There are usually three grades of medial collateral ligament tears in the knee:

- Rupture of the collateral ligament of the knee.
- causes
- Anatomical structure of the knee joint
- collateral ligaments
- cruciate ligaments
- Instability and types of ligament injuries
- High angle view of radiologist woman and her patient having knee MRI scan in clinic_637285-467-1.jpg
- Chiropractor stretching an elderly patient's legs for physical therapy_482257-26989-1.jpg
- stiffening of the ligaments
- ligament stapling
- Causes of rupture
- trauma
- tendonitis
- General weakness of the tendon ligament
- diagnosis of the injury
- Diagnosis by X-ray examination
- diagnosis
- Conservative treatment
- surgical treatment
- Video about our clinic for traumatology and orthopedics
- Duration of the operation and recovery period:
- Comments and explanations:
- Symptoms of a tear of the medial collateral ligament in the knee joint
- Treatment of a medial collateral ligament tear
- Conservative treatment
- diagnosis
- Treatment of meniscus injuries
Rupture of the collateral ligament of the knee.
A tear in the collateral ligaments of the knee occurs primarily in athletes. The intrinsic ligament is torn more often than the extrinsic ligament. There are 3 degrees of injury based on the radiological findings. With a grade 1 injury, the patient recovers with conservative treatment. In Grade 2 injuries, the torn ligament usually needs to be repaired arthroscopically. In the case of a complete rupture, plastic surgery using the body's own material or Lavsan tapes is required. Untimely treatment can lead to chronic instability of the knee and the development of osteoarthritis.
Ruptures in the collateral ligaments of the knee occur primarily in athletes. Inner ligament tears are more common than outer ligament tears. There are 3 degrees of severity of the injury, which are determined by the radiological picture. With a grade 1 injury, the patient recovers with conservative treatment. Grade 2 injuries usually require arthroscopic repair of the torn ligament. In the case of a complete rupture, a plastic treatment with endogenous material or Lavsan tapes is required. Untimely treatment can lead to permanent knee instability and osteoarthritis.
- Affordable Visit to an orthopedic trauma surgeon, MD from 4,000 rubles
- Urgent Prompt appointment on the day of treatment
- Near 8 minutes from Prospekt Mira metro station
- Comfortable Private appointment by appointment
Ruptures in the collateral ligaments of the knee occur primarily in athletes. Internal ligament tears are more common, external ligament tears are less common. There are 3 degrees of injury, which are determined by the radiological findings. With a grade 1 injury, the patient recovers with conservative treatment. Grade 2 injuries usually require arthroscopic repair of the torn ligament. In the case of a complete rupture, a plastic treatment with endogenous material or Lavsan tapes is required. Untimely treatment can lead to permanent instability of the knee and osteoarthritis.
causes
There are two ligaments inside and outside the knee joint. Any of these ligaments can tear as a result of direct (leg kick) or indirect trauma. The cause is an inward or outward tilting of the tibia.
When the tibia tilts inward, the lateral collateral ligament of the knee joint tears. Its job is to limit this movement. However, if the force is too great, the belt will fail and tear.
The mechanism of injury on the other side is similar. The medial collateral ligament of the knee joint tears when the tibia is pivoted outward with great force.
The inner collateral ligament tears much more frequently than the outer ligament. It usually occurs as a result of a direct hit to the knee or shin, twisting of the leg, sudden loss of rotation, or an awkward landing after a jump. The injuries mainly occur in athletes. Similar injuries can also occur in traffic accidents, but they are usually multiple (as a concomitant of other limb injuries).

Anatomical structure of the knee joint
The knee joint consists of the kneecap (patella), which also protects it to a certain extent, as well as the tibia and femur.

Figure 1 shows the normal anatomical structure of the knee joint, which consists of four main components: meniscus, bone, ligaments and tendons.
As previously mentioned, the bony elements of the knee are connected by four major ligaments that keep them a safe distance apart, ensuring the stability of the knee in all types of movement.
The major ligaments consist of the collateral ligaments (medial and lateral) and the cruciate ligaments (anterior and posterior).
collateral ligaments
The collateral ligaments of this group are located on the sides of the knee joint - the lateral ligaments on the outside, the medial ligaments on the inside. Their main function is to control the movement of the lateral bone elements and to prevent even the slightest possibility of their movement, even in relation to each other.
cruciate ligaments
The ligaments of this group, which cross each other in an X-shape, are located in the inner part of the knee joint. Their primary role is to prevent the tibia from moving forwards and backwards relative to the femur.
Instability and types of ligament injuries
Because the stability and proper functioning of the knee joint is directly dependent on the ligaments that connect the joint to muscle tissue, injuries of all kinds to these ligaments are very common. The most common causes are not only direct trauma to this area, but also extremely violent contractions of muscle tissue, such as B. a sudden change in pace while running.
In practice, experts distinguish between the following degrees of ligament injuries:
1st degree: the mildest, characterized by a slight stretching of the tape while maintaining its basic stabilizing properties;
2nd degree: characterized by a greater dislocation with partial or complete loss of the stabilizing function. This degree of damage is often referred to as a partial tear;
Grade 3: In this grade there is a complete rupture of the ligament into 2 fragments accompanied by loss of stability of the knee.
It is not uncommon for specialists to find two or more torn ligaments at the same time. With such serious injuries, there is damage to the nerves responsible for the work of the leg muscles, as well as a significant disruption in the blood supply to the tissues. In severe cases, the patient is at risk of limb amputation.
According to medical practice, the medial ligament is the most commonly damaged ligament. However, due to the anatomical differences in the outside of the knee, collateral ligament injuries are often exacerbated by injuries to other, nearby parts of the joint.
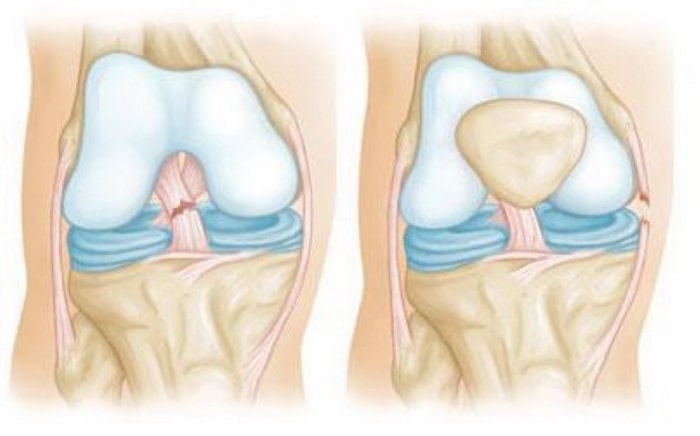
A cruciate ligament tear (left) often leads to destruction of the inner ligament (right).
High angle view of radiologist woman and her patient having knee MRI scan in clinic_637285-467-1.jpg

Oblique view of a radiologist woman and her patient during the knee MRI scan in the clinic_637285-467-1.jpg
The basic principle of conservative treatment is to bring the medial (tibial) ligament of the knee to a state of complete functional rest. This creates the necessary conditions for the healing of the torn fibers. At the same time, the symptoms in the acute phase (pain relief, regression of the swelling) are controlled.
In the acute phase, the person concerned is carefully examined immediately after the injury. The medial collateral ligament tears most commonly after an impact on the lateral surface of the knee. This is usually a sports injury. It can be accompanied by damage to other intra-articular structures (meniscus, joint capsule, ligaments).
Sometimes surgery is done soon after the injury. However, if only the inner collateral ligament is damaged, conservative treatment is performed. The knee is punctured, irrigated, and the blood removed. A local anesthetic is given internally to relieve pain. Usually 0.5 % procaine is used. A plaster splint is applied for 1 week. Once the joint swelling has subsided, it is replaced with a circular cast from the groin to the toes.
If the medial collateral ligament of the knee joint is torn, the tibia is brought into a lying position. This immobilization allows limited mobility of the leg in the area of the injured joint. Limb positioning reduces stress on the damaged ligament. The ligament is held in a relaxed position for an extended period of time so that an appropriate regeneration process can take place.
- Physiotherapy – various methods are used to improve blood circulation in the joint, accelerate edema elimination and normalize regeneration processes;
- Therapeutic exercises – static exercises are recommended from the third day, while dynamic exercises to strengthen the muscles of the limbs are used in the recovery period (after removing the plaster cast);
- Arthrotherapy – injections into the joint with hyaluronate and platelet-rich plasma, which accelerate tissue regeneration and prevent cartilage degeneration.
Chiropractor stretching an elderly patient's legs for physical therapy_482257-26989-1.jpg

Chiropractor extending leg of an elderly patient for physical therapy_482257-26989-1.jpg
Surgical treatment of a torn medial knee ligament is required when it is completely torn and joint instability persists. This can be partially alleviated by special orthopedic restraints. However, sooner or later this condition leads to gonarthrosis and muscle wasting. The earlier the operation is performed, the better the results.
stiffening of the ligaments
There are several ways to stabilize the knee in the event of a medial ligament tear. One of them is plastic surgery. The material used is an autograft. This means that tissue with similar properties is taken from the human body. This is implanted in place of the torn ligament. A fragment of the vastus femoris is often removed for this purpose.
An autograft with a tendon of the tendon muscle is used. A bone adhesive suture is placed in the medial epicondyle of the thigh. The tendon is placed underneath. The flap is then secured with sutures. The wound is stitched up. The limb is immobilized with a plaster cast for 4 weeks. The cast is applied from the upper third of the thigh down to the toes. The knee should be bent at 170 degrees.
ligament stapling
This operation is often performed in the acute phase of the injury, no later than eight days after the injury. It can also be carried out within the first three days. That is, almost immediately after the injury, even if swelling and hematoma are still present. Early intervention improves the outcome of the operation.
If the superficial flap of the medial collateral ligament of the knee is torn, the area of the tear is sutured. The doctor detects the formation of a hematoma at the site of the tear. In addition, he can locate the site by retracting and adducting the tibia: the ends are divergent. The doctor sews the band across, grasping 1 cm above and below the injury site. The tape is then sewn lengthwise. If a piece of bone detaches, it is held in place with a screw and washer.
Causes of rupture
trauma
Because tendon tissue is very strong and elastic, it takes a great deal of force to induce a tendon rupture, especially a full one.
Jump. Excessive contraction of the quadriceps muscle upon landing in a jump when the knee is in a flexed position is considered one of the most common causes of native ligament detachment.
Direct physical impact. A blow to the knee, caused by a fall or other circumstance, is as common as a jump, but can also result in serious damage and ligament detachment.
tendonitis
Tendinitis, an inflammation of the tendon tissue that leads to degeneration and weakening of the tendon, is considered one of the most common causes of minor (partial) tears.
General weakness of the tendon ligament
The possibility of inner ligament rupture is directly proportional to the degree of ligament weakness for the following reasons
- disorders of metabolism;
- Rheumatoid arthritis;
- diabetes mellitus;
- kidney failure;
- taking certain types of medication (eg, steroids);
- lupus, etc.
diagnosis of the injury
In order to diagnose the presence of a ligament injury and determine a treatment strategy, the specialist will obtain information about the cause of the injury and the current condition of the patient, and conduct a visual examination.

Fig. 3: A knee extension/torsion test can provide important information about the type of tendon injury.
Diagnosis by X-ray examination
Visual diagnosis of the nature of the injury requires more accurate confirmation, which can be obtained by MRI and/or X-rays.
X-ray examination. If the ligament is partially or completely torn, the kneecap will be displaced upwards.
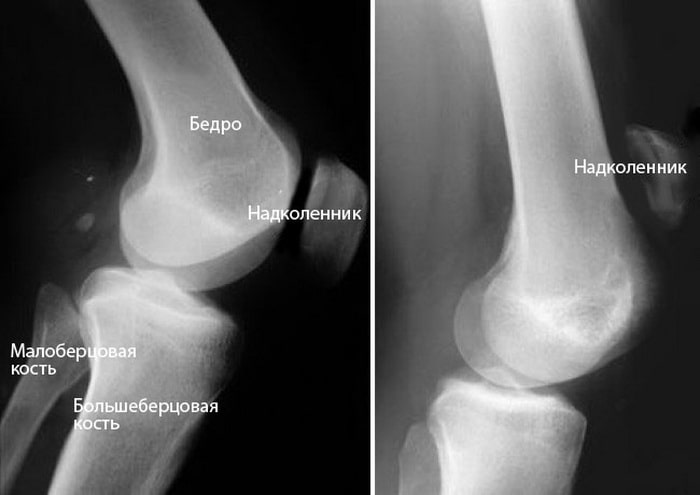
Fig. 4: (Left) Lateral projection showing the normal position of the patella. (Right) Upward displacement of the ligament when torn.
MRI. During the MRI scan, the examiner can not only look at the soft tissues around the knee, but also determine the location and severity (extent) of the tear.
diagnosis
The first medical examination immediately after the injury usually gives a very good indication of which ligaments were damaged. When examining the joint area, the doctor looks for soft tissue swelling or bleeding and gently palpates the knee to locate the area of most pain.
The doctor may also perform specific stress tests to assess the degree of mobility in the lower extremity relative to the thigh. Stress tests for ligament injuries often provide valuable information. When the knee is loaded, the joint space on the side of the injury increases, indicating that the affected ligaments are not functioning properly. Ligament injuries can be partial or complete.

With a partial ligament injury, the joint space is less open and the joint instability is not pronounced. Performing stress testing in the acute phase of the injury usually causes pain in the projection of the damaged collateral ligament.
A few hours after the injury, a ligament injury is more difficult to diagnose due to swelling and muscle spasms. In such cases, the knee joint should be re-examined after a few days, when the pain and swelling have subsided. Between examinations, the joint should be protected with an orthosis, the limb elevated and anti-inflammatory medication taken.
If hemarthrosis is detected in the joint, aspiration (removal) of blood from the joint is required.

Blood in the joint with a mixture of fat is a sign of bone or cartilage damage.
A radiological examination is mandatory to rule out bone damage. Occasionally stress tests are performed and the width of the joint opening can be documented with X-rays.
Conservative treatment
Isolated injuries to the inner and outer collateral ligaments require surgical reconstruction. Partial ligament injuries in the knee (grades 1 and 2) usually do not result in joint instability and are usually treated conservatively to reduce pain and swelling and limit limb movement (use of a splint).
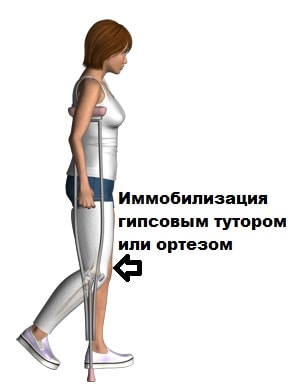
An orthosis is usually used for up to 4 weeks. When the pain subsides, the limb is allowed to be carried, and crutches are preferably used for locomotion.
surgical treatment
Most isolated collateral ligament injuries of the knee can be treated conservatively. Surgery may also be indicated when the collateral ligament damage is so severe that it is unlikely to heal on its own, or when it is combined with injuries to other parts of the knee joint.
In all cases, an endoscopic examination is carried out during the operation in order to identify and treat any damage to the articular cartilage, cruciate ligaments and meniscus.
Special anchors or interference screws are required for the anatomical reconstruction of the collateral ligaments from bone.
The anchor is placed at the site of the collateral ligament tear during surgery. The seams of the side band are sewn together with anchor sutures. Once the sutures are knotted, the tape is pulled to the bone where the tear occurs.
The best treatment for long-term collateral ligament injuries is anatomical reconstruction. In reconstruction, the damaged collateral ligament is replaced with a graft from another tendon taken from the patient.
In our clinic we use arthroscopy and other minimally invasive methods to treat knee joint pathologies. The operations are performed on state-of-the-art medical equipment with high-quality and proven consumables and implants from the world's largest manufacturers.
However, the result of the operation depends not only on the devices and the quality of the implants, but also on the skills and experience of the surgeon. The specialists in our clinic have many years of experience in treating injuries and diseases in this place.
Video about our clinic for traumatology and orthopedics
- Analysis of the anamnesis and the complaints
- Clinical examination
- Diagnosis of the symptoms
- Examination and interpretation of MRI, CT and X-ray images as well as blood analyses
- diagnosis
- prescription of treatment
Duration of the operation and recovery period:
The operation is performed under short-term anesthesia. The operation takes about 45 minutes. 2-3 days stay in the hospital. 6 weeks on crutches and with a splint. Cycling after 2 months. Ban on running and jumping for 3 months.
The results after the operation are good to very good, and the full function of the joint is usually restored. As after any operation, infections or thrombosis are possible. Unlikely complications: re-tearing or limited mobility.
Comments and explanations:
Rehabilitation is very important. A follow-up examination by the surgeon and a two-week rehabilitation program are recommended 6 to 8 weeks after the operation.

Chronic lateral (external) instability of the kneecap is the cause of limited mobility in quite a few patients. Chronic instability of the kneecap, also known as habitual dislocation of the kneecap, generally affects patients, especially young and middle-aged women, and leads to a significant reduction in quality of life. Chronic lateral patellar instability is of critical importance in active sports when the patella, an important part of the knee's extensor system, is unstable and pain-free.

Chronic instability of the patella is usually caused by inadequate diagnosis of the primary lateral (external) patellar dislocation and subsequent inadequate treatment. The importance of diagnosing a primary or acute external dislocation of the kneecap cannot be overstated. The doctor must not only analyze the mechanism and circumstances of the injury, but also consider the patient's normal anatomy, because in some cases conservative treatment is completely futile and surgical intervention is required.
Symptoms of a tear of the medial collateral ligament in the knee joint

When the medial collateral ligament of the knee joint is torn, there is usually a 'click' sensation, a sharp pain in the interior of the knee joint. Shortly after the injury, the inner part of the knee joint is visibly swollen.
Initial treatment for suspected medial collateral ligament injury is immobilisation of the knee joint, reduction of axial loading on the injured lower extremity, elevation, and cooling.
After a detailed questioning about the mechanism of injury, the orthopedist must examine the area around the injured knee joint and compare the degree of external deviation of the lower limb with the uninjured limb (so-called valgus stress test). When palpating a medial collateral ligament injury, a stabbing pain becomes noticeable, bending and stretching the knee joint is usually possible, but painful.
If a medial collateral ligament injury is suspected, it should be borne in mind that while isolated collateral ligament injuries do occur, medial meniscus tears and anterior cruciate ligament injuries are more common due to the common mechanism of injury.
Treatment of a medial collateral ligament tear

To confirm a medial collateral ligament tear and to diagnose other knee joint injuries, a competent orthopedic trauma surgeon will order two standard x-rays and recommend magnetic resonance imaging (MRI) of the knee joint.
If only the medial collateral ligament of the knee joint is damaged, the trauma surgeon will recommend conservative treatment. This consists of immobilising the knee joint in a comfortable straight orthosis that prevents flexion and extension of the knee joint. The doctor will also prescribe elastic bandages or compression knitwear, as well as special drugs to prevent blood clots in the veins. This is crucial, since any injury to the lower limbs can trigger deep vein thrombosis, so regular follow-up visits to the doctor and strict adherence to recommendations are essential. In the care of a competent and experienced orthopedist and traumatologist, healing of the medial collateral ligament takes 3 to 4 weeks, depending on the extent of the original injury. Once immobilization is restored and vigorous movement is begun, the patient is first recommended to wear a stabilizing patella to prevent re-injury of the medial collateral ligament.
Conservative treatment

diagnosis
Diagnosing a meniscus tear in the acute phase is difficult in the absence of a blockage. The absence of characteristic symptoms means that patients are often diagnosed with a sprain or contusion of the knee joint. The diagnosis is most meaningful in the subacute phase (2-3 weeks after the injury), when the nonspecific symptoms of the injury are less pronounced. At this stage, the traumatologist can diagnose a meniscus tear based on local pain and infiltration in the area of the joint space, specific pain tests (mediolateral test, compression symptoms, stretch symptoms (Landa, Baykov, Roche) and rotation symptoms) and MRI data of the knee.

Treatment of meniscus injuries
In the acute phase, if the joint is blocked, the blockage is removed under local anesthesia; if fluid accumulates (hemarthrosis or joint effusion), a joint puncture is performed. A plaster cast is then placed on the knee joint, which is bent in half, for three weeks. The patient then undergoes exercise and physical therapy.
Surgical intervention is indicated when the blockage cannot be removed in the acute phase, the blockage recurs and the joint shows pain and restricted movement in the chronic phase. Arthroscopic procedures are currently the preferred surgical treatment to reduce trauma to the joint and the risk of complications. The meniscus should be preserved whenever possible, since its removal accelerates wear on the articular surfaces, leading to the rapid development of osteoarthritis.
1 Meniscus Injury of the Knee: Clinical Guidelines/ All-Russian Public Organization Association of Traumatologists and Orthopedists of Russia (ATOR) – 2013.
2 Surgical treatment of patients with meniscus damage in the knee joints: from removal to transplantation (literature review)/ Klyukvin IY, Filippov OP, Slastinin VV // Transplantology – 2013 – № 3.
3. Diagnosis and treatment of meniscal injuries in knee joint trauma : abstract of the dissertation / Filippov, OP. – 2014
Read more:- Collateral ligament rupture.
- Femoral collateral ligament.
- Rupture of the ligaments of the ankle.
- The lateral dislocation is.
- tibial ligaments.
- Axis of rotation of the knee joint.
- Rupture of the radial-clavicular joint.
- Treatment of torn ligaments in the ankle.
