Squint surgery is indicated in adults for a number of reasons:

- Squinting in adults: causes and treatment
- Can adult strabismus be corrected?
- types of
- symptoms
- Acquired clubfoot
- Treatment
- Ponseti method
- alternative therapies
- Types of osteoporosis of the joints
- osteoporosis of the hip joint
- How is osteoporosis of the joints diagnosed?
- Hardware treatment of strabismus in adults
- Surgical correction of strabismus in adults
- Causes of Squinting
- How is the surgical correction performed?
- Causes of post-traumatic contractures of the shoulder, elbow, knee, etc.
- Treatment of post-traumatic contractures
- What to do if the contracture has already occurred?
- Prognosis and possible complications
- prevention
Squinting in adults: causes and treatment
Normally, both eyes are aligned in one visual axis. The brain's processing of these two projections results in a single three-dimensional image of the object in focus. When squinting, binocular vision is impaired due to a dysfunction of the eye muscles.
Squinting (strabismus or heterotopia) is a disorder of the visual system in which the function of the eye muscles is disturbed. This causes the eyeballs to move out of sync when focusing the gaze. Visually, it looks like the eyes are looking in different directions. In strabismus, the eyeballs can move independently of each other. Each eye can be tilted down or to the right, up or to the left. Squinting can affect both eyes or just one. Often the condition is associated with other eye diseases that are the cause of the problem. In most cases, strabismus is diagnosed in childhood. Rarely does strabismus begin in adulthood (unless there is trauma that preceded the pathology).

In ophthalmology there is a standard classification of strabismus. It can be congenital or acquired and comorbid or non-comorbid.
Cases of congenital heterotopia are rare in medical practice. If the pathology develops already in the fetus in the womb, it may mean that in the last trimester of pregnancy the mother contracted a serious infectious disease or took powerful drugs that adversely affected the development of the child's visual system. Squinting can occur in both adults and children. It is caused by diseases related to refractive errors or by trauma.
The convergent type refers to an equal angle of deviation of the patient's eyes with respect to the axis of focus. In this case, the eyeballs retain their motor function.
Can adult strabismus be corrected?
Acquired strabismus is easy to diagnose and treat, unlike cases where the pathology is congenital or involves hidden strabismus in adults, which has its own characteristics (it can be recognized only through a detailed examination, since it is visually normal ).
If an ophthalmologist detects heterotopia in an adult, he will immediately prescribe a treatment for the patient. Otherwise, the disease will progress to a more serious stage, causing aesthetic and visual discomfort.
The treatment of strabismus has two main goals: to restore the function of binocular vision (its correct formation) and to correct refraction.
To achieve these goals, the ophthalmologist must correctly determine the methods of future therapy, which may vary depending on the individual characteristics and the course of the disease.
Modern medicine offers several ways to eliminate squinting:
- Apparatus treatment that achieves full or partial restoration of binocular vision;
- wearing glasses;
- occlusion – regular covering of the healthy eye for the duration of the treatment (this is done in order not to lose the effect obtained during the treatment);
- a surgical method used when cosmetic correction is required (it alone does not help restore binocular vision, ie it does not help to merge the two image projections into a single image).

The question of whether squinting can be corrected is answered positively in most cases. Several of the treatments mentioned above are often necessary for the success of the therapy.
types of
Squinting is a congenital pathology of the spine. It occurs in 7 % of women and twice as often (15 %) in men. It is practically asymptomatic and is detected by radiological examination.
Depending on the type of stiffening, the sacralization is classified as follows:
Deep fusion is characterized by the penetration of the vertebrae into the sacrum without fusing them. It is not distinguished as an independent type.
Depending on the type of anastomosed tissue, a distinction is made between bony, cartilaginous and articular fusion.
With regard to symmetry, a distinction is made between unilateral and bilateral.
With regard to the etiology, a distinction is made between true and false fusion (high concentration of salt deposits).
With regard to the clinical symptoms, there is a classification:
- Asymptomatic if fusion is discovered accidentally;
- early onset pain that radiates to the buttocks and legs, is not severe, and occurs after bruising, falling, or bending down suddenly;
- a later onset caused by age-related changes that occurs only in the lower back.
symptoms
The disease is asymptomatic, but in rare cases it can manifest itself with the following symptoms
- pain in the lower back, lower back, legs;
- Decreased or complete loss of sensation in the lower limbs with partial dysfunction;
- reduced motor function of the spine.
Those at risk include those over the age of 25 and those who exercise and lift weights after spinal injuries.
If the above symptoms appear, an appointment with an orthopedist should be made. A consultation with a trauma surgeon or spinal surgeon is also advisable.

Acquired clubfoot
Acquired clubfoot can be caused by trauma to the distal tibial epiphysis. In adults, it develops after fractures of the talus and ankle with inaccurate fracture reduction and in tuberculosis of the foot.
Paralytic clubfoot After a muscle or nerve injury, it is easy to identify the type of damage. The etiology of paralytic clubfoot in early childhood is not always easy to determine. The unilateral nature of the lesion and other signs of paralysis may rule out a congenital origin of the deformity.
forecast. Without early treatment, the deformity progresses, becomes permanent and often affects not only physical development, but also the patient's psyche. With early orthopedic treatment for clubfoot, quite satisfactory results can be achieved in terms of foot form and function. Restoration of normal function is achieved only after many years of functional therapy with great difficulty.
Treatment
Congenital clubfoot can be treated conservatively or surgically. In infants, treatment should be started as early as possible, that is, at the age of 7-10 days. In the mildest cases, treatment can include immobilization with a flannel bandage, corrective gymnastics, and massage. The treatment can be carried out by the mother herself under the guidance of a doctor. At a young age, all the bones of the foot are made of cartilage, have only ossification nuclei and are flexible to changes in the growth process, so the foot can be easily corrected without anesthesia with certain manipulations. These manipulations are performed according to the basic foot positions in clubfoot: supination, adduction, and plantar flexion (Fig. 2).

The Fink-Ettingen bandage technique for clubfoot is as follows: The child's limb is bent at a right angle at the knee to relax the muscles. The bandage is 2 m long and 5-6 cm wide. The free end of the bandage is placed on the dorsal surface of the outer edge of the foot and wrapped twice in a circular and tight manner around the forefoot, from the outer edge of the foot along the dorsum of the foot, through the inner edge along the sole, to the outer edge again (opposite the varus of the foot ). After the second round of bandages, the bandage is passed inside out over the outside of the lower leg to the thigh at the back of the knee, then diagonally across the front outside of the lower leg from top to bottom and in, to the inside edge of the foot, wrapped twice in a circle and then from the outer edge of the foot to the thigh (Fig. 3).

Since the bandage is applied under tension, the condition of the toes should be monitored, which should have a normal color after applying the bandage. If toe cyanosis persists for more than 10 minutes after applying the bandage, the bandage should be loosened.
Ponseti method
The Ponseti method is often the most effective method for clubfoot. This is a special bandaging technique that stretches the child's ligaments as much as possible without causing pain.
The Ponseti method lasts no more than 5-6 months (usually 2-3), and then the child has to wear braces - special shoes that are connected by a strong rod. The specialist will explain to the mother what they are for, how to use them and how long the child should wear them. It is important to remember that not wearing insoles almost always leads to a recurrence of the foot deformity.
Many experts consider the Ponseti method to be an excellent alternative to surgical treatment. Their main advantage is that the tissue is not traumatized, as is the case with surgery. Surgical procedures often lead to stiffening of the joint, breakdown of the muscles that were manipulated during surgery, and persistent pain. These consequences do not occur with the Ponseti method.
alternative therapies
Some parents find that clubfoot can be treated without a cast or surgery. They rely on other treatment methods. Because of this, their children go to the doctor too late when the process is already far advanced.
Parents should be aware that neither clubfoot massage nor exercise alone can eliminate foot deformity. It is often so severe that complex surgery is required to correct the shape of the foot. Nevertheless, such techniques are used as rehabilitation measures. They are necessary so that the muscles do not atrophy during plaster correction and to consolidate the effect in the recovery period.
During the plastering phase, massages are performed on the back, abdomen, upper limbs and non-plastered parts of the legs. This massage improves general body tension. During therapeutic exercises, the mother bends and straightens the child's legs at the knees and hips.
Types of osteoporosis of the joints
It is customary to divide the disease into 4 groups:
- Postmenopausal (occurs in women going through menopause);
- senile (characteristic of older people);
- secondary (caused by other diseases);
- Combined (a combination of two or even all of the above species).
Osteoporosis also differs in which joints are affected. Let's look at them individually.
osteoporosis of the hip joint

This is the most severe and most common form - 40 % of osteoporosis cases affect the hip joint. It can damage the hip joint even with light exertion, and the pathological tissue can spread to the spinal disc processes, skull bones and ribs. Osteoporosis of the hip joint, like other forms of this disease, is more common in women than in men.
The characteristic symptoms of hip joint damage are:
- Spasms throughout the skeletal muscles, mostly at night, but can also occur during the day;
- changed posture;
- pain in the lower back, front and sides of the hip that increases with exertion;
- Pain in buttocks and groin (recurring), sudden, intermittent;
- limping and changing gait to relieve discomfort, often unconsciously;
- Absence of anything that could be the cause of the pain, ie practically no cause;
- insomnia, deterioration in the general condition of the person;
- weakness in the legs (usually occurs a year after the onset of the disease);
- Deformation of the chest (if the process is extensive and advanced).
Osteoporosis of the hip is most at risk of rupturing the epiphysis of the femur, the neck of the femur, and damaging the socket of the hip (joint capsule).
How is osteoporosis of the joints diagnosed?
If you experience symptoms of osteoporosis of the joints, you should consult a general practitioner, trauma surgeon or rheumatologist. The doctor will conduct an initial examination and refer you for examinations. The fastest, most convenient and most informative method is ultrasonic densitometry. In just a few minutes, a statement can be made about the bone density in the entire body.
- Radiographs of diseased joints in two projections showing bone leakage, spikes on the articular surfaces, and periarticular fractures;
- ultrasound examination of the joints;
- CT SCAN;
- MRI;
- Blood tests for calcium, thyroid hormones, and estrogen.
If secondary osteoporosis is suspected, a differential diagnosis is performed to rule out other diseases that could be the cause.
Hardware treatment of strabismus in adults
To date, various technical systems for the non-surgical correction of strabismus have been developed and introduced into ophthalmological practice worldwide. Despite widespread skepticism, their effectiveness is very high. Device training usually lasts 10 to 20 days and includes four to five devices; a session lasts between 40 and 70 minutes on average.
Sinoptophore devices, in particular, are used both for diagnostic purposes and to restore binocular vision - the principle of this class of devices is the separate, independent display of images for the right and left eye (e.g. when the squinting eye is holding a plate and the healthy eye sees a chop, the patient must exert will effort and visual imagination to visualize the image of the chop on the plate). Using such methods, which require a lot of motivation and perseverance, in most cases strabismus can be eliminated without surgical intervention.
Surgical correction of strabismus in adults
Some patients unjustifiably insist on radical squint correction 'in one session', even with a scalpel. This type of maximalism is mostly due to a lack of awareness. Above all, patients should be aware and take into account that restoring the correct position and synchronous movement of the eyeballs has a purely external, cosmetic effect and does not automatically mean the restoration of visual function.
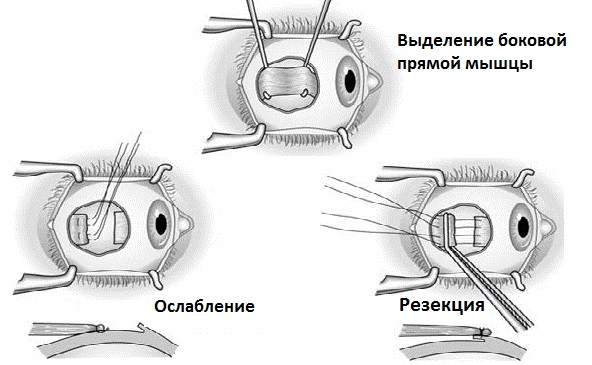
Surgery to correct strabismus in adults is not always indicated; the recommendation for surgery depends on a number of clinical and anamnestic characteristics (heredity, age, acquired or congenital type of strabismus, etc.). In some cases, for example, the operation is aimed at restoring the natural muscular balance in the eye muscles: a poorly functioning muscle is surgically strengthened or weakened. There are various techniques - resection, recession (shortening) of the muscle, relocation of the point of attachment, etc. Usually not just one, but several overly tight or relaxed muscles need to be corrected surgically; in some cases both eyes have to be operated on, in others only the squinting eye is corrected. As a rule, the operation is planned and carried out in several steps.
Causes of Squinting
- Myopia, hyperopia and astigmatism of varying degrees
- Central nervous system disorders and stress
- complications after infectious diseases;
- traumatic eye injuries;
- acute deterioration of visual acuity in one eye.
In persistent squinting, the protective mechanism of the central nervous system blocks the image of the squinting eye to prevent double vision. The result is a decrease in vision and the development of amblyopia, in which one eye is not used for vision.
A detailed computer-assisted exam, including a series of tests to check binocular vision, is performed to confirm the diagnosis and select a course of treatment.
How is the surgical correction performed?
The most reliable and effective method of treating strabismus in adults is surgery. The surgical procedure restores the symmetrical position of the eye axis. In surgical treatment, the surgeon works on the eye muscles and corrects the perceived squint by weakening or strengthening the muscles.
The operation is performed in one day and is completely painless as anesthesia is used. The patient can go home after the operation as hospitalization is not required. The recovery period after the operation lasts a week. During this period, it is necessary to follow the instructions of the ophthalmologist and continue therapy to normalize the visual function of the eyes.
Once both eyes are corrected symmetrically, visual function correction can proceed. Various techniques are used to improve vision, which are individually tailored to the patient's visual impairment.
To restore vision, special therapeutic eye exercises or apparatus therapy are additionally prescribed.
Causes of post-traumatic contractures of the shoulder, elbow, knee, etc.
As the name suggests, mobility impairment is caused by traumatic damage to components of the musculoskeletal system - bones, tendons, fascia, joints, ligaments, muscles and/or surrounding tissues such as skin, subcutaneous tissue, blood vessels and nerves. Statistically, limb injuries lead to the development of contractures seventy percent of the time.
These injuries can include puncture wounds, gunshot wounds, contusions, fractures, dislocations, burns, skull and spinal injuries. For example, when the integrity of the skin and deeper connective tissue structures such as muscles, ligaments and tendons are compromised, scarring in the joint leads to restricted mobility. Scarring tightens tissue and promotes adhesion formation; the latter form what is termed 'scarring'. additional fixation points - obstacles to free movement.
Among the most complicated contractures are those resulting from gunshot wounds. Because in addition to the musculo-fascial structures, blood vessels and nerves are also damaged.
Poor blood supply to tissues is an important factor in the development of contractures. It can be caused by edema, disruption of the integrity of large vessels, compression by tourniquet or plaster bandages, etc. This type of mobility restriction develops very quickly (within hours), in contrast to scar deformities, which take months to form.
Another important factor is pain, which triggers protective spasms. It can lead to a long-term limitation of movement, even if there is no serious tissue damage.
Limitation of mobility in one or more joints can also be caused by long-term immobilization of the injured limb. This can lead to changes in the joint capsule (loss of elasticity, shrinkage, thickening, adhesions, etc.) and replacement of muscle with connective tissue, etc.
The contracture is caused not only by the tissue damage itself, but also by its cause (muscle wasting, inhibition, subluxations, deformation of bone and joint structures).
Treatment of post-traumatic contractures
'Prevention is easier than cure'. Prevention of contractures is important and effective.
- Proper immobilization of the injured limb (in its natural position without undue compression of blood vessels and nerves) is an effective measure. Some doctors have experience healing fractures as quickly as possible without a cast.
- Early mobilization of the injured limb (passive and active exercises improve blood supply and nerve trophicity, accelerate healing and prevent scar tissue formation). When actual movement is not possible, visualizing a variety of movements gives good results. Experiments have shown that people who did not stop exercising during imagination recovered much faster and better, even after very serious injuries and long periods of complete immobility.
- Adequate early pain control and prevention of tissue swelling and hypoperfusion are the most important factors in contracture aggravation (anesthesia, physical therapy).
- If the injury does not require emergency hospitalization (or surgery), a session (or sessions) of osteopathy can have an excellent effect. In this area of medicine, the so-called 72-hour rule applies: After this period, the injury is fixed in the tissue. Within three days of injury there is a reasonable chance of returning the tissues to the 'matrix of health' and setting the stage for rapid and correct restoration of structural integrity and natural mobility.
What to do if the contracture has already occurred?
The key elements of a comprehensive approach are:
- positioning therapy. It aims to stretch the tissue (when it contractures, it is tight). This is achieved through the use of orthotics and splints. The requirements are continuity, little effort and great care not to cause additional tissue trauma.
- The movement therapy is called kinesitherapy: passive and active. The passive exercises are all about stretching the tissues. It is important that the muscles are relaxed (e.g. in warm water, in a suitable position, etc.). Active exercises (which are performed individually) are aimed at increasing the strength of muscles against contractures. Correct positioning and dosage of tension, gradually increasing amplitude and duration.
Prognosis and possible complications
Even if a person has undergone extensive treatment for irritable bowel syndrome and the symptoms have disappeared, it is important to remember that the therapy is effective in ⅓ of all patients and only 10 % achieve a durable remission. The clinical picture is wavy, that is, it is accompanied by periodic exacerbations. Symptoms usually remain for life but do not worsen provided the patient has diligently followed all medical recommendations.
The prognosis worsens if there is no or poor late treatment. Colitis, diseases of the liver and pancreas, disorders of the urogenital tract, erectile dysfunction in men, menstrual disorders in women, etc. can occur. However, a history of irritable bowel syndrome does not lead to malignancy or inflammatory bowel disease.
prevention
To prevent the pathological process, you should follow simple preventive recommendations:
- Eat healthy;
- Establish a drinking regime;
- Try to avoid stressful situations, control your psycho-emotional reactions, learn to relax completely;
- Follow a regime of work, rest, and sleep;
- Moderate physical activity, but avoid excessive exertion;
- regular walks in the fresh air;
- quit smoking and other bad habits;
- See a doctor and get checked out not only if you notice any suspicious symptoms, but also as a preventive measure when there are no health problems.
- 2 year old child with clubfoot.
- How to treat strabismus.
- How to treat clubfoot in a child.
- How to cure a clubfoot.
- kews is.
- Treatment of clubfoot in adults.
- Clubfoot correction in children.
- Which doctor treats adult posture?.
