There is a specific first aid algorithm for upper limb soft tissue injuries. In the case of a dislocated shoulder joint, the first thing you should do is stop the physical strain on the injured shoulder immediately. Well, this advice can be considered unnecessary as in most cases further movement is not possible. However, you should not try to 'work' the shoulder by pushing it up or pulling it to one side. This can worsen damage to ligaments, tendons, or muscles.

- Stretching of the joint capsule
- Stage 1: Freezing
- ICD-10
- causes
- What types of joint dislocations are there?
- Our specialists
- Stages of shoulder capsule inflammation
- Symptoms of adhesive capsulitis
- How is a hip dislocation treated?
- Anterior cruciate ligament rupture in knee
- shoulder instability
- Before treatment, the causes must be eliminated
- How to treat the cruciate and collateral ligaments of the knee joint
- Causes of dislocations of the shoulder joint capsule, muscles, tendons and ligaments
- Signs of a shoulder sprain
- Treatment of strained and torn ligaments in the shoulder
- Mechanism and symptoms of shoulder joint sprains
Stretching of the joint capsule
Frozen shoulder, or adhesive capsulitis, is a condition that causes pain and limitation of movement in the shoulder joint and can lead to significant impairment of shoulder mobility over time.
Once the period of peak symptoms is over, mobility of the shoulder joint in adhesive capsular inflammation begins to return to normal, but full recovery can take up to three years. The main treatment for adhesive capsulitis is physical therapy to restore and maintain mobility of the shoulder joint. Surgery is often required as well.
Adhesive capsulitis occurs most often between the ages of 40 and 60, slightly more often in women. The risk of developing this disease is increased in people with diabetes.
The human shoulder joint is a ball and socket joint made up of three bones: the humerus, the scapula, and the collarbone.
The head of the humerus articulates with the corresponding socket of the scapula. The circumference of the joint is surrounded by a tough connective tissue covering, the joint capsule.
The inside of the joint capsule is lined with a synovial membrane. This membrane produces synovial fluid, which acts as a lubricant and allows free movement of the shoulder joint.
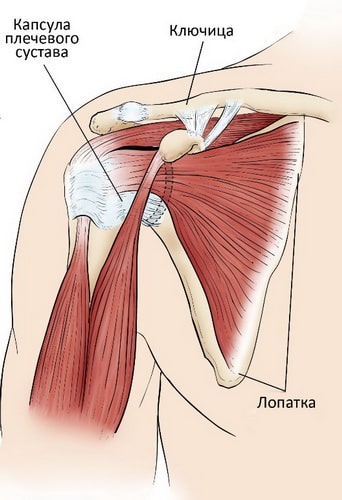
The shoulder joint capsule surrounds the shoulder joint and the rotator cuff tendons.
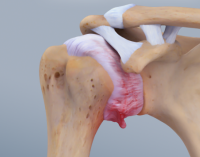
In frozen shoulder syndrome, the shoulder joint capsule thickens and becomes narrow and stiff. Bundles of connective tissue fibers called adhesions form in the joint cavity. In many cases, there is also a reduction in synovial fluid in the joint.
The main features of the disease are a pronounced pain syndrome and a significant impairment of the mobility of the shoulder joint - the patient can move the arm in the shoulder joint either independently or with the help of others. The disease proceeds in three stages.
Stage 1: Freezing
In the freezing stage, patients notice a slow progression of pain in the shoulder joint. As the pain increases, so does the loss of mobility in the shoulder joint. This stage usually lasts between six weeks and nine months.
At this stage, pain may decrease slightly, but mobility limitations remain. The duration of this stage is 4-6 months, during which the patient complains of severe limitation in activities of daily living.
ICD-10
Adhesive capsulitis is a disease that causes severe limb dysfunction and long-term disability, but has a good prognosis and ends in cure. It is diagnosed in about 2 % of the population. It usually occurs between the ages of 50 and 70, with women being affected 3-5 times more often than men. The dominant and non-dominant hands are equally affected. In 7-10 % patients, the adhesion process is bilateral, with symptoms in the other shoulder appearing within a few months to years of onset.
causes
The causes of adhesive capsulitis have not yet been elucidated. Researchers hypothesize that the disease is caused by trophic abnormalities resulting from a neurological defect. Experts believe that the disease is etiologically related to pathologies of reflex tissue dystrophy, such as Sudeck's syndrome, which often occurs simultaneously with capsulitis (shoulder-knee syndrome).
Adhesive capsulitis can develop on its own or be triggered by other disorders. The disorders that most commonly cause capsular contracture include:
Type II diabetes is the most common cause of a secondary adhesion process; one in three diabetics will be diagnosed with this condition. The connection between capsular inflammation and tendinitis (the most common cause of shoulder pain) is not supported by research data.
What types of joint dislocations are there?
There is a classification of dislocations commonly used by traumatologists today. According to the type, joint dislocations can be:
- Complete - absolute disruption of the congruence of the articular surfaces
- Incomplete - with partially preserved congruence through the ligament and joint apparatus
- Congenital – hip dislocation is common
- Acquired pathological – when joint changes occur
- Acquired traumatic - caused by forces exceeding the protective capacity of the ligaments and joints.

Fill out the form and we will get in touch with you.
Our specialists
Vertebrologist, Orthopedist, Traumatologist, MD/PhD
The frequency of dislocations depends on the anatomy and physiology of the joint. The shape and size of the joints, the elasticity of the ligaments and joint capsule, muscle tension, etc. play an important role. The most common dislocations occur in the shoulder joint, in the forearm joints and, to a lesser extent, in the hip joints and in the phalanges of the hands.

The pathogenesis of the acquired dislocation is trauma to the periarticular ligamentous apparatus, which results in relative movement of the articular surfaces and incongruence. Without appropriate treatment, serious complications such as inflammation, fractures of the bony structures of the joint, arthrosis, venous thrombosis, pulmonary embolism, joint stiffness and even complete immobility - ankylosis - can occur.
A dislocation is dangerous because patients may not seek hospital treatment and try to self-medicate, including pulling the joint, which is absolutely forbidden for non-specialist traumatologists. However, it is imperative that the injured person is supported and given first aid.
Stages of shoulder capsule inflammation
There is a clinical classification of adhesive capsular inflammation of the shoulder joint according to its stage. Three stages are distinguished. As the disease progresses, the clinical picture changes in several stages.
- Frostbite stage (painful). Its duration varies between 3 months and a year. It is accompanied by a severe inflammatory process that causes pain and further restriction of movement of the affected shoulder.
- stiffness (rigidity). As pain sensations decrease or disappear altogether, stiffness increases. Inability to perform normal movements. The duration of this stage ranges from 4 months to a year.
- Dissolution (thawing, thawing). Over the next 12-42 months, mobility is restored and the pain syndrome completely disappears. 50 % of the patients make a full recovery. The rest have more or less limited mobility, but this does not prevent them from living a full life.
The duration of the individual phases as well as the disease as a whole is not precisely defined. This parameter is influenced by the individual characteristics of the organism, accompanying pathologies and the timeliness of diagnostic and therapeutic measures. It has been found that the longer the first phase lasts, the longer the next two phases last. Without therapy, healing takes 1.5 to 4 years.
Symptoms of adhesive capsulitis
One of the main symptoms of capsular inflammation is unexplained pain in the affected joint, which sometimes occurs after physical exertion or minor trauma. These get worse in the first 2-3 weeks. The excruciating pain is troublesome in the evening and at night; it is impossible to lie on the affected shoulder and turn from side to side without waking up.
The second main symptom of capsular inflammation is the restriction of movement in the affected shoulder. It is difficult to swing the shoulder outward, move it sideways, and finally it becomes difficult to rotate the shoulder. Basic daily activities such as eating, washing, dressing and undressing, and combing become impossible.
In some cases, this condition can lead to the following symptoms
- An increase in body temperature to subfebrile levels;
- general malaise, body aches;
- reddening of the skin and excessive swelling of the tissue over the affected joint;
- strong pain.
In addition to the debilitating pain, the ability to work is also impaired. Therefore, consulting a rheumatologist is essential. Since the disease has no characteristic symptoms, it is difficult to diagnose it in a timely manner.
How is a hip dislocation treated?
The treatment of a dislocated hip begins immediately with first aid measures. These include immobilization of the limb (immobilization is necessary until bone and soft tissue fracture can be ruled out), applying a tight bandage, and applying cold. After 5-6 hours, hip sprain treatment may include administration of nonsteroidal anti-inflammatory drugs to relieve pain. After 24 hours, heat, UHF and other physiotherapeutic measures can be applied to accelerate tissue regeneration and bruise resorption.
However, the treatment of a hip dislocation does not end there. There is a potential risk of severe keloids and fibrous scarring at the site of the microscopic fibrous break.
These impair the normal function of the joint. The scarring of the muscle tissue leads to the disintegration of the hip joint.
The aim is to prevent the formation of scar tissue, improve the elasticity of ligaments and muscles, and increase muscle tone in the lower limbs.
In our chiropractic clinic, the following techniques are used for rehabilitation after hip dislocation:
- Massage to improve muscle conditioning, relieving excessive muscle tension;
- Osteopathy to improve blood and lymph microcirculation, thereby accelerating repair processes;
- Reflexology, which, with the help of acupuncture and pharmacopuncture, stimulates the regeneration process by tapping into the body's hidden reserves;
- kinesitherapy, remedial gymnastics;
- laser therapy;
- Physical therapy.
Anterior cruciate ligament rupture in knee
- Severe knee pain associated with an indistinct cracking sound;
- sensation of lateral or anterior displacement of the tibia;
- Unsteadiness ('looseness') of the knee joint or limitation of movement;
- inability to shift weight to injured leg while walking;
- swelling of the knee.
The tear can be complete or incomplete (when not all fibers are torn).
Diagnosis at Yusupov Hospital includes:
- Examination by a trauma surgeon. A set of tests to determine the crack:
- 'Anterior Drawer' Test - With the leg flexed at right angles, the physician draws the tibia toward him and compares the displacement of the joint to a healthy knee;
- Lachman test – gradually flexing the knee to an angle of 20-30° and assessing the degree of forward displacement of the tibia.
Rehabilitation after a conventional transplant takes about 6 months. With an artificial knee replacement, a return to sports training is possible after 2 to 3 months. Physiotherapy is actively used during rehabilitation.
In most cases, the range of motion of the knee joint is fully restored and the stability of the joint is restored. You can now return to your previous physical activity.
shoulder instability
Shoulder instability is the inability to keep the condyle in the correct position, which can lead to various dislocations. When a person performs certain movements of the shoulder with great force or very abruptly, a shoulder dislocation can occur. In addition, the bandage can be pulled or torn, resulting in a loss of strength and support of the joint itself, which can eventually lead to instability. If dislocations occur more than once or twice, this is an indication of chronic instability of the shoulder joint.
- poor posture;
- Heavy load on the shoulder;
- presence of dislocations and subluxations;
- Insufficient rehabilitation after a shoulder dislocation;
- hypermobility of the shoulder joint;
- Inappropriate or insufficient warm-up before exercise;
- weakening of muscle ligaments and muscular imbalances;
- Abnormal movement patterns in sports activities.
Patients with shoulder instability may have few or no symptoms.
The main symptoms of shoulder instability are:
- Symptoms of pain in dislocations and subluxations of the shoulder joint In the case of a dislocation, the pain is severe and acute, caused by an injury to the soft tissues surrounding the joint. With repeated dislocations, the pain lessens or disappears altogether;
- Limitation of movement of the upper limb due to dislocation of the joint head, every movement is stiff and accompanied by severe pain;
- Shoulder Joint Deformity With an anterior dislocation, the front of the shoulder joint is visually more rounded. With a posterior dislocation, the scapula is clearly bulging at the front of the shoulder joint, which is also visually recognizable;
- The occurrence of shooting pains, pops, crunches, or other painful sensations in subluxations. A subluxation occurs when objects are thrown sharply at the head from behind. The trauma patient may have uncomfortable pain sensations even at rest;
- Numbness and numbness in the hand due to nerve damage. A feeling of fear of a possible dislocation.
Before treatment, the causes must be eliminated
Before treating a dislocated knee ligament, all causes of the problem must be eliminated. In otherwise healthy people, the ligaments can usually cope quite well with the physical and impact loads they are subjected to.
Before treatment, our doctors usually determine several possible risk factors. This includes:
- instability of the knee joint;
- degenerative-dystrophic changes in the meniscus horns and their reduction in height;
- stretching of the joint capsule;
- scarring of ligaments and tendons;
- Rheumatic tissue damage in the knee joint;
- foot deformity (clubfoot or flatfoot);
- musculoskeletal dystrophy caused by various vascular anomalies or after long periods of immobility (e.g. as a result of casts after an ankle or hip fracture);
- development of contractures or ankylosis of the knee, ankle or hip joint;
- Short lower limb syndrome (often caused by pelvic twisting, deformity, postural changes, or after the development of deforming osteoarthritis of the large joints);
- Disorders of innervation of the lower limbs caused by osteochondrosis of the lumbosacral spine, piriformis muscle syndrome or cauda equina syndrome, entrapment of the sciatic nerve at the popliteal foramen.
Diagnostic arthroscopy should be performed prior to treating a torn ligament in the knee. In most cases, during this endoscopic procedure, the surgeon restores the integrity of the damaged fiber through plastic surgery. After the early postoperative period, treatment can then be initiated for full rehabilitation using chiropractic techniques.
Choosing the right technique for treating a torn knee ligament is important. In most cases it is possible to repair ligaments without surgery using manual therapy techniques. However, it is also important to eliminate as many potential risk factors from your life as possible, such as: e.g.:
How to treat the cruciate and collateral ligaments of the knee joint
The question of how to treat the cruciate ligaments of the knee joint often arises, since they are subjected to high loads and often suffer mechanical damage. In the early stages of a dislocation, there is a small amount of capillary bleeding from the soft tissues surrounding the ligament. Capillary blood is rich in fibrin, so the dislocation heals quickly. However, the resulting connective tissue is not very stable. Therefore, if the cause of the injury is not eliminated, re-trauma will quickly occur. There is a larger area of injury and the area where the ligament fibers tear increases. This situation continues until the cruciate ligament is completely torn.
Also, the anterior and posterior cruciate ligaments must be diagnosed before treating the collateral ligaments of the knee. This is because the cruciate ligaments are the most commonly injured lateral structures and the cruciate ligaments are the most prone to instability.
An MRI scan is performed for diagnosis. In controversial cases, arthroscopy is performed under anesthesia when fresh blood is obtained during a puncture of the knee joint.
How to treat without surgery?
- First restore compromised ligament fiber integrity (this requires short-term physical rest);
- Then the natural regeneration process is gradually initiated;
- Capillary blood flow to the soft tissues around the knee joint is increased;
- The metabolic processes at the cellular level are improved;
- The function of all muscles of the lower limbs is improved.
Extensive treatment and rehabilitation is required to achieve these effects. This is developed individually for each patient by the attending physician. The general state of health, age, weight, lifestyle, occupation, concomitant illnesses and complications in the course of the illness are taken into account.
Causes of dislocations of the shoulder joint capsule, muscles, tendons and ligaments
There are underlying pathological factors that can cause shoulder dislocations, e.g. B.
- Insufficient development of muscle tissue;
- Excessive physical exertion (e.g. lifting excessive weight);
- shoulder injuries (blows, dislocations, fractures and fractures of the humerus and shoulder blade);
- shoulder sprains;
- Excessive range of motion.
A lack of animal or vegetable protein in the diet can be a predisposing factor. Without amino acids, the body cannot rebuild the structure of muscle tissue. Persistent protein deficiency leads to severe muscular dystrophy and frequent muscle loads, even with moderate loads.
The greatest long-term prognostic risk is dislocation of the shoulder joint capsule due to partial collapse of the labrum. Without proper rehabilitation, this injury will always result in a lack of locking of the humeral head in the joint cavity. This leads to a habitual dislocation of the shoulder.
A shoulder tendon strain is characterized by an injury to the sternoclavicular ligament. It can have the following causes:
- overweight;
- Deformity of the thoracic and cervical spine with hyperkyphosis or scoliosis;
- Abnormal blood supply to the shoulder joint due to malformation of the bone head;
- tunnel syndrome;
- cervical osteochondrosis;
- Static muscle tension in the collarbone area.
These conditions increase the risk of straining the sternoclavicular ligament tendon. So, if you have cervical or thoracic pain and your shoulder girdle muscles aren't trained enough, you shouldn't lift weights or engage in rapid, high-amplitude arm movements. You are sure to sustain an injury that will have dire consequences.
Signs of a shoulder sprain
The clinical signs of a shoulder sprain are difficult to miss. Typically, at the time of the injury, a stabbing pain will shoot through the joint and literally drop the shoulder. After that, every movement in the shoulder joint becomes difficult and causes new flare-ups of pain.
After a few minutes, the typical symptoms of a shoulder sprain become clearer:
- The pain increases in intensity;
- Movement becomes impossible;
- swelling around the joint;
- subcutaneous hematoma (initially bright red, then darkening, blue, purple, and green as the hemoglobin breaks down).
Palpation of the shoulder joint is painful. The head of the humerus is located inside the joint capsule. The joint itself is not deformed.
The pain may get worse over the next two to three days. After this time, all symptoms subside. Recovery occurs.
An x-ray should always be taken to make the diagnosis. This shows that there are no broken bones and that the head has detached from the joint capsule. When a dislocation, fracture, or fracture is ruled out, a soft-tissue sprain is treated.
If the swelling continues to increase after 2-3 days and the condition worsens, a tendon, ligament or muscle rupture with blood pooling in the joint capsule can be ruled out. An intra-articular puncture can be performed to rule out such a disease. If blood is found in the synovial fluid, arthroscopy is indicated. This is an endoscopic examination of the joint using special equipment. Surgery may be performed during the procedure to repair a soft tissue tear.
Treatment of strained and torn ligaments in the shoulder

In the Stolitsa network clinics you can undergo a high-tech procedure using your own platelet-rich plasma (PRP therapy) to speed up the healing of injuries to ligaments, tendons, cartilage, synovium and arthrosis.
The shoulder shell, which provides shoulder stability and upper limb mobility, consists of three joints interconnected by ligaments:
- A movable shoulder joint with a distinct capsule into which the ligaments that hold the humerus are woven.
- A firm connection between the clavicle and the shoulder process of the shoulder blade, which encloses the shoulder joint from above and is involved in the formation of the shoulder joint.
- A movable connection between the scapula and ribs held in place by tendon muscles.
There is also a stiff joint or joint (syndesmosis) between the breastbone and collarbone that allows for small, flexible rocking motions. Sprains of the shoulder ligaments, which include all injuries of the shoulder joint, lead primarily to a functional limitation of the upper extremity.
Mechanism and symptoms of shoulder joint sprains
Shoulder sprains are almost always the result of indirect trauma. It can be caused by falling on your shoulder while leaning back or doing horizontal bar exercises. A 'pulling' mechanism is characteristic of children, with adults lifting the child by the shoulder and pulling it off the floor. If the force of the injury is too great, the shoulder joint ligaments and joint capsule are completely torn and the humerus dislocated. If the ligaments of the shoulder joint are partially torn (luxation), the capsule remains intact and dislocation does not occur.
A shoulder sprain presents with acute pain, swelling, and limitation of active movement (due to pain). Passive movement is still possible and the shoulder and joint are not deformed, distinguishing a ligament strain from a shoulder dislocation.
Damage to the collarbone and clavicular joint results from direct trauma (impact) to the scapula, often associated with fracture of the collarbone. Clinically, there is local sensitivity to pain and swelling in the joint area. The mobility of the shoulder joint is moderately restricted.X-rays are always part of the diagnosis of shoulder injuries to rule out fractures and dislocations. However, it is not sufficient to determine the extent of the shoulder ligament tear, since the soft tissue structures cannot be made visible with the conventional X-ray image.
In order to rule out diagnostic errors and clarify the extent of the injury, computed tomography (CT) and magnetic resonance imaging (MRI) are available around the clock in the Stolitsa hospital network.
The treatment of an acromioclavicular joint rupture is conservative. Traumatologists apply a Dezos bandage to immobilize the shoulder rim for 7-14 days, depending on the extent of the injury. Physiotherapeutic measures are started within 2 to 3 days to speed up recovery. For magnet therapy, UHF treatment and some other treatments, there is no need to remove the bandage and the immobilization of the joint is not affected. Full recovery can be observed no later than three weeks after the injury.
- Pronation of the shoulders - what is it?.
- How much does shoulder dislocation surgery cost?.
- shoulder supinators.
- Diagram of a joint with and without a dislocation.
- Pronation and supination of the shoulder.
- How much does shoulder surgery cost?.
- There is abduction and reduction of the joints.
- This is what a dislocated leg looks like.
