Tarsal sinusitis is inflammation of the lining of the nose due to an infection that has entered the paranasal sinus. It is rare, occurring in no more than 2 % to 3 % of all cases of sinusitis.
- Use of MRI in diseases of the paranasal sinuses
- MRI in diseases of the paranasal sinuses
- Chronic rhinosinusitis
- Symptoms of cranial osteitis
- Methods for diagnosing frontal sinusitis (frontal sinusitis)
- How is sinusitis diagnosed?
- Treatment
- 1 Etiotropic treatment
- 2nd puncture
- 3. the 'JAMIC catheterization'.
- treatment of sinusitis
- How can pain in the frontal sinuses be relieved?
- What is chronic splenic inflammation?
- What Are the Complications of Vertebrobasilar Arteritis?
- Acute and chronic sphenoid sinusitis (sinusitis)
- Treatment of acute and chronic sphenoid sinusitis (cuneiform sinusitis), ozone therapy
- Additionally
- Diseases of the nasal cavity and paranasal sinuses
- What you can and cannot do about sinusitis
- Treatment of sinusitis (sphenoiditis)
- How common is this problem?
- Perforation in sinus lift surgery
- How our clinics proceed with the treatment
Use of MRI in diseases of the paranasal sinuses
There are a number of clinical conditions in which MRI can help clarify their nature and distribution. First a few words about the developmental variants, of which sinus hypoplasia and aplasia are the most common.Frontal sinus hypoplasiaParticularly noteworthy is the overpneumatization of the frontal sinus and posterior laminae in the form of pronounced superior lateral pockets, with which the internal carotid arteries and the optic nerve canals in it lumen can withdraw. Therefore, the clinical picture of progressive atrophy of the optic nerve can develop with inflammatory processes of the mucous membranes of these segments (including with subacute and chronic processes). Also, the risk of damage to the carotid arteries and optic nerves during surgical interventions in this anatomical region is several times increased.Developed upper lateral pockets, against which the optic nerves are delimited Inflammatory changes
MRI in diseases of the paranasal sinuses
There are a number of clinical conditions whose nature and distribution MRI helps clarify.
First, a few words should be said about the variants of development, the most common of which are sinus hypoplasia and aplasia.
A development variant that deserves special attention is excessive pneumatization of the cuneiform sinus and posterior laminae in the form of pronounced superior lateral pockets, in the presence of which the internal carotid arteries and optic nerve canals can retreat into their lumen. As a result, inflammatory processes of the mucous membranes of these sections (including subacute and chronic) can develop the clinical picture of progressive visual impairment. In addition, the risk of damage to the carotid arteries and optic nerves during surgical interventions in this anatomical region increases several times.
Chronic rhinosinusitis
is characterized by thickening of the mucosa due to mucosal hyperplasia and partial fibrous changes in the mucosa. The thickness of the mucosa varies between 4-5 mm.
Sinus polyposis, hypertrophic rhinosinusitis. Non-neoplastic inflammatory swelling of the mucosa.
Symptoms of cranial osteitis

In some cases, the disease can even cause paresis, paralysis of the nerve fibers of the bones of the skull.
Chronic splenitis is characterized by phases of exacerbation and remission:
- The patient suffers from visual disturbances;
- a purulent discharge from the nasal passages appears;
- Severe headache and fever occur.
Depending on the location of the inflammation, rhinosinusitis can occur on the left, right, or both sides.
The disease can be triggered by pathological processes in the nasal passages, abnormalities in the formation of the paranasal sinuses in childhood, cysts, polyps, tumors, injuries to the sphenoid sinus, narrowing of the paranasal sinuses, weak immunity.
Since the paranasal sinuses are quite deep in the cranial tissue, pathogens have to overcome the naturally created defense mechanisms in the nasal cavity (in the form of viscous mucus, cilia and hair, small size of the sinuses). Therefore, the frontal sinuses rarely become inflamed.
However, frontal sinusitis often occurs as a complication of infectious diseases such as influenza, pharyngitis or scarlet fever.
Methods for diagnosing frontal sinusitis (frontal sinusitis)
Due to the anatomical location of the paranasal sinuses, it is not easy to make a correct diagnosis. To put them effectively, it is necessary to involve several specialists: otolaryngologist, ophthalmologist, neurologist.
X-rays are not very helpful because the location of the paranasal sinuses is overlaid by other bones in the skull. A CT or MRI scan is more likely to be warranted. Nasal endoscopy is also done to locate the site of swelling and purulent exudate. Pharyngoscopy is also used.
In order to receive an accurate diagnosis of the disease, you should make an appointment with a specialist from the family doctor network.
How is sinusitis diagnosed?
For the diagnosis of the disease, it is necessary to collect a number of data: inquire about ailments, record the symptoms, analyze the patient's medical history and conduct an examination (X-ray, CT).
Possible symptoms: headache, pain in the temples, discharge from the nose and ears, accumulation of mucus in the back of the throat, poisoning (in severe cases).
Medical history should include information about previous medical conditions, trauma, hypothermia, etc.
The examination usually consists of palpation and percussion of the paranasal sinuses and includes a pharyngeal endoscopy and rhinoscopy.
Treatment
1 Etiotropic treatment
Prompt treatment can be aided by an antimicrobial drug (the main cause of acute sinusitis):
- β-lactams: amoxicillin, clavulanate, cefaclor, cefuroxime axetil;
- fluoroquinolones: levofloxacin, moxifloxacin;
- Macrolides: azithromycin, clarithromycin.
2nd puncture
This method is used when the disease cannot be cured with medication. This is the most well-known method of removing pus from the maxillary sinuses. Unlike the other procedures, it is quite painful.
3. the 'JAMIC catheterization'.
Very effective against maxillary sinusitis, without complications. The procedure is painful and, like LP, is not always well tolerated by patients.
Important: Surgical intervention is not advisable for an isolated sinus infection, as the infection can be transmitted to the healthy sinuses.
treatment of sinusitis

The pain from a sinus infection can be very severe and debilitating, making it difficult to move and think. Touching the face increases the pain and makes the skin more sensitive. The pain may be worse if the head is held down. To get rid of them, you have to wait until the inflammation subsides. When inflammation becomes chronic, the condition can last for months, worsen, or resolve.
Mild forms of sinusitis resolve spontaneously (60% of cases). However, if the person's condition does not improve within 10 days, a doctor should be consulted. Initially, nasal sprays are prescribed to clear the sinuses and antibiotics if the infection is bacterial. If the problem is due to anatomical features or tissue overgrowth, surgical treatment using an endoscope is recommended.
How can pain in the frontal sinuses be relieved?

So what can you do to make your life easier while your body fights the disease?
- Spray a saline solution into your nose most of the time. This swells the mucous membrane and liquefies the mucus that is clogging the sinuses. The nasal cavity should be rinsed at least 5-6 times a day. Alternatively, the nose can be irrigated with saline or weak saline using a large syringe without a needle, making sure that the liquid injected into the nasal cavity exits the other nostril.
- Avoid cigarette smoke, 'pungent perfume odors and household chemical odours' - they all irritate the lining of the sinuses, causing extra mucus production and consequently increasing pain.
- Use a humidifier. In wetter air, the mucus heals faster and the sinuses stay open. And the better the fluid drains from the sinuses, the less pain there is. If you don't have a humidifier, you can use an inhaler or a simple pot of hot water to inhale steam. Finally, you can also simply lie down in a hot bath.
- Place warm, moist compresses on your face in the sinus area several times a day to encourage fluid drainage.
- Drink more fluids - no matter what kind: water, juice, hot tea. Alcohol and drinks with a high caffeine content are not recommended during this time, as they dry out the body and cause the mucous membranes to swell.
- Use vasoconstrictors in the form of sprays or drops. They are especially effective in the early stages of the disease or during the cold season. However, this type of medication should not be taken for more than three days, otherwise there is a high risk of addiction.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) — naproxen, ibuprofen, or acetaminophen — can be taken for pain relief.
What is chronic splenic inflammation?
If a spleen infection lasts longer than 12 weeks, it is called chronic inflammation and is difficult to treat with conventional non-surgical methods.
- Acute headache, especially when tilting the head.
- In sphenoiditis, the pain is usually not localized but diffuse and occurs in the occipital, orbital, parietal, and temporal regions.
- Fever that can reach high values (39°C).
- Nasal congestion – not in all cases.
- Accumulation of secretions and mucus in the nasopharynx (often purulent).
- Unpleasant smell and taste sensation.
Sinusitis is more often combined with inflammation of the jaw and frontal sinuses. A single localization is rather rare.
What Are the Complications of Vertebrobasilar Arteritis?
If the inflammatory process does not subside due to the lack of or insufficient treatment, the infection migrates to the surrounding areas. Meningitis, encephalitis (collection of pus in the meninges), abscesses and cerebral vascular thrombosis can result. Other complications include visual disturbances and even permanent blindness.
After examining and questioning the patient, the otolaryngologist conducts a clinical examination with the help of nasoscopy (endoscopy). Endoscopy can be used to detect inflammatory (purulent) lesions in the paranasal sinuses.
This so-called endoscopy is not painful, but it can be uncomfortable. To avoid this, the nasal cavity is pretreated with a local anesthetic.
Computed tomography (CT) of the paranasal sinuses is required to diagnose sphenoiditis.
Acute and chronic sphenoid sinusitis (sinusitis)
Inflammation of the sphenoid sinus (sinusitis) is usually accompanied by inflammation of the ethmoid bone (posterior ethmoid inflammation), more rarely with a cold and sinusitis, so that the symptoms are usually similar to those described above. The headache associated with sphenoiditis is more often not localized and is felt in the occiput, orbit, crown, and temples. Secretion flows down the throat.
The diagnosis of sphenoiditis is made:
Treatment of sphenoiditis is usually conservative. However, with complicated ponsinuitis, ocular symptoms and intracranial sphenoiditis, surgical intervention is required.
Puncture of the sphenoid sinus in sphenoid sinusitis is performed after determining the exact angle of the needle in order to drain the contents of this inflamed cavity.
To diagnose sphenoid sinusitis, the sphenoid sinus is probed. If the olfactory cleft is wide, this is done under sight or under the surgical microscope. If the anatomical situation is unfavorable, the olfactory region should be thoroughly anesthetized and desensitized, the medial turbinate retracted with a Killian nasal speculum (if this is prevented by the natural opening at the bottom of the nose), and the paranasal sinuses probed by palpation. Probing is done with a slightly curved probe or cannula probe, which should be at least 10 cm long (the distance from the nasal entrance to the anterior sinus wall is about 8 cm in older children and adults, from the posterior edge of the nasal septum about 3 cm).
The method of probing for wedge sinusitis is as follows: A self-clamping nasal decongestant device is used. With the patient's head tilted back, the end of the probe is placed on the inferior edge of the nostril and the probe is passed along the nasal septum (without retracting laterally from it), along the inferior edge of the middle turbinate and into the natural opening of the paranasal sinus; sufficient feeling is generated. The wedge cavity can be cleared with a split cannula or a thin double-walled catheter no larger than 2 mm in diameter. If the natural opening of the maxillary sinus is small (about 1 mm), the probe will not penetrate the maxillary sinus. If it is brought closer forward from the center of the lower edge of the medial turbinate, it can penetrate the perforated plate and enter the cranial cavity. It is safe to go backwards from this marker. Failure may be due to the sphenoid sinus being present in many different forms, with accessory septa, ridges, and in rudimentary form or absent at all.
Treatment of acute and chronic sphenoid sinusitis (cuneiform sinusitis), ozone therapy
In the complex treatment of purulent sinusitis, it is recommended to combine it with local ozone therapy in the form of rinsing the inflamed paranasal sinuses with a physiological solution containing ozone in a concentration of 6-8 mg/l (to suck purulent secretions from the paranasal sinuses), followed by saturation of the mucous membranes with ozone by aerating the paranasal sinuses with an ozone-oxygen gas mixture (concentration 6-8 mg/l) for 15-20 minutes. Local ozone therapy is particularly indicated in cases of hypersensitivity to antibiotics and antiseptics. When the signs of inflammation and the discharge of pus decrease, it is advisable to reduce the ozone concentration to 3-4 mg/l in order to stimulate tissue regeneration.
Topical ozone therapy should be complemented by injection of a hydrocortisone suspension into the affected sinuses to reduce swelling of the sinus mucosa and anastomotic area. In patients with severe symptoms of intoxication, parenteral ozone therapy is also recommended by intravenous injection of a saline solution containing 0.8-1 mg/l ozone (400 ml per day, 3-6 infusions per treatment course). The duration of parenteral ozone therapy depends on the general condition of the patient and the resolution of the symptoms of intoxication. Given the relative instability of ozone in physiological solution, it is advisable to perform ozone transfusions via the droplet route.
Additionally
Diseases of the nasal cavity and paranasal sinuses
Diseases of the paranasal sinuses:
- Allergic rhinosinusitis, vasomotor rhinitis
- Hematomas and abscesses of the nasal septum
- Gonorrheic rhinosinusitis
- Deformations of the nasal septum (deviated septum)
- Diseases of the external nose: boils, eczema, ringworm, rhinitis, epistaxis
- Changes in the nasal mucosa caused by infectious diseases: influenza, diphtheria, measles, scarlet fever
- Foreign bodies in the nasal cavity
- Disorders of nasal breathing and the sense of smell in young children
- impairment of the sense of smell
- nosebleeds
- ozena
- Acute rhinitis, runny nose, nasopharyngitis
- Perichondritis of the nasal septum
- Post-traumatic synechia and nasal atresia
- Reflex nasal neuritis in adolescents and adults
- Nasopharyngitis-like conditions (rhinosinusitis) in adolescents and adults
- Subatrophic trophic rhinosinusitis and related diseases
- nasal injuries
- Removal of dry nasal crusts
- Chlamydial and trichomonas rhinosinusitis (cold)
- Chronic rhinitis: catarrhal, hypertrophic, atrophic
What you can and cannot do about sinusitis
The outcome of the disease depends not only on timely seeking medical help and the right choice of therapy, but also on the patient's willingness and ability to follow the recommendations of the specialist.
To quickly cure sinusitis at home and improve general health, it is recommended:
- Drink at least 1.5-2 liters of water a day. These may include herbal decoctions, infusions, green tea, alkaline water.
- Massage the sinuses. The massage stimulates microcirculation, improves nasal breathing and reduces swelling.
- Ensure a healthy diet. Avoid fatty foods, smoked meats, hot spices, salt, sweets and alcohol. Eat plenty of fresh fruits and vegetables, dairy products, lean meats and fish.
- Do breathing exercises. These exercises activate the airways, increase the body's resistance to germs, normalize blood flow and prevent inflammation.
- Rinse the nose regularly with running water or saline solution during the day to remove irritants and infections, moisten the nasal mucosa and prevent crusts from forming.
Self-medication is categorically forbidden, especially in infants, young children and pregnant women. It is forbidden to take medication without a doctor's recommendation, to engage in vigorous physical activity and to put onion, garlic or beetroot juice in the nose to avoid burning the nasal mucosa.
Heat treatment of bacterial sinusitis can be harmful. Heat increases the inflammatory process and promotes the spread of infection throughout the body.
Treatment of sinusitis (sphenoiditis)
Therapeutic measures are aimed at reducing swelling of the mucous membrane of the nasopharynx and sphenoid sinus, stimulating the outflow of pathological masses and fighting infectious agents. Depending on the severity and type of lesions, medication and/or surgery are used. The treatment program for sinusitis includes:
- antibiotic therapy. It is of crucial importance for the treatment. Initially, a broad-spectrum antibiotic is used, e.g. B. penicillins or cephalosporins of the second or third generation. If necessary, drugs should be changed after determining the sensitivity of the isolated microflora. If the disease is of viral or fungal origin, antiviral or antifungal drugs may be prescribed.
- Symptomatic pharmacotherapy. These include vasoconstrictive drugs to reduce swelling and suppress exudate. Antipyretics, analgesics and nonsteroidal anti-inflammatory drugs are used depending on the clinical picture. Severe poisoning is relieved by intravenous infusion therapy. Massive antibiotic therapy is supplemented with probiotics to prevent gastrointestinal disease.
- Surgical interventions. Surgical methods (sphenotomy) are used in productive forms of chronic sphenoiditis, when the patency of the entrance to the sphenoid sinus cannot be restored by other means and conservative treatment is ineffective. With the endonasal approach, the natural sinus port is visually expanded and the sinus cavity drained. In the extranasal variant, the maxillary sinus is opened by removing the posterior third of the nasal septum, the medial turbinate and the posterior lamellar protuberance.
How common is this problem?
According to a study by the University of Tokyo, sinus perforation is more common in men over the age of 30 who have had a first molar (sixth tooth) extracted.
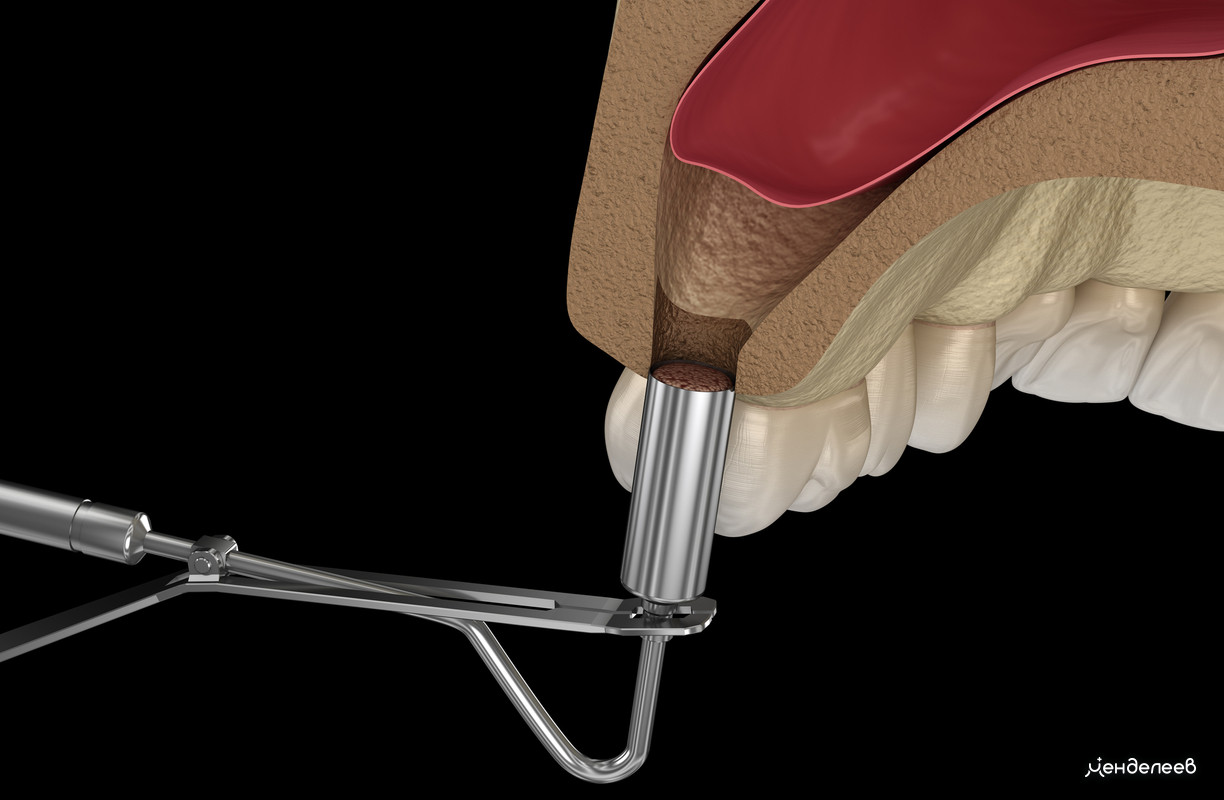
Perforation in sinus lift surgery
A maxillary sinus augmentation is a surgical procedure performed prior to the placement of dental implants because the bone volume in the upper jaw is insufficient to accommodate the implants. This procedure differs from other bone grafting procedures in that it is performed in the maxillary sinuses to make room for the implants.
The procedure is carried out with the aim of eliminating them:
However, simply lifting the maxillary sinuses can result in perforation. During the operation, the maxillary sinus membrane (Schneider's membrane) is separated from the periosteum and raised to create space for bone material. During the introduction of the osteoplastic material there is a risk of perforating the maxillary sinus.
Trauma to the maxillary sinus in maxillary augmentation is common when:
- the practitioner did not adequately examine the patient's jawbone in the preparatory phase,
- the procedure is a closed sinus post and the practitioner has limited room for manipulations in the maxillary sinus area,
- the bone was built up with outdated technology,
- the patient was born with large and thin-walled maxillary sinuses.
If a perforation occurs during the sinus inlay, the hole must be closed by microsurgical interventions. In the worst case, the maxillary sinus can become inflamed and infected. The treatment measures depend on the diameter of the perforation:
- Up to 2mm. The injured mucosa heals spontaneously and without surgery.
- 2-4mm . Spontaneous healing is not possible. Immediate surgical closure of the hole may be sufficient to prevent infection. Bone augmentation can be continued without sutures.
- More than 4mm . If significant perforation occurs during augmentation, the procedure must be postponed until the maxillary sinus has healed.
How our clinics proceed with the treatment
Implantologists and surgeons with an experience of 15 to 22 years work in the Dental Clinic 'Mendeleev'. Before treatment, we conduct a thorough diagnosis of the patient with the help of a CT scanner. This allows us to choose the safest and most effective treatment method.
The dental microscope is used in endodontic treatments, dental implants and other surgical or therapeutic procedures. Its multiple magnification helps the dentist to closely monitor the course of treatment and reduce the risk of postoperative complications.
Read more:- sphenoid.
- hole in the eardrum.
- Those are the pluses.
- Transverse arch of the foot Latin.
- interdental membranes.
- Arching of the foot in man.
- Tibiofibular ligament.
- Pain in the periosteum of the tibia.
