital № 1' akimat Astana;
- Akhmetzhanova Gulmira Okimbekovna – clinical pharmacologist RSE at the PCV 'Scientific Research Institute of Traumatology and Orthopedics'.
Reviewer:
Mukhtar Tolegenovich Abilmazhinov – MD, PhD, Professor, Head of the Department of Traumatology and Orthopedics, JSC 'Medical University of Astana'.Rehabilitation process
After arthrosis, special orthoses must be worn for the first three months. The insoles are made according to individual parameters. It is recommended not to put strong pressure on the legs in the first postoperative period. The implant inserted is only temporary. Once the problem is resolved, it will be removed again. Most often this happens after 1-1.5 years.
In children, however, this point is often postponed until the age of 18 because the musculoskeletal system does not fully develop until adulthood. If the device does not cause discomfort, it is left in the leg.
Reviews and effectiveness
Numerous reports show that subtalar arthrosis delivers excellent results. As a rule, the procedure does not cause any complications. Therefore, it is actively used to eliminate flat feet in adults and children.
The cost of the procedure depends on the clinic and the qualifications of the doctor. Today the price of surgical intervention is 20-30 thousand rubles per limb. This amount does not include the cost of the implant.
If the operation is supplemented by tendon plasty, an additional fee of 11-58 thousand rubles will be required. The exact amount depends on the complexity of the disease. The operation can be performed at the age of 9-10. If necessary, it can also be carried out at other ages.
Since ankle arthrodesis is a minimally invasive surgical procedure, there are practically no restrictions. If you have serious somatic illnesses, you should consult a doctor. For acute viral infections, surgery should be postponed until recovery.
Ankle arthrodesis is a minimally invasive procedure that has a high success rate and does not require complex and lengthy rehabilitation. This surgery can control flat feet and avoid dangerous complications.
See how subtalar joint arthrodesis is performed in our video:
For practitioners
Dear colleagues, just because something doesn't work under local anesthesia doesn't mean you've done something wrong. It doesn't mean you are a bad practitioner. It just means that the patient's muscles are stronger than your hands. Also, there are certain types of dislocations that can only be repaired in the only conservative way possible, and if you don't know that, it won't go away no matter how much effort you try. You have to operate. I personally observed a doctor with decades of experience suffering from a similar dislocation. And I was lucky, I knew how to do it. And that doesn't mean he's a bad doctor. And I might not be good at something else. And then there is Kaplan (for example here) [AV Kaplan, Bone and Joint Injuries, 1979. 428 p.]It's ancient, but useful. Not much has changed on this issue since the days of Hippocrates (apart from anesthesia, of course). There are many books online, here are the links. doc_zlo a whole bunch of them. I invite you to read them, it's completely normal. Patients are somehow convinced that we know everything, and we know very little. This is how we learn throughout our lives.
Dislocated shoulder
The most common dislocation in nature. 50-60 % of all dislocations [Traumatology and Orthopedics: Guidelines for Doctors / Edited by NV Kornilov: In 4 volumes - St. Petersburg: Hippocrates, 2005 - T.2 - P.54]. (Note – statistics from this source here and below). У morita The mechanism is described in great detail - falling on the shoulder. The position of the arm afterwards is called 'forced'. Every movement causes pain. The patient turns his entire body around the suffering arm and tries to find a comfortable position. It must be transported as it is and try to fix the arm in the position in which it is.
There are anterior-posterior dislocations (the vast majority) and posterior dislocations (rare but not uncommon) in which the head of the shoulder lies behind the socket of the scapula (also called horizontal dislocation). There are other forms (according to Kaplan's classification), but they only occur sporadically. Shoulder dislocations can have the following consequences complications Compression of the neurovascular bundle by the humeral head. This can lead to (a) traumatic plexitis (or brachial plexopathy), in which the hand becomes numb and loses mobility (due to compression of the brachial plexus), a complication that may require very long (months-long) treatment by a neurologist; and (b) compression of the axillary artery (fortunately rare), which in extreme cases (almost casuistically) can lead to gangrene of the hand if the dislocation is not quickly reversed. The latter can also manifest itself as numbness in the hand, albeit gradually and primarily due to the absence of a pulse in the usual location (on the radial artery).
Causes of ankle ligament injuries
Ankle ligament injuries are not accidents. They are the result of the presence of numerous risk factors. Their pathogenic effects can affect the integrity of various tissues.
The ankle joint is quite complex. It is composed of three bones. At the tip are the distal ends of the tibia and fibula. They are connected to each other by a cartilaginous anastomosis. If this anastomosis breaks, the entire joint deforms. From below, the joint is formed by the talus bone. This bone forms another joint with the heel bone - the subtalar joint.
The joint is surrounded by a dense joint capsule containing synovial fluid. There are ligaments and tendons nearby. The ankle joint is involved in walking, running and jumping. It takes on some of the burden of shock absorption.
Damage to the ankle ligaments is very likely in people with the following risk factors:
- Excessive body weight – each additional kilogram increases mechanical pressure on the articular surfaces;
- sedentary lifestyle - the muscles surrounding the ankle joint are not fully functional and do not supply the ligament fibers;
- strenuous physical work involving constant standing, lifting and carrying loads;
- disturbed metabolic processes in the body;
- Impairment of blood supply to the lower limbs, usually obliterative arteritis, varicose veins of the lower limbs, atherosclerosis, vasculitis, diabetic angiopathy, etc;
- unsuitable footwear for daily wear and sports;
- Flat feet, clubfoot and other types of foot abnormalities;
- deformed arthrosis of the knee and hip joints;
- Postural abnormalities and curvature of the spine, leading to disruption of the uniform distribution of shock loads and an increased risk of destruction of the anastomosis between the tibia and fibula;
- Valgus or varus deformities of the tibia, big toe, etc.
Types of ankle injuries
There are many different types of ankle injuries. A closed ankle injury is, for example:
- Dislocation of the ligamentous apparatus (or microscopic tears in its fibers);
- Dislocation of the distal condyles of the tibia and fibula with tear of the cartilaginous anastomosis;
- Achilles tendon injury;
- Damage to the soleus ligament and development of fasciitis;
- Formation of a bony tip (outgrowth) on the heel bone (heel spur);
- Fracture of the heel bone (often caused by a fall on the heel from a height);
- Fractures and fractures of the distal ends of the tibia and femur;
- the penetration of blood into the joint cavity and the development of hemarthrosis.
Any injury, even partial, to the ankle ligaments requires intervention by a trauma surgeon. If the patient is not treated and rehabilitated in time, a ligament rupture may soon occur. Such a patient can only be helped by a surgeon. Surgery is required to repair the damaged ligamentous apparatus. After the operation, a long rehabilitation period is required.
Types and degrees of joint instability
Depending on the damaged joint, instability of the shoulder, elbow, knee and other joints occurs. Depending on the degree of damage, a distinction is made between:
- 1st degree – there is structural damage of less than half the fiber volume, with the overall integrity of the ligament remaining intact.
- Grade 2 – more than half of the fibers are traumatically damaged and the ligaments are torn. The injured joint is restricted in its movement.
- Grade 3 – the ligaments are completely torn and the joint is pathologically mobile. At this stage, instability is often accompanied by damage to the adjacent structures such as cartilage, meniscus and joint capsule, as well as simultaneous damage to the ligaments (e.g. the cruciate and collateral ligaments in the knee joint).
Symptoms of joint instability
Symptoms directly depend on the type of joint, the type of damage, the load and the function of the joint. In general, an unstable joint can manifest itself as follows.
- Local swelling of the soft tissues.
- Pain, especially under strain and with violent movements.
- A feeling of instability (e.g. an unstable knee joint).
- Excessive mobility and laxity of the joint.
- Visible enlargement of the joint.
- Over time – muscle loss, inability to perform powerful movements.
Tarsal Sinus Syndrome – Cure
Recovery can often take several weeks using conservative methods. Even people who have had surgery usually need a few weeks to recover. In some cases, it may take up to three months to return to exercise and six to 12 months to fully recover.
The type of surgery may affect recovery time. For example, during flat foot surgery, the foot must not be put under any weight for 6 to 8 weeks after the operation. Recovery can occur within 10-12 weeks. After 12 weeks, the affected person can switch to normal shoes, but must immobilize the ankle and use walking and mobility aids. Full recovery often takes 1-2 years. After an operation to stiffen the ankle, those affected can wear shoes for around 8-12 weeks.
In any case, those affected must follow the surgeon's and physical therapist's recommendations on how to care for their foot and when they can exercise again. Failure to follow these recommendations may increase recovery time and result in further or worse injury.
There is also some risk of surgical complications, including infections, failed operations, and pain.
Sinus-tarsal syndrome often causes:
- Pain or discomfort on the outside of the foot, usually behind and below the ankle
- Swelling around the ankle and heel
- Instability and worsening of symptoms when standing, walking or putting pressure on the ankle
- symptoms do not improve over time
- Immobilization doesn't help
- the pain is severe and interferes with daily life or activities such as sports, work or study
An orthopedic trauma surgeon will evaluate the patient's symptoms and order additional imaging tests to determine the cause of the pain and rule out other possible causes, such as a cyst or tumor. If the doctor diagnoses sinus syndrome, he or she will recommend treatments to help the sufferer recover.
conclusion
Tarsal sinus syndrome usually manifests itself as pain and swelling below the ankle joint on the outside of the foot. It is often caused by trauma, such as: B. due to a sprain of the ankle ligaments.
Initial treatment includes conservative measures such as NSAIDs, orthoses and medication. If conservative treatment doesn't work, your doctor may recommend surgery. Surgery can correct flat feet, remove damaged tissue, or join the joint together. Recovery often takes a few weeks, but surgery can extend the time it takes to return to normal activities.

Doctor of diagnostic ultrasound at SZDCM (St. Petersburg)
Founder of the online publication Medical insiderEditor-in-chief and author of articles.
- dislocation of the ankle.
- Diagram of a joint with and without a dislocation.
- Ankle ligament sprain.
- Treated subluxation of the ankle.
- Rupture of the ligaments of the ankle.
- This is what a dislocated leg looks like.
- How do you treat a sprained ankle?.
- How much does shoulder dislocation surgery cost?.
