There used to be no hurry to tie off and cut the umbilical cord. The severed placenta was hung over the newborn's cradle, allowing all of its blood to flow through the umbilical cord into the baby's bloodstream. The umbilical cord was cut when it started to dry out on its own. Or it was tied off and allowed to dry out and fall off.

- postoperative period
- compression therapy
- care of the stump
- Further information
- Gangrene Rescue Center
- QUESTIONS AND ANSWERS
- Care of the umbilical cord stump
- care of the umbilical cord
- What Happens to the Umbilical Cord: Phases
- What can go wrong?
- Psychological counseling accompanies the patient throughout the rehabilitation program.
- polyneuropathy
- Phantom Pain Syndrome
- Rules for sport after a leg amputation
- Application of massage treatments
- How to care for the stump
- What does the patient have to consider during care?
- How do you properly massage a residual limb?
- General information.
- Care after skin grafting
- How do I change a patient's colostomy bag?
- Prevention and treatment of peristomal dermatitis
postoperative period
The rehabilitation process after an amputation takes up to six months on average. Your primary focus will be preparing the residual limb for the prosthesis. You should also be aware that the suitability of the residual limb for a particular prosthesis design is highly dependent on the postoperative musculoskeletal condition, which in turn is highly dependent on the type of procedure and underlying or comorbid conditions. This should be discussed with your doctor.
An amputation is a serious event that brings about significant changes in a person's life. Thanks to technological advances, amputees can now go on with their lives and maintain their social status despite losing a limb. However, a properly shaped residual limb and a suitable prosthesis are essential to achieve this goal. Some postoperative complications can make prosthesis fitting very difficult and in some cases even impossible. These complications include non-healing ulcers, surgical site infections, circulatory and sensory disturbances, and phantom limb pain. This also applies to residual limb deformities as a result of the complications described, as well as limited mobility (contracture) due to prolonged immobility and muscle weakness.
During the rehabilitation period, the patient must always follow the recommendations for the care of the postoperative suture, the formation of the stump, the preservation of joint mobility and the strengthening of the remaining muscles.
The disappearance of pain is a prerequisite for the transition to subsequent rehabilitation measures. Pain caused by surgery and tissue trauma usually subsides as the surgical wound heals if properly managed.
However, amputation can cause another type of pain unrelated to tissue trauma: phantom limb pain, which is sometimes difficult to treat with medication.
compression therapy
The most important problem to solve is the swelling that develops after the operation. The swelling is the body's natural response to surgery and usually subsides after 1-2 weeks. During this period, bandages and primary prostheses are used to reduce swelling. In the case of non-edematous edema, among other things, lymphatic drainage massages by an experienced specialist and the use of an elastic bandage or tourniquet are recommended.
An elastic bandage is the traditional treatment for edema. The bandage is first applied by the medical staff and then guided by the patient or their relatives, since it can also be applied at home. A bandage that is too loose will not have the desired effect, and a bandage that is too tight (it is not taut at the end of the residual limb but compresses it higher up) can damage the tissue.
An elastic bandage is useful in the management of edema, but not as effective without the other complex aspects of residual limb care. In addition, in the absence of regular movement, the bandage can cause spasticity in the knee joint and the development of contractures.
care of the stump
rescue the stump
high-tech methods
- Vascular and cardiovascular diseases
- Dry gangrene
- critical ischemia
- Diabetic foot
- Atherosclerosis and its treatment
- Obliterating arteritis
- Arterial thrombosis and embolism
- Popliteal artery aneurysm
- Removal and dissolution of thrombi
- Carotid artery surgery
- Aortic Femoral Bypass Surgery
- Carotid artery stenting
- Microsurgical shunts on the lower leg and foot
- angioplasty and stenting
- amputations due to gangrene
- High risk surgery
- Treatment of ulcers and bedsores
- Clinical examination
- ultrasound examination
- Computed Tomography
- Subtractive angiography
Further information
Hand and body strengthening exercises are best started before the amputation. They promote the skills necessary to move from bed to wheelchair, go to the toilet and maintain the fitness for learning to walk, which is done with or without prostheses.

Gangrene Rescue Center
Moscow region, Klin city, Pobedy street, ld. 2
QUESTIONS AND ANSWERS
My husband has to be amputated at the waist - they say there is no chance. Burger's disease. Terrible pain. Gangrene of the foot. They gave vasoprostan drops for three weeks. They said there is no chance.
Answer: This is our profile. Please send photos of your foot and a discharge form to [email protected] and we will try to help you.
Hello, I am on hemodialysis, my fistula was sewn up incorrectly, there was a bandage and the toe could not be saved, gangrene had formed. It was possible to restore blood flow, but I was sent home to St. Petersburg to await spontaneous amputation. Now he is gone.
Answer: Yes, we can solve everything. The cost of treatment is 190 rubles.
Hello, my mother is 79 and they had 2 toes amputated but the gangrene has spread to half of the foot, the doctors say she needs an amputation above the knee. She had vascular surgery, but it wasn't done to the knee.
Answer: Send a photo of the foot and vascular data to [email protected]. Maybe we can save the foot from amputation.
The possibility of reconstructive surgery on the arteries of the left renal pelvis with signs of small-spot hemorrhagic erosions on endoscopic examination.
Can you tell me in which cases the shunt closes so soon after surgery and what are the next steps? Will another operation be required? Thank you very much for your answer
Answer: If the condition recurs, blood flow must be restored.
Hello, I had bypass surgery on my leg 3 months ago. After the operation I felt better. The leg is cold again and hurts as before. What can be the reason?
Care of the umbilical cord stump
The umbilical cord can be clamped shortly after birth or later. In many cultures, people believe that all life from the placenta must be passed to the newborn or the baby could die. Therefore, the umbilical cord is usually cut after it has stopped pulsing or after the placenta is delivered. This practice is harmless and may even be beneficial for the baby.
Late clamping, after the umbilical cord has stopped pulsating, is a common procedure in traditional out-of-home deliveries, and early clamping is common in healthcare settings. Timing of umbilical cord clamping can affect both mother and child. Rh-negative women should avoid early cord clamping as it increases the risk of fetal blood transfusion. However, the possibility of free bleeding from the placental end of the umbilical cord reduces this risk. Delayed clamping of the umbilical cord leads to blood transfer from the placenta to the child. The amount of blood transfused varies between 20 % and 50 % of the newborn's blood volume, depending on when the umbilical cord is clamped and the height at which the child is held prior to clamping. If the newborn is placed on the mother's stomach or on the bed she is lying on, and the umbilical cord is clamped only when it stops pulsating, the blood volume of such a baby is 30 % higher than in babies whose umbilical cord is directly connected was clamped after birth. The transfusion of blood from the placenta occurs at about 80 % within 1 minute and is almost complete after 3 minutes.
The umbilical cord should always be tied or clamped before cutting, otherwise excessive bleeding may occur. A sterile and sharp instrument is usually used to cut the stump of the umbilical cord, e.g. B. a new scalpel blade or surgical scissors. The recommended length of the residual limb after cutting is usually 2 or 3 cm. Some authors recommend clamping the umbilical stump 3-4 cm from the abdominal wall to avoid pinching the skin or pinching part of the intestine, which in very rare cases may be located in the umbilical stump. A long stump can increase the risk of infection because it's harder to keep clean and dry.
care of the umbilical cord
Umbilical cord care during and after birth is an effective way to prevent umbilical cord infections and neonatal tetanus. Methods for maintaining a clean umbilical cord after birth include washing hands with clean soap and water, placing the newborn on a clean surface, and washing hands again before touching the umbilical cord. Postnatal cord care includes washing hands with clean water and soap before and after care, and keeping the cord dry, either exposed to air or loosely covered with clean clothing.
If necessary, the umbilical cord should be washed with clean water and soap (cleaning with alcohol or antiseptics will delay healing), and the diaper should be folded over so that the stump is exposed to air. Avoid touching the atrophied limb with your hands, soiling it with feces, and applying bandages.
Other methods that can reduce the risk of umbilical cord infection include 24-hour skin-to-skin contact with the mother after birth, which encourages colonization of the newborn with non-pathogenic bacteria from the mother's skin flora. Early and frequent breastfeeding provides the newborn with antibodies.
There is insufficient evidence to recommend the widespread use of topical antimicrobials on the umbilical cord stump. The decision to use depends largely on the local conditions. In hospital settings, for newborns in the neonatal unit or intensive care unit, it is probably best to apply a topical antimicrobial to the umbilical cord stump after birth and for the first three days to prevent umbilical cord colonization with pathogenic bacteria and cross-infection to prevent.
The choice of agent depends on the prevailing hospital flora (usually S. aureus, but sometimes gram-negative organisms). If the pathogen is not known, an antiseptic with a broad spectrum of activity should be chosen. If the mother is the primary caregiver, the use of antiseptics is probably not necessary as the risk of umbilical cord infection is much lower.
What Happens to the Umbilical Cord: Phases
Every day, parents can see how the remnant of the bond between mother and child changes throughout pregnancy and minutes after birth.
- The rest of the umbilical cord gradually dries up and becomes smaller and smaller.
- First it thickens, then it darkens and takes on a dark brown color.
- One day it falls off and the parents see a fresh pink epithelium at the bottom of the umbilical wound.
- After a while, all that remains is the most beautiful belly button in the world.
What can go wrong?

Sometimes an infection like Staphylococcus aureus, E. coli and other bacteria can get into the umbilical wound. This increases the risk of inflammation – omphalitis. This disease can take various forms: simple omphalitis, phlegmatic and necrotizing inflammation. Treatment of the latter requires hospitalization in a surgical department.
Sometimes a misshapen tissue forms around the umbilical wound, which can be frightening to look at. But you don't have to worry: this is what is known as an umbilical granuloma. Your doctor will help you remove the granuloma quickly and painlessly.
If the umbilical stump or umbilical wound leaks a yellowish, greenish or bloody liquid, sometimes with an unpleasant smell, it is advisable to seek immediate medical attention.
The child's temperature, swelling and redness in the navel area should be a cause for concern. The baby becomes anxious and cries when the navel area is touched.
However, a clean, dry scab should not be a cause for concern; he is normal

In some countries where medical care is still poor, the infant mortality rate, including from umbilical cord infections, is still high. This is largely because the umbilical cord is cut with improvised tools, and in some places even more brutal methods are employed. For example, it can be severed by the midwife or by the mother herself. Sometimes the umbilical cord is cut with a sharp stone or kitchen knife without prior treatment.
In more developed countries, it is customary to perform all manipulations on the umbilical cord using sterile materials and instruments.
Opinions differ on how to treat the umbilical cord. You can either cut it in the hospital or wait for it to fall off on its own (the preferred option).
Psychological counseling accompanies the patient throughout the rehabilitation program.
polyneuropathy
Polyneuropathy is a classic complication of chemotherapy. It is accompanied by general symptoms such as weakness in the arms and legs, numbness, tingling and burning in the hands and feet. She is known as. 'Glove and sock syndrome', ie reduced superficial, vibrational and joint-muscular sensation.
– Depending on the dose of chemotherapeutic drugs, we offer patients magnetic therapy on the limbs and a special complex of therapeutic physical exercises to combat this problem,' explains Anton Andreevich. – We cannot cure all cases of polyneuropathy, but we are able to help patients get used to the problem so that they can avoid injuries in the future.
Phantom Pain Syndrome
Phantom pain syndrome is a consequence of limb amputation. It may present as severe pain, or the person may feel that the amputated leg or arm is being pinched, or feel a burning or tingling sensation in the area.
– Phantom pain syndrome is a chronic condition and directly depends on the psycho-emotional condition of the person affected, explains Anton Andreevich. – According to various sources, between 50 and 80 percent of patients suffer from phantom limb pain. However, in our country there are very few specialists dealing with this syndrome. In our center we treat this pathology with mirror therapy. A clinical psychologist places a mirror in front of the patient, in which he sees the reflection of his healthy limb, and teaches him neuromuscular relaxation techniques. If phantom pain syndrome occurs at night, the patient can use this technique himself and relieve the attack. We also use transcranial electrical stimulation to stimulate the production of endorphins and serotonin. This is a physiotherapy procedure that is not contraindicated in cancer patients unless they have brain metastases.
Rules for sport after a leg amputation
During sports, the residual limb must be protected from contamination and trauma. A soft cloth blanket should be placed over the residual limb so that the foot is well ventilated.
If the surgical sutures become detached, redness and irritation occurs, a doctor should be consulted immediately.
Crutches and canes are height-adjusted and must be as easy and comfortable to use as other mobility aids.
Incorrectly adjusted supports lead to poor posture and limping. Excessive pressure from crutches on the armpit area can lead to inflammation of the lymph nodes and, in particularly difficult cases, to paralysis of the arm muscles.
Practice in front of a mirror and make sure you have good technique and balance.
secondary prosthesis A secondary prosthesis is made when the residual limb is reduced, otherwise adjustments need to be made. A fixed prosthesis is made to more closely resemble a real limb. These prostheses can be modular (consisting of several parts) or non-modular and must meet the weight and safety requirements of the patient.
Rehabilitation after an amputation takes time and a lot of effort, both physical and mental. The most important thing is to follow the recommendations of the doctors and nurses and not to do without the support of the relatives.
Application of massage treatments
Massage treatments are very helpful for the recovery process as they stimulate blood circulation in the tissues and thus prepare the limbs for further fitting with prostheses. Massages can begin at the end of the second week of a rehabilitation vacation.
It begins with a simple stroking, rubbing, or stroking with all the fingers of both hands.
Danger! The pressure must not be too strong and the movements should be gentle, evenly spaced and undulating.
This helps reduce swelling. Light pinching, stroking, spiral rubbing and gentle rolling should be used for better resorption of the surgical scar tissue.
Immediately after the sutures are removed, when the swelling has subsided, sharper and rougher techniques can be used to train the strength of the stump: intense rubbing, finger pressure, tapping and tapping.
How to care for the stump

Any experienced doctor wants to do whatever it takes to save the stump. However, in practice, there are cases when amputation is necessary and surgery is required.
Only if the residual limb is properly cared for after the removal of the segment, part of the leg or arm, can the patient recover as quickly as possible. With appropriate rehabilitation, the patient's quality of life can be maintained.
What does the patient have to consider during care?
Immediately after discharge from the hospital, the patient has to make significant changes in his lifestyle. The stump should be washed with warm water and a special soap solution every evening and every morning. Special care should be taken when washing scars and skin folds. All hygiene measures end with thorough drying of the residual limb and the obligatory application of care products.
You should learn how to perform massages in the first few days. This is the most effective prevention against swelling. Once the wound has healed, you should spend about ten minutes daily massaging the residual limb itself. This starts with the bottom and ends with the top stump. To avoid discomfort during the procedure, use talcum powder, which dries the skin and facilitates movement. In this way, possible irritation caused by friction is avoided.
How do you properly massage a residual limb?
- Fingers and hands are used to stroke;
- the skin is rubbed in a circular motion;
- Gentle pressure is applied to the muscles with fingers and palms;
- Rub the stump with the palm of your hand;
- Adjust the intensity of the movement and pressure to how you feel;
- Finish the massage with gentle strokes so you can relax.
General information.

The transplant surgery is called dermatoplasty. Surgical intervention is indicated for the treatment of burns and extensive wounds in victims of all ages, as well as in many other cases:
- burns;
- wounds, including postoperative wounds;
- Diabetic foot with associated ulcers that do not respond well to conservative treatments;
- Operations related to limb defects and elephantiasis.
Skin grafts are contraindicated in fever, wound infection, and decompensated somatic diseases. The material for skin grafts can come from 3 sources:
- patient or donor skin;
- animal skin, after special treatment;
- artificial materials made from biological polymers and cell coatings.
The choice of material depends on the clinical indications and its availability. According to the classification of dermatoplastic surgery, the following types of interventions are distinguished:
In dermatoplasty, the patient's own skin is used. It is performed when the skin loss affects no more than 35-50 % of the body. A thin layer of skin is removed from a healthy part of the back or leg and transplanted to the damaged area.
With this method, the rehabilitation process is particularly difficult. According to studies, up to 10 % of first-degree burns, 55 to 62 % of second-degree burns, and 30 to 40 % of third-degree burns develop keloids and hypertrophic scars after autodermoplasty.
They are the most problematic and sensitive of all possible scars, because in the course of their development they cause a person inconvenience: they spoil the aesthetic appearance, cause itching, redness and increased temperature at the site of the injury. Also, the hypertrophic scar enlarges over time and invades healthy areas of the skin.
Care after skin grafting

The speed of healing after the procedure depends on how well you follow your doctor's instructions. The regeneration process itself takes place in three phases:
- Adaptive changes in the transplanted skin. The foreign fragment adapts to the new conditions and begins to interact with the organism. This process takes 2-3 days.
- Regeneration (healing phase) .. The skin fully adapts to the new conditions; Donor cells are replaced by new cells, the synthesis of connective tissue proteins occurs. This process takes about 3 months.
- stabilization. Normal skin structure is restored, with the transplanted areas becoming identical to the 'original' skin. This phase will be completed within 6 to 18 months.
After the operation, the transplanted skin grows back within 7-10 days. The bandage should be changed every 2-3 days and the old bandage removed in layers: the lower layers will cling to the unhealed wound and there is a risk that the wound will open again with careless movements. After that, the bandage should be changed daily with the help of a nurse or doctor. To speed up healing and prevent infection, antiseptics and medicines prescribed by the doctor are applied to the wound. In addition to bandages, there are a number of recommendations that the operated patient must follow:
- Avoid thermal and mechanical effects on the injured area - do not wear skimpy, synthetic or restrictive clothing;
- Do not wet the operated area and cover it with polythene or any other waterproof material for reasons of personal hygiene;
- Do not remove the bandage yourself;
- Drink plenty of fluids, about 2-2.5 liters of water per day for an adult;
- avoid spicy, salty and smoked foods; enrich your diet with vitamins, macronutrients and protein;
- Refrain from alcohol and smoking.
How do I change a patient's colostomy bag?
If a person is unable to take care of themselves and needs help, the nurse, caregiver, or family members will change the colostomy bag. The colostomy bag should be changed before or a few hours after a meal when the bowels are not too active.
Before beginning the procedure, help the patient into a comfortable position and cover the abdomen with a diaper or paper towel to protect clothing. Wash your hands thoroughly and wear non-sterile gloves.
- wipe the moistened skin;
- cleaning spray or antibacterial wipes;
- silicone protective film spray or wipes;
- special ostomy sealing paste;
- colostomy bags;
- scissors with rounded tips;
- a template for determining the size of the opening to be cut for the stoma.
Gel bags for colostomy bags and medications can also be helpful.
- Use the template to determine the shape and size of the stoma.
- Draw the contours of the future opening on the protective layer of paper covering the adhesive plate of the colostomy bag. It should be about 2-3mm larger than the diameter of the stoma.
- Cut out the opening with rounded scissors and smooth the edges with your finger to remove any imperfections.
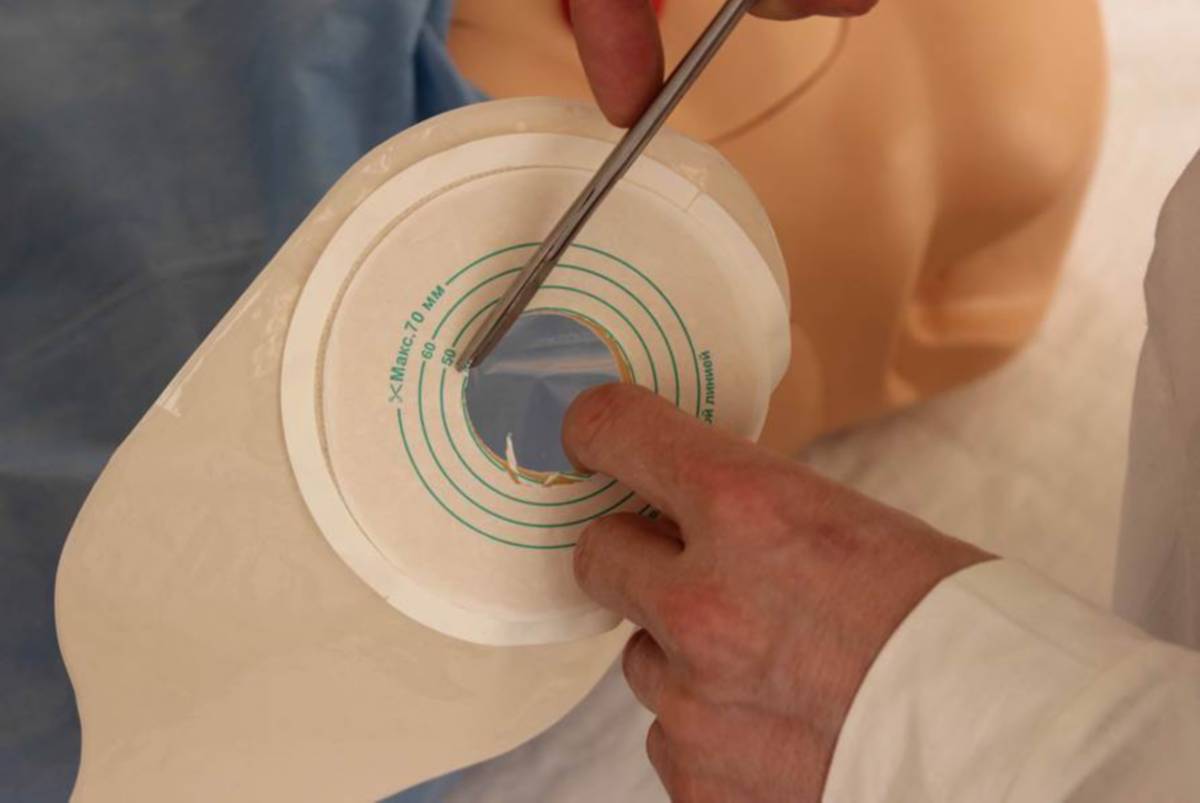
- Gently remove the old colostomy bag with Niltac spray to avoid skin trauma.
- Clean the skin around the stoma with wet wipes or with water and baby soap, then allow it to breathe and dry.
- Carefully inspect the stoma and the area around the stoma for irritation, diaper rash, sores, and inflammation.
- If the skin is healthy, apply a protective silicone pad, Silisse or ConvaCea.
- Apply a thick layer of Stomagezip paste around the stoma.
- Heat the adhesive pad of your new colostomy bag between your hands to help it stick.
- Remove the protective paper layer from the adhesive sheet and stick it to the skin, starting from the bottom.
- Use your hand to gently press the colostomy bag against your abdomen to help it stick.
- Make sure the deflation arm of the deflated colostomy bag is securely closed.
- The colostomy bag can also be secured with a special belt for added security.
Prevention and treatment of peristomal dermatitis
The inflammation and irritation of the skin around the stoma is called peristomal dermatitis. The main causes are soiling of the stoma skin and changing the colostomy bag too frequently and too gently without the use of non-stick and protective agents.
To avoid skin damage, you should use a good quality ostomy recommended by your doctor.
If the stoma is flat or indented, special convex stool plates are used.
If the patient is underweight or overweight, a safety belt is always recommended.
If the skin around the stoma is slack and has stretch marks and wrinkles, a sealing paste should not be neglected.
The stoma is initially swollen, but then the swelling goes down, which means that the opening in the colostomy bag's adhesive plate should be smaller.
If you notice redness, swelling, maceration of the skin, or other signs of inflammation when changing the colostomy bag, always use a healing powder (wound dressings) or oil-based cream paste. However, the oily cream paste should be thoroughly rinsed off the skin before inserting the colostomy bag, and the healing powder should be left on the skin.
At kama-med.ru you can always get free advice from experts on the choice of ostomy care products and wound treatment.
- A tricky stump.
- Cult at Shopar.
- The reamputation is.
- blunt.
- What to do with amputated limbs?.
- Life after a leg amputation.
- Indications for amputation.
- acetabulum.
