If the heel hurts when you wake up and hurts when you go to sleep in the morning, a number of diseases with damage to the joints and connective tissue can be the cause. These triggers include various pathologies:

- Treatment of heel spurs
- Causes of heel spurs
- Causes of heel pain
- Treatment of heel pain
- Treatment of heel pain
- physical therapy
- Treatment
- prevention
- evaluation of results
- Symptoms of a heel bone fracture
- Causes of heel spurs in children
- classification
- Causes of heel pain
- Common Complaints
- Pain in the heel can tell us a lot
- Structure of the heel
- What to do if the heel hurts and walking hurts?
- Heel pain after an injury: what to do?
- Why does the heel hurt when the tendon or ligament is pulled?
- Heel pain at bunions
- What diseases and health problems can cause heel pain?
- How do you treat heel pain?
Treatment of heel spurs
A heel spur is hypertrophy of the heel bone caused by calcium deposits. The protuberance can be spike- or wedge-shaped and can be between 2 and 13 mm in size.
Sometimes heel spurs are mistakenly referred to as plantar fasciitis. However, this is a different condition – inflammation of the plantar fascia (the connective tissue that supports the arch of the foot). A heel spur can form as a result of such inflammation, but this is not always the case.
Causes of heel spurs
The process of lime deposition takes months. The mechanism of disease development is limited to stretching of the fascia and microtrauma of the membrane covering the heel bone. Regular trauma provokes degenerative and aseptic inflammatory processes in the tissues. The latter cause limescale deposits.
The development of a heel spur can be triggered by:
- running or jumping;
- overweight;
- Uncomfortable footwear (hard, thin soles, high heels or without cushioning insoles).
Heel spurs are caused by:
- Longitudinal flatfoot (causes an uneven load on the foot);
- osteoarthritis (destruction of joint cartilage);
- Metabolic disorders including gout (leading to salt accumulation).
Finally, indirect causes of heel spurs should also be considered, such as: B. A lifestyle of constant standing, high arches, and limited foot flexion. After the age of 40, a person falls into the risk group, and in old age 25 % of the population is diagnosed with a spur.
Causes of heel pain
Our foot and ankle are made up of more than 100 tendons, 33 joints and 26 bones, the largest of which is the heel. Although nature designed us to be able to move for long periods of time, damaging or overloading it is a lot easier than it sounds.
In most cases, severe heel pain is not caused by a one-off injury, but rather by repeated strain and impact.
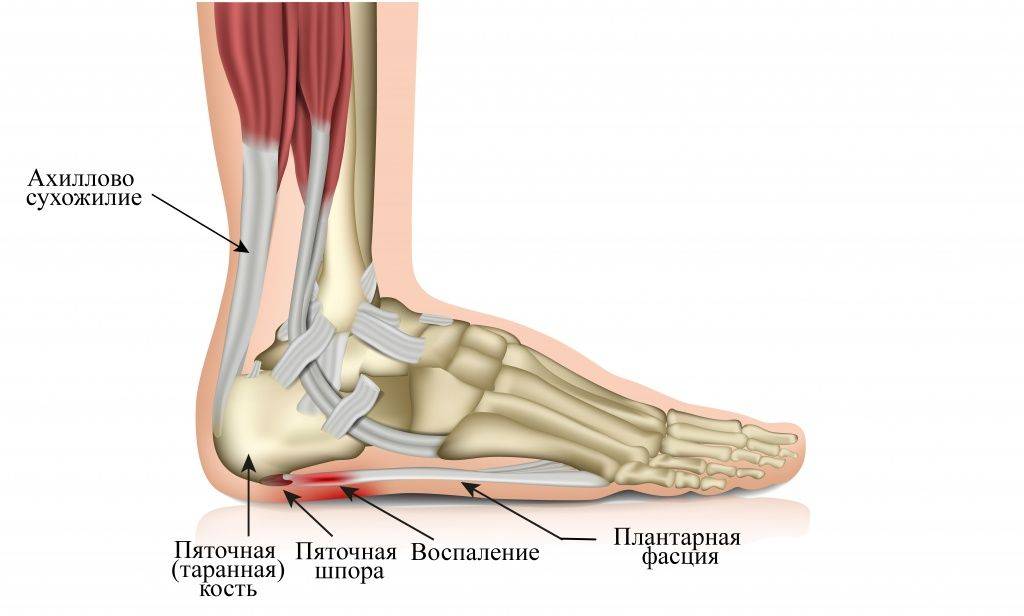
Inflammation of the plantar tendon or fascia – is the most common cause of heel pain in the morning and at rest. It occurs when a special tissue called the plantar fascia — a tendon-like band that runs from the heel to the toes — becomes inflamed.
It's caused by overstretching when the foot isn't built properly - flat feet or an arch that's too high - the part of the sole that doesn't touch the ground, wearing shoes that don't provide the necessary support when walking on a flat, hard surface Provide support, too much weight or overweight.
Sometimes doctors also notice a spur, which is a growth on the lower part of the bone that sticks out like a spike and compresses the underlying soft tissue.
The main symptom of plantar fasciitis is heel pain on foot strike, which worsens over several months, especially after periods of rest, and decreases with walking. This is because when you walk, this thick band of tissue is stretched, allowing the foot to move freely. However, the symptoms of the disease also appear after standing for a long time, since the damaged tissue is quickly overstretched and can no longer withstand normal loads.
In most cases, the problem can be treated within a few months. These include rest, ice packs, stretching exercises, physical therapy, nonsteroidal anti-inflammatory pain relievers, or hormones. These treatments are usually sufficient, with surgery only being necessary in rare cases.
Treatment of heel pain
Most cases of heel pain disappear within a few months, even with conservative treatment, that is, without surgery, but only with the competent support of a doctor and not on your own.
- Nonsteroidal anti-inflammatory drugs - NSAIDs such as ibuprofen or diclofenac - reduce swelling and discomfort.
- Corticosteroid hormone injections are used when inflammation persists and cannot be relieved even with NSAIDs. These funds should be used with caution and only under medical supervision, since their long-term use can lead to side effects - swelling, increased blood pressure and blood sugar levels, slowed tissue repair and many others, no less serious.
- Physiotherapy, ie special exercises, help to properly stretch the plantar fascia and Achilles tendon and strengthen the lower leg muscles so that the ankle and heel can absorb and process loads properly.
- Special Bands - Elastic bands used by athletes provide good support for the lower part of the foot.
- Orthopedic devices and insoles with orthotics help the foot stay in the correct position and relieve pressure on damaged tissues for faster recovery.
- Special night splints worn on the lower leg and foot ensure that the plantar fascia and Achilles tendon are stretched while you sleep. After such a rest, the first steps in the morning will be much easier, and an ordinary trip to the toilet will not become a torment.
Unfortunately, it is not always possible to do without surgery - it is necessary for people who, despite all efforts to seek treatment, still experience severe pain.
For example, with fasciitis it is sometimes necessary to release the ligament from the heel bone, which can weaken the arch, with bursitis it may be necessary to remove the inflamed joint capsule, and with a spur it may be necessary to remove a growth, pressing on the underlying tissue.
Treatment of heel pain
The treatment plan for dorsal foot pain depends on the type of process that caused the negative feeling. With drug treatment, patients are prescribed several types of treatments aimed at reducing pain and restoring functional activity:
| types of treatment | Description |
| Anti-inflammatory therapy | The drug treatment plan includes nonsteroidal and hormonal anti-inflammatory drugs (NSAIDs, NSAIDs, glucocorticosteroids), massage therapy and physical therapy. |
| normalization of blood flow | With vascular disorders, drugs are prescribed to restore microcirculation and capillary resistance (angioprotectors, anticoagulants, ganglion blockers). |
| restoration of nerve conductivity | Symptomatic treatment (antidepressants, anticonvulsants). |
B vitamins are used as adjuvant drugs, and immunomodulatory agents are used in the treatment of autoimmune diseases.
Pain that prevents walking can be treated surgically. Surgical intervention is performed for complex pathologies caused by traumatic or degenerative changes in the tissues of the heel. Surgical treatment is used for fractures, Achilles tendon tears, plantar fasciitis, and to remove articular cartilage.

physical therapy
The supportive treatment consists of physiotherapeutic treatments (electrophoresis, laser therapy, shock wave therapy) and physical therapy. Patients with degenerative-dystrophic changes in the heel joints need to engage in physical activity. To minimize the effects of the injury, it is advisable to delay or reduce the intensity of physical activity.
Treatment
There are currently several types of heel spur treatment:

- Medication. The goal is to reduce inflammation and eliminate pain when walking.
- MBST therapy. It is said to reduce swelling, relieve pain and improve vascular function.
- laser therapy. To stimulate tissue, reduce swelling, eliminate inflammation and relieve pain.
- phonophoresis. This method combines the benefits of hormonal, anti-inflammatory ointments and ultrasound. Under the influence of ultrasound, the active substance of the ointment penetrates the heel better and very effectively reduces inflammation.
- X-ray therapy. With this method, the nerve endings near the heel spur are blocked, reducing or eliminating pain when walking.
- shock wave therapy. It helps dissolve the growths. It is a non-surgical treatment that is often comparable to surgery in its effectiveness. However, a number of treatments are required to achieve results.
Since these methods are not always successful, there is another option: surgical treatment of heel spurs. Typically, 5 % patients require this option.
Lifestyle changes and additional medical advice are also an important part of treatment:
- Wearing special orthopedic insoles to reduce stress on the heel.
- Regular foot baths and massages (on doctor's advice).
- Therapeutic exercises for heel spurs (specific exercises). These are necessary to keep blood vessels and muscles in good condition. Common sports for people with this condition include cycling and swimming. Foot gymnastics without straining the heel is also useful.
- Diet to restore metabolism. In general, you should eat a healthy diet, avoid excess salt and drink plenty of clean water.
prevention
Preventive measures include:

- Timely treatment of all orthopedic diseases: diseases of the spine, flat feet, etc.
- Increased attention to the condition of the joints in order to prevent their diseases.
- Selection of suitable footwear – without high heels, with a stable but not too flat heel.
- Supplementing the footwear with special insoles, which are selected with the assistance of an orthopaedist.
- Moderate physical activity for a harmonious development of muscles, ligaments and joints.
- Avoiding foot overloads and various types of injuries (avoiding dangerous situations).
- Regular gymnastics for the feet.
- weight control. Excessive weight puts a lot of stress on the heel area, which can contribute to the development of spurs.
- Healthy and nutritious diet.
It pays to follow these recommendations from an early age to eliminate the risk of later disease or to delay the first signs of heel spurs.
evaluation of results

In private medical centers, the radiologist interprets the images immediately after the diagnosis is made. If a digital machine is used, the X-ray image is transferred to a computer, where it can be enlarged to allow a closer look at the structures.
In the conclusions, the doctor enters the size of the heel bone, detected lesions, fractures and any fractures. Signs of heel spurs and malignant growths will appear. The diagnosis is made by the attending physician on the basis of x-rays, complaints, visual changes, test data and other examinations.
Symptoms of a heel bone fracture

A calcaneus fracture occurs when a strong external force is applied that exceeds the maximum strength of the bone structure. In older people, injury is possible even with a small trigger, since osteoporosis increases with age. A broken heel is characterized by severe pain that increases when the foot is touched, swelling of the injured area, and bruising. The calcaneus may appear flattened following the injury and the ability to fully support the foot is severely limited, but mobility in the ankle is preserved.
If a heel bone fracture is suspected, X-rays are taken in three projections. If the diagnosis is confirmed, a plaster cast is applied from the fingertips to the knee joint.
Heel X-ray is a simple diagnostic method used in the treatment of children and adults. The examination in our center can be carried out with modern equipment and without waiting times.
Causes of heel spurs in children
In the normal state, the fascia is always taut and protects the bony and muscular structures of the foot from damage. Trauma, inflammation, or excessive deposition of calcium salts compromise the integrity of the fibers and a bony outgrowth, known as an exostosis, gradually forms in this area.
The main causes of bony outgrowths in children of different ages forming spurs are:
- flat feet, in which the load on the ligaments and muscles of the foot is abnormally and unevenly distributed;
- Obesity, which increases the pressure on the lower limbs;
- wearing shoes that are too tight, narrow, heavy and uncomfortable, not adapted to the size of the foot;
- a sedentary, sedentary lifestyle;
- Certain musculoskeletal disorders that shift axial loading of the skeleton, such as B. scoliosis;
- inherited predisposition;
- Excessive physical exertion in sports and other physical disciplines;
- Metabolic disorders and diseases related to the endocrine system;
- Injuries to the bones and joints of the lower limbs (dislocations, sprains, fractures, severe bruises);
- vascular diseases, in which the blood supply to the feet is impaired;
- Bone and cartilage diseases (osteoarthritis, arthritis, deformities of the limbs, etc.).
In some cases, the starting point for the development of the disease is an infectious inflammatory process in the surrounding tissues, as well as conditions in which there is a decrease in the density of bone structures.
Risk factors are children who are regularly subjected to static loads (running, long jumps, long walks), children who are subject to hormonal changes, and children who have problems with calcium and phosphorus absorption.
classification
According to the International Disease Registry ICD-10, plantar fasciitis refers to pathologies of the musculoskeletal system and connective tissue. The disease can be unilateral, with osteophytes forming on one foot, or bilateral, with osteophytes affecting the soles of both feet.
The course of development of plantar fasciitis can be divided into three stages:
- The first stage, entosopathy, is characterized by the first pathological changes in the longitudinal fascia under the influence of a traumatic factor;
- The second stage, fasciosis, is characterized by aseptic inflammation of the plantar fascia, that is, the process proceeds without the involvement of foreign pathogens;
- In the third stage, calcification, excessive accumulation of calcium salts occurs in the damaged fascia, leading to the formation of bony outgrowths.
The process of osteophyte formation is quite lengthy, lasting from 2 weeks to several months, depending on the type of injury and the cause of the pathology.
Causes of heel pain
The physiological causes of pain are not disease-related. For example, the heels hurt a lot when the layer of fat on the skin of the sole becomes thinner. The pain is caused by constant strain, e.g. B. by standing work or wearing high heels.
A common cause of heel pain is inflammation, which can be attributed to various factors. injuries. The most common cause of heel pain is inflammation resulting from trauma to the heel structure caused by mechanical damage to bones, tendons, joint capsules, or ligaments. It can also cause pain associated with heel spurs, broken bones, bruises, bursitis, ankle ligament or Achilles tendon dislocations and Sever's disease - a tear between the epicondyle and bursa, Haglund-Schinz disease - destruction of the shaft bone from excessive mechanical stress; Achilles tendonitis - Inflammation from excessive strain or wearing uncomfortable footwear.
The second cause of heel osteoarthritis in patients is metabolic disorders caused by diabetes and gout. In diabetes, the veins in the feet suffer first by developing diabetic angiopathy, which also attacks the walls of the blood vessels. In gout, uric acid salts are deposited in the joints and periarticular structures. Causes of pain syndrome: in diabetes – vascular disorders, in gout – uric acid accumulation.
In Bechterew's disease, a chronic inflammation of the joints and spine caused by an abnormal autoimmune response, rheumatoid arthritis causes deformities and limited joint mobility due to pain and swelling; Heel pain sometimes occurs with inflammatory conditions caused by autoimmune diseases - e.g. B. reactive arthritis caused by intestinal and urogenital infections such as salmonellosis, yersiniosis, chlamydia, gonorrhea and others; tuberculosis of the bone tissue with superinflammation of the bone substance and necrosis of the skin parts; purulent necrotizing process caused by inflammation of the heel bone, tendon and adjacent soft tissues. Pain is rarely caused by pathogenic inflammatory microorganisms in the structures of the heel. Tuberculosis and osteitis usually lead to suppurative osteitis on the heel.
Common Complaints
If the heel hurts on the inside, an x-ray should be taken first to rule out a heel spur. In the absence of a spur, lateral pain can be caused by sports, home and other injuries, foot deformities, obesity, uncomfortable footwear, and heavy physical labor. If your heel hurts when you walk, try to reduce the strain and see your doctor. Heel spurs, achillitis, heel bone osteochondropathy, bunions, or stress periostitis, as well as infectious diseases, tumors, and trauma may be associated with these symptoms. The doctor treating you makes an individual differential diagnosis. Heel pain after sleeping is most common with plantar fasciitis, which is characterized by severe pain and swelling in the morning that subsides in the afternoon.
When you visit the doctor, you will be examined according to a specific plan. Your doctor will first question you in detail about your symptoms, explain the type, extent and location of your pain as well as any additional pain symptoms and carry out an initial examination of the heel area. If you have persistent pain in the heel area, you should visit a podiatrist to rule out a dangerous condition that requires urgent treatment.
Conditions that can cause heel pain:
- Heel spurs or plantar fasciitis
- bunions
- Haglund's deformity
- Tarsal Tunnel Syndrome
- tuberculosis of the bone
- osteomyelitis
- reactive arthritis
- osteochondropathy
- Osteoarthritis of the metacarpal
- diabetic angiopathy
- gout
- bruises
- sprains
- tendonitis
- fractures
Pain in the heel can tell us a lot
Despite its small size, the heel is subjected to the most stress throughout our lives. Constant static loads, dynamic trauma and various diseases can cause inflammation in the heel. One day, walking on the heel becomes painful.
To understand the causes of heel pain when walking, we need to look at the structure of the heel and how it relates to and interacts with the other anatomical structures of the foot, ankle and lower leg.
Structure of the heel
The calcaneus bone, located at the back of the foot along with the surrounding fatty tissue and skin, is what we commonly call the heel. Together with the ankle bone (talus), the cuboid (cubic bone), the scaphoid (navicular) and the three sphenoid bones (sphenoid), it belongs to the tarsal bone.
- On the underside of the heel bone is an outgrowth called the calcaneal tubercle, which attaches the soleus ligament, which supports the arch of the foot. There is also one of the largest and strongest tendons in the human body, the Achilles tendon, which continues the work of the cambio and calf muscles. The Achilles tendon allows the plantar bone to flex.
- The heel bone connects at the top with the ankle bone (talus) to form the ankle joint and at the front with the elbow bone (cubitalis) to form the tarsal joint (tarsal joint), along with the talus and ankle joint.
- In the lower subcutaneous fat layer of the heel, numerous arteries, veins and nerves intertwine, which are connected to the tibial nerve.
- On the outside of the heel, under the subcutaneous fat layer, is the sagittal tendon capsule, under which the two short extensors and the adductor muscle of the little toe begin, as well as the ligaments of the ankle and talus.
- On the inside of the heel bone are the deltoid ligament of the ankle, the popliteal ligament and the tendon capsule of the extensor and adductor tendons of the thumb, under which the flexor tendons of the long fingers run.
What to do if the heel hurts and walking hurts?
Let's look at all of the above causes and associated treatment.
Heel pain after an injury: what to do?
A bruised heel is not that unusual. An unfortunate landing from a great height, running, jumping or walking barefoot for a long time on uneven ground is enough. This can lead to symptoms:
Anything can happen with a bruise:
Swelling, reddening of the bruise, and bulging are unfortunate symptoms that may indicate a tendon or ligament tear, heel dislocation, or heel fracture.
Therefore, the heel must be relieved immediately and taken to the emergency room as soon as possible, where the emergency doctor will take an x-ray of the heel and provide first aid: bandage the wound, apply a tight bandage or a cast.
Running, jumping, or turning the foot inward often overstrains the Achilles tendon and ligaments of the foot.
Why does the heel hurt when the tendon or ligament is pulled?
The Achilles tendon attaches directly to the heel bone, and the ligaments of the ankle attach to the heel or to the bones that articulate with it (talus, scaphoid), so a dislocation of both the AC and ligaments causes heel pain caused.
- If the AC is completely torn, the symptoms are as follows:
- sudden stabbing pains in the heel, ankle and lower leg;
- inability to stand on tiptoe, flex or straighten foot;
- Swelling and redness at the back of the heel and ankle.
- Pain on the outer, lateral surface of the heel and ankle (a sign of a lateral ankle ligament sprain);
- Inability to adduct and supine the foot.
Heel pain at bunions
Heel pain in bunions occurs in two main cases: Achilles bursitis or plantar bursitis.
What diseases and health problems can cause heel pain?
Deformities of the foot lead to an abnormal distribution of the load in the upright position. The first symptom is pain in the heel. As a result, other joints are damaged, which can lead to knee or hip arthrosis in the long term. Other deformations, e.g. B. the spine, lead to the same clinical symptoms.
The most common cause of heel pain is trauma. The heel is a complex structure that is damaged by mechanical stress. In addition to sprains and broken bones, there are the usual dislocations, torn ligaments and tendons and soft tissue injuries. How dangerous these are can be seen from the course of the disease. If swelling occurs and persists, bruises and dimples are visible, and the foot is in an unnatural position, an orthopedist needs to be urgently consulted.
There are no injuries like injuries: some are very dangerous.
Inflammatory processes on the heel are very dangerous. The affected person complains of acute pain and swelling, local and general temperature increases. If the ligaments are inflamed, the pain will not go away even after rest. Reactive and infectious arthritis, bursitis and fasciitis require urgent treatment. They can lead to complications such as abscesses, septicemia, and death. And it all starts with pain in the heel.
The ankle joint is affected by degenerative changes in the cartilage tissue, the amount of synovial fluid in the joint decreases and pain occurs. Osteophytes - bony outgrowths - form in the joint and the foot deforms and loses mobility. In the initial stages, you may notice discomfort at the end of the day or after a long walk. Over time, this discomfort worsens and develops into pain, you feel cramps in your feet and intuitively begin to limp.
If the disease is diagnosed early enough, it can be managed, which is not a bad thing given its incurability. Injecting synovial fluid from the prosthesis can effectively fix the joint deficiency and relieve the heel pain. If the preparation is based on hyaluronic acid, the injections must be repeated every six months. If we are talking about synthetic Noltrexin - much less often, once every 1.5-2 years.
How do you treat heel pain?
The success of treatment depends on how quickly and correctly the cause of the problem is identified. Do not overdo it with painkillers, ointments and poultices, because with some diseases, on the contrary, they can even harm. Observe the following rules:
- Have the diagnosis made by an orthopedist or rheumatologist;
- if your heel hurts badly before the consultation, apply a cold compress once;
- Rest your lower limbs;
- Walk with assistance - use a cane or handrail;
- Avoid self-medication.
Diagnosis may require MRI or CT scan, tests, and ultrasound of blood vessels. Depending on the underlying cause, your doctor will select medications and prescribe physical therapy. You may need to wear special orthotics or orthopedic shoes.
Heel pain can only be treated once the cause has been identified
Anyone who has ever suffered from heel pain knows how much it complicates life. Normal movements cause discomfort, a normal life can no longer be lived. If inflammation develops, the risk of an abscess increases. Sometimes surgery is required, but fortunately many problems can be treated conservatively. So be vigilant and don't turn a blind eye to the occasional sharp pain in your foot because your health is at stake!
- Structure of the heel.
- Treatment of plantar fasciitis.
- bones in the heel.
- The bones of the human heel.
- Treatment of plantar fasciitis at home.
- Tear of the foot fascia.
- How to cure plantar fasciitis forum.
- Structure of the human ankle.
