The causes of hip dysplasia also include factors affecting the overall development of the fetus – radiation, nutritional factors (lack of alcohol, protein and vitamins), infectious diseases, drug use, thermal factors, the general condition of the woman during pregnancy, etc.

- hip dysplasia
- classification
- diagnostic procedures
- Treatment
- complications
- diagnostic procedures
- Treatment
- complications
- Causes of congenital hip dislocation
- Features of the joint in disease
- Diagnosis of dysplasia in children
- consequences of hip dysplasia
- Complications and consequences of hip dysplasia
- Diagnosis of hip dysplasia
- Hip lengthening with the Bliskunov apparatus with different types of osteotomy
- keywords
- Causes of delayed hip development ↑.
- Types of dysplasia ↑.
- Signs of delayed hip development ↑.
- symptoms
- diagnosis
hip dysplasia
This disease is associated with a congenital disorder of the formation of the hip joint. The severity of the disease varies greatly, ranging from a weak ligamentous apparatus to a significant defect.
Hip dysplasia in newborns can be caused by the following factors:
- inheritance. Parents who had dysplasia themselves as children are at higher risk of having a child with dysplasia symptoms.
- The tradition of wrapping the baby tightly in a duvet. It has been statistically proven that babies whose legs are swaddled upright are more likely to be ill than other children.
- Presentation of the buttocks. Hip dysplasia is more common in babies who are late in breech presentation. The development of the defect is favored by fetal malformations and the first pregnancy.
- Hormonal abnormalities in women. An underactive thyroid in the mother-to-be can lead to abnormal development of the connective tissue in the child.
The risk of dysplasia also depends on the gender of the child. Girls are mostly affected.
classification
There are the following variants of hip dysplasia
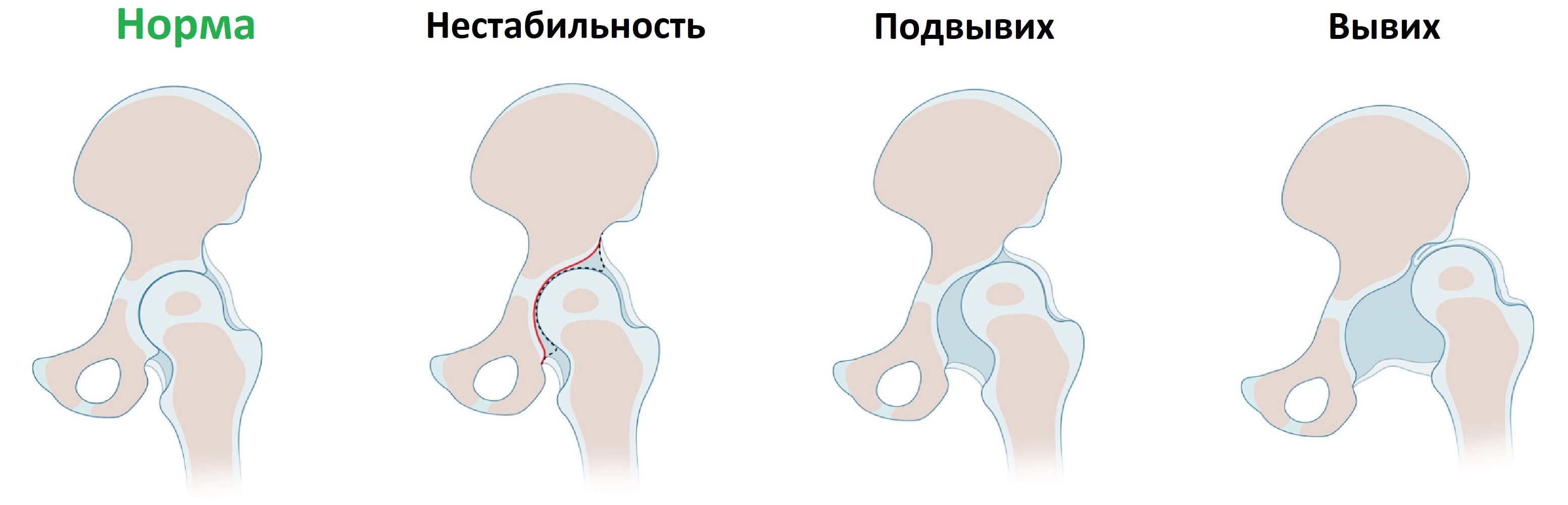
- predislocation. The femoral head is in the normal anatomical position: it lies in the sclera. It is systematically dislocated and returns to its original position due to abnormal stretching of the joint capsule.
- Subluxation – the head of the femur is displaced upwards and to the side, but cannot exit the acetabulum.
- Hip dislocation is characterized by a complete separation of the joint structures. The head of the femur completely exits the socket.
In the case of a hip dislocation, on the other hand, 5 degrees of severity are distinguished. At the most severe degree, the head wanders into the hip wing area (upper pelvic region).
diagnostic procedures
The diagnosis of a femur fracture is based on the assessment of the symptoms, the medical history, the clinical examination and instrumental examination methods to confirm the diagnosis. Diagnosis aims to determine the type of fracture, the severity of the disease, and the complications that are present.
Based on the medical history, the mechanism of the fracture – car accident, fall from a height, fall on the hip joint – and the factors associated with the injury – osteoporosis (advanced age or metastases in bone tissue) – can be determined.
Instrumental examination of a patient with a suspected proximal (femoral neck) fracture begins with a radiological examination - an X-ray of the pelvis, a plain and axial X-ray of the proximal thigh and hip joint on the side of the injury.
For fractures of the proximal segment (femoral neck fractures) and in some cases for intra-articular fractures, computed tomography is performed for clarification.
General blood and urine tests, as well as routine biochemical blood tests, have no independent value and are carried out to assess the current state of health, the diagnosis of the underlying disease and possible complications.
The most important laboratory tests are:
The main instrumental tests:
Treatment
The treatment of the thigh fracture is recommended by the accident surgeon. Since the surrounding tissues, including blood vessels, are damaged by the fragments' displacement, timely medical attention can prevent complications such as bleeding.
In the first place, the limb must be immobilized in the position in which it was stored and no attempt should be made to set the broken bone yourself, as such an attempt may damage the vessels surrounding the bone and cause bleeding. The second rule of immobilization is to immobilize the joints above and below the fracture and, in the case of a hip fracture, the ankle as well. If there is a wound, it should be treated with antiseptics and a bandage applied. Painkillers should be given to relieve pain.
Intra-articular fractures are treated surgically with three-pin immobilization. A complication of treating femoral neck fractures is the formation of a false joint or aseptic necrosis of the femoral head. If this is the case, a hip prosthesis may be required after the operation. In the case of a hip fracture, skeletal traction is performed for 8 weeks and then a plaster cast is applied. Surgical treatment - osteosynthesis with a triangular shaft, plates and screws - is also possible. Surgical treatment shortens healing time.
complications
Bleeding, fat embolism, pain shock, bone inflammation, complete limitation of movement, trophic disorders (wounds, ulcers) are possible.
diagnostic procedures
The diagnosis of a congenital dislocation of the hip is based on the collection of anamnestic information and an objective examination. The diagnosis is confirmed by imaging methods - ultrasound and X-rays.
To establish the diagnosis, the following manipulations are performed: with the child in the supine position, the doctor slowly stretches the legs, bent in the knees, to an open angle so that they practically touch the table surface. If there is an anomaly in a hip, a slight tremor is felt, which corresponds to the moment when the head falls out of the joint. If the hips are then brought into a central position, there will eventually be a jerky movement that can be visually perceived on the affected side.
To confirm the diagnosis, the child undergoes an ultrasound scan and an x-ray of the hip joints. X-ray examination and its variant, arthropneumography, are considered the most important examination method. A comprehensive indexation of the hip joint is made on the basis of radiographs and arthrograms, which is essential for a complete understanding of its structure to predict further pathologies. The spatial position of the pelvic and femoral components of the joint, the size and shape of the acetabulum and femoral head, the relationships in the hip joint, the bony structure of the acetabulum, femoral head and femoral neck, the condition of the Y cartilage and metaepiphyseal growth plate, as well as the degree of ossification of the femoral head.
An ultrasound examination can be used to clarify the joint conditions, taking into account the cartilaginous parts of the hip socket and femoral head. CT examinations clarify changes in the structure and the spatial position of the joint components.
The main instrumental studies are:
- X-ray of the hip joint.
- X-ray examination with contrast medium (arthropneumography).
- Ultrasound examination (ultrasound of the joint).
- Computed tomography (CT scan).
Treatment
The most important condition for improving the treatment of congenital dislocation of the hip is early detection of the pathology, the earliest possible use of orthopedic treatments and the prevention of further progression of the disease.
The currently accepted treatment methods for congenital hip dislocation are various types of bandages that hold the hip in abduction and allow movement of the hip joint. Preserving joint mobility in the treatment of congenital dislocation of the hip is considered the most important method of preventing the development of dystrophic processes in the femoral head. In children up to the age of 1 year, the treatment is conservative with functional appliances and physiotherapeutic methods. From the 5th to 7th day of life, functional splints are used in infants with clinical signs of hip dislocation. In addition to the splints, devices with the same function, such as e.g. B. Pavlik stirrup, used to ensure the correct position of the femur in the acetabulum.
The infant should be rocked extensively. Range of motion exercises with buttock massage play an important role in restoring joint function. With the growth of the bone and under the influence of the measures taken, the head gradually retracts into the natural socket of the joint.
If the child has not developed a congenital hip dislocation and more than a year of unsuccessful conservative treatment has passed, surgical treatment may be required, which includes open surgery of the femoral head with its immobilization in a physiological position. If a new joint has already formed (neoarthrosis) and the disease is progressing, it may be necessary to surgically replace the joint with a synthetic joint prosthesis.
complications
A serious complication of congenital dislocation of the hip is the development of deforming coxarthrosis and loss of joint function, which leads to disability of the patient. Without proper treatment and as the disease progresses, spinal curvature and osteochondrosis develop. Walking is impaired due to the difference in length of the limbs.
Causes of congenital hip dislocation
A combination of causes can be responsible for the development of a hip dislocation. If certain risk factors are present, the probability of developing the disease increases significantly. This includes:
- brainless fetal presentation;
- poisoning;
- Alcohol and drug abuse, significant vitamin, mineral and protein deficiencies, as well as a number of infectious diseases during pregnancy;
- hereditary predisposition;
- multiple pregnancies;
- high birth weight of the baby;
- low body water content;
- Damage to the baby's bones and ligaments during passage through the birth canal;
- Drug treatment during pregnancy.
There are several theories about the origin of this pathology, one of them is the hormonal theory. Scientists suspect that an imbalance between two hormones - progesterone and estrogen - could be a key factor. In experiments on rats, it was found that an increase in the level of estrogen inhibits the development of dysplasia, while an increase in the level of progesterone, on the contrary, promotes this process.
There is another theory for the origin of the disease, which is related to the impact of mechanical factors during intensive growth. In the prone position and high fetal weight, deforming forces act more strongly on the hip joint. A direct association has been found between increased morbidity and the tradition of tightly swaddling the baby with stretched legs.

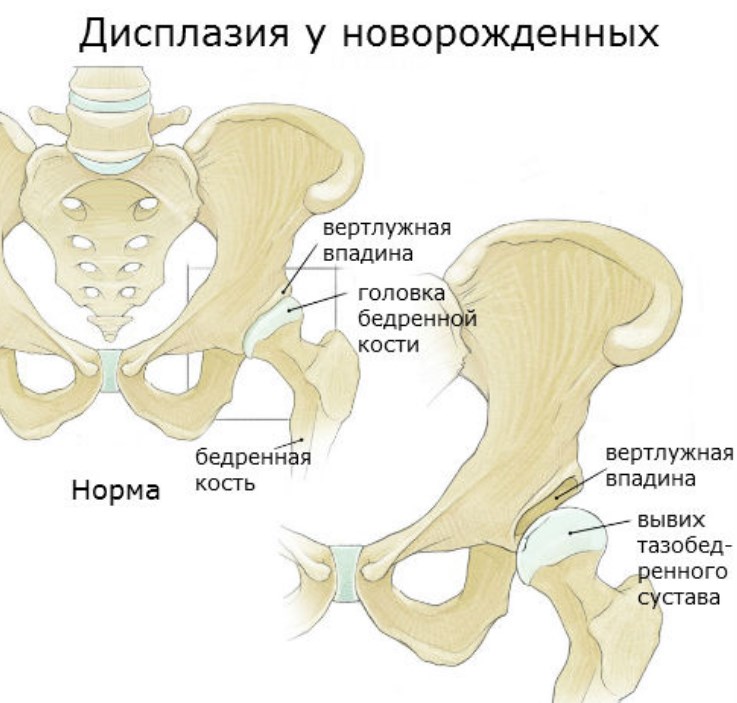
Features of the joint in disease
The hip joint consists of the femoral head and the acetabulum, with a cartilage plate attached to the top of the joint, which increases the contact area of the articular surfaces and the depth of the acetabulum. The newborn joint has some peculiarities, and even if there are no pathological processes, it is an immature structure.
Compared to the adult joint, infants have a flattened socket that stands more erect and overly elastic ligaments. The fixation of the femoral head in the articular surface ensures tension in the joint capsule and its own ligament. On the articular surface is a cartilaginous lamella - the limbus - that prevents the thigh bone from moving.
Depending on which hip joint is more affected, different types of dysplasia can be distinguished:
- Acetabulum: Abnormalities of the acetabulum - flattening, reduction.
- Rotation: changes in the geometry of the bone in the horizontal plane.
- Associated: with underdevelopment of the upper parts of the thigh.
In the disease, the relationship between the joint structures changes as well as their shape and size. The acetabulum flattens, the ligaments and capsule are no longer able to hold the femoral head in place, and the femoral head is displaced from its normal position. The cartilage plate deforms and can no longer fully fulfill its function, ie it can no longer absorb the displacement of the femoral head.
Subluxation can occur during sudden abnormal movements when the femoral head partially protrudes beyond the acetabulum. A more complicated situation can also occur when the head protrudes completely from the socket of the hip, known as a dislocation. If this is not treated promptly, the acetabulum will gradually fill with fatty connective tissue, making it very difficult to reinsert the joint.
Diagnosis of dysplasia in children
The suspicion of hip dysplasia in a newborn can already be expressed in the maternity ward. If there is a suspicion of pathology, doctors strongly recommend a visit to a pediatric orthopedist within 3 weeks after discharge. Children with a suspected diagnosis and the presence of several risk factors are examined by a specialist every 3 months.

Diagnosis of hip dysplasia in children includes:
- A clinical examination of the child by an orthopedist. During the examination, the doctor assesses the symmetry of the legs and determines whether Marks-Ortolani symptoms are present or not.
- X-ray examination of the hip joints. Conducted only in children over 3 months of age, since at a younger age this diagnostic method is ineffective.
- Hip ultrasound is the gold standard for diagnosing dysplasia.
A definitive diagnosis is only made through a combination of clinical signs and instrumentally proven joint lesions.
consequences of hip dysplasia
Minor joint changes caused by dysplasia may not be apparent at a young age. However, the risk of developing dysplastic hip osteoarthritis increases with age. The more pronounced the pathological changes, the earlier coxarthrosis occurs. In some patients, it develops as early as 25-27 years of age. The first symptoms of coxarthrosis, as a rule, appear with reduced physical activity, and in women it very often manifests itself during pregnancy.
The typical symptom of dysplastic coxarthrosis is a sudden onset and rapid progression. First, there are unpleasant sensations when moving, followed by pain and reduced joint mobility. As the disease progresses, the hip becomes misaligned – the leg is turned to the side and slightly bent at the hip joint.
Severe dysplasia with true hip dislocation and premature hip dislocation can result in incomplete nonunion. This complication is almost non-existent in the modern world thanks to a good diagnosis.
Complications and consequences of hip dysplasia
Left untreated or undertreated, hip dysplasia gets worse and leads to the following complications
- Muscular dystrophy;
- Chronic back and limb pain;
- lower body deformity;
- dysplastic coxarthrosis;
- gait deformities;
- impaired mobility of the spine;
- neoarthrosis;
- spinal curvatures;
- Claudication of varying degree and form.
Over time, a new, incomplete joint can develop, which is associated with leg shortening and muscle wasting. Such a joint takes over some of the functions of the hip joint, but not all.
Diagnosis of hip dysplasia
The initial diagnosis is sometimes made within the first few hours after birth. The doctor always examines the newborn to make sure the child is okay. The baby is palpated and examined after breastfeeding in a quiet environment. To confirm the diagnosis, an additional examination is prescribed, which includes, among others, the following procedures:
- Ultrasound – to determine the cause and location of the anomaly;
- X-ray – in adults and children over one year old;
- CT, MRI to assess the condition of the ligamentous apparatus.
Diagnosis of hip dysplasia is made by correlating clinical symptoms with changes seen on ultrasound and radiographs. Since the skeletal system is not yet developed in small children, a special marking method is used to decode it. Conventional lines are drawn on the frontal projection images to determine the acetabular angle. These lines are used to determine if there is an anomaly.
Hip lengthening with the Bliskunov apparatus with different types of osteotomy
A total of 174 patients underwent hip lengthening using a fully implantable, guided device powered by the patient's muscular strength. Bone is removed from the side of the medullary canal with a specially designed osteotome that allows transverse, oblique, anterior oblique, straight Z-shaped, and oblique Z-shaped osteotomies. A transverse osteotomy was performed in 59 (33.9 %) cases, an oblique osteotomy in 70 (40.6 %), an anterior oblique osteotomy in 19 (10.9 %), and both Z-shapes (straight and oblique) in 26 (14.9 %). The distraction phase was completed in all patients. Lengthening was achieved as planned in 165 (94.8 %) of 174 cases and 150 patients had their devices removed. The mean distraction rate was 1.4±0.3 mm/day, the mean duration of the distraction period was 87±13 days. A good result was obtained in 141 (94 %) out of 150 cases, a satisfactory in 7 (4.6 %), an unsatisfactory in 2 (1.4 %). Complications were observed in 30 (17.2 %) of the 174 cases. They affected the outcome in 9 (5.2 %) cases. Analysis of complications showed that they could be largely avoided by strict adherence to distractor implantation technique, osteotomy procedure, distraction rate, and rational postoperative management.
keywords
Correction of inequalities in limb length, correction of deformities and lengthening of paired segments is today without periosteal osteosynthesis, whose achievements are named GA Ilizarov, MV Volkov, OV Ohanesian,
VK Kalnberz, ON Gudushauri and others. With the advent of extrafocal compression-distraction devices, achievements have also been made in solving such a difficult problem as hip extension. However, the attention of orthopedic surgeons remains focused on the disadvantages that are most apparent in the use of braces in this segment of the lower limb. This is partly due to the fact that complications occur more frequently and more severely here than in the lower extremity [1, 4-8, 10-12, 14-16, 18].
We believe that the disadvantages of external extramedullary devices should not be dramatized: if the method is used correctly, they outweigh the advantages. The implantable devices described below should not be viewed as competing, but as a distinct direction of limb lengthening.
The complications of ectopic hip lengthening cannot convincingly demonstrate the superiority of one device over the other due to the different composition of the compared patient groups, but the technology still brings between 3 % and 78 % of complications. To date, the main cause of complications has been persistent perforation of the skin by pins or rods.
The history of implantable devices goes back about 40 years. The first two developers were never able to eliminate the prolonged skin perforation. Solimei's [19] device, described in 1959, communicated with the external environment through a high-pressure hose, while Schollner's [17] device communicated with the external environment through a polychlorinated vinyl hose. Only Bruns et al. [13] eliminated this disadvantage, but their device required the patient to lie next to the energy source throughout the extension period.
Causes of delayed hip development ↑.
The most common causes of hip dysplasia are:
- Maternal infectious abnormalities during pregnancy;
- Endocrine disorders during pregnancy;
- Severe toxicosis, especially in the first trimester;
- late pregnancy;
- Unbalanced nutrition of the expectant mother - lack of vitamins, minerals (especially calcium);
- family predisposition.
Types of dysplasia ↑.
Depending on the consequences of the underdevelopment of the hip, several types of dysplasia are distinguished:
- Grade 1 - is characterized by instability of the hip joint, known as preloaded. There is no displacement of the femoral head relative to the acetabulum.
- Grade 2 - the femoral head is partially displaced from the acetabulum, this is a congenital hip subluxation.
- Grade 3 - involves complete dislocation of the femoral head from the socket. This is a congenital dislocation of the hip joint.
degree of hip dislocation
The initial diagnosis is usually made by an orthopedist during a routine examination at the end of the neonatal period. The presence and extent of the anomaly is clarified by an ultrasound examination of the joint and x-rays.
Signs of delayed hip development ↑.
In an infant up to 1 year old, dysplasia manifests itself in varying degrees as follows:
- Limitation of hip abduction - the severity of the symptom depends on the degree of impairment. Maximum restriction of movement with dislocation of the hip joint. To identify the symptom, with the child in the supine position, bend both legs at the knee and hip joints and spread them slightly. The abduction obstruction is clearly visible on the affected side.
- Presence of skin fold asymmetry: lie on your stomach, stretch your legs and carefully examine the folds of the buttocks and thighs. This symptom is rather vague, but when it is present, hip dysplasia is suspected.
- Clicking sign – a clicking sound is heard or felt in the dysplastic joint during abduction. The noise is caused by the head of the femur pressing into the socket of the joint. This is also an implicit symptom and is usually seen in infants in the first few days of life. However, in the case of hip dysplasia with muscle hypotonia, this symptom persists until 6 months of age.
- Shortening of the legs - clearly visible when the baby is lying on his back and his knees are bent.
- Excessive outward rotation of the affected limb - seen when the child is in a relaxed position e.g. B. in sleep.
symptoms
The symptoms of Perthes disease depend on the degree of necrosis and the size of the necrosis. In the early stages of Perthes disease, symptoms may be absent or minor. Children may complain of moderate pain in the hip or knee region.
Gait disturbances (dragging of the foot) can also occur. This latent healing in the early stages of Perthes disease (osteonecrosis stage) means that the disease is rarely diagnosed and treated in its early stages. As the necrosis progresses, the femoral head deforms, leading to changes in the biomechanics of the joint and symptoms such as claudication, leg pain, and joint pain. Extrusion fractures in the area of necrosis can result in limb shortening, which can be detected by visual inspection.
diagnosis
X-rays are the most important method for diagnosing Perthes disease. As a rule, x-rays of the hip joint are prescribed in anteroposterior and Lauenstein projection. In addition, MRI and ultrasound of the hip joints can be performed to more clearly identify morphological changes. Laboratory tests are necessary to differentiate it from other possible hip diseases.
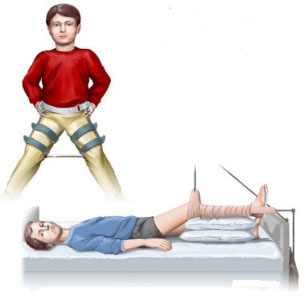
Perthes disease can be treated conservatively or surgically.
Conservative treatment is based on therapeutic measures that ensure centralization of the femoral head (ie full immersion of the femoral head in the acetabulum). Once Perthes disease is diagnosed, bed rest and leg rest (only walking with crutches) is recommended. To maintain alignment, special orthopedic braces (Vilesky, Mirzoev, Lange plaster casts and others) are used. Permanent centering is particularly necessary when the area of necrosis is large. In addition to orthopedic aids, massages, medication, physiotherapy and physiotherapy are used. Therapeutic measures are carried out in courses of 2-4 weeks with intervals of 1 month. Therapeutic exercises must be performed daily. The duration of conservative treatment with full (or partial) weight bearing of the affected limb ranges from 1 to 4 years on average. The duration of treatment depends on the age of the child and the degree of pathological changes at the beginning of treatment. Dose loading is permissible only with positive dynamics on the X-ray image (MRI) of the joint.
However, with pronounced thigh deformity and hip subluxation, surgical reconstruction of the joint is often required. The advantage of surgical treatment of large dislocations is that there is no need to wear a long-term orthosis and the rehabilitation time is shorter.
Read more:- external rotation of the hip.
- Legs of different lengths in a child.
- Leg splint for newborns.
- The child has a shorter leg than the other.
- outward rotation of the leg.
- leg brace.
- Shortening of the lower limbs.
- hip pronation.
