A grade 1 rupture does not require strong immobilization of the limb. Patients are recommended to wear elastic bandages during the day. These products only slightly restrict mobility and prevent excessive strain on the ankle joint.

- Ankle ligament injuries
- Conservative treatment
- Sprained or torn ligaments: how to recognize them?
- What does the clinical picture look like?
- symptoms of pathology
- Stages of development
- symptoms
- diagnosis
- Physiotherapeutic treatment
- Therapeutic exercises and gymnastics
- Diagnosis of the problems
- How do you give first aid to an injured person?
- REAR ANKLE LIGAMENTS: WHO IS AT RISK?
- WHAT A TORN ANKLE LIGAMENT LOOKS LIKE
- 1ST STAGE
- 2 STAGE.
- 3 DECISION
- Massage for chronic injuries
- massage
- AdobeStock_220819137-1.jpg
- AdobeStock_288966178-1.jpg
- How does this work?
Ankle ligament injuries
Ankle ligament injuries are one of the most common injuries. They are the main reason why patients present to an orthopedic trauma surgeon. Ankle sprains account for up to 35 percent of sports injuries. These injuries can usually be treated conservatively and well.
However, some patients, especially those who exercise or do physical work, may experience pain and swelling despite treatment. In addition, this group of patients may experience a feeling of instability in the ankle joint. The instability or instability of the joint is manifested by recurrent dislocations of the foot, in the patient's expectation and fear of recurrent dislocations of the ankle joint.
This article explains in detail the anatomy of the ankle ligaments, how and why they can become damaged, and what methods are available to diagnose and treat ankle instability, both conservative and surgical.
The ankle is the joint that transfers load from the trunk to the foot. This joint is formed by the tibia, fibula and talus.

A normal, healthy ankle is an extremely stable joint. Its stability is ensured by strong ligaments that run along the inner and outer surfaces of the joint. The ligaments connect the shinbone and the foot bones. The ligaments on the outside of the joint (talar, fibula, and calcaneus ligaments) are the most commonly damaged ligaments.
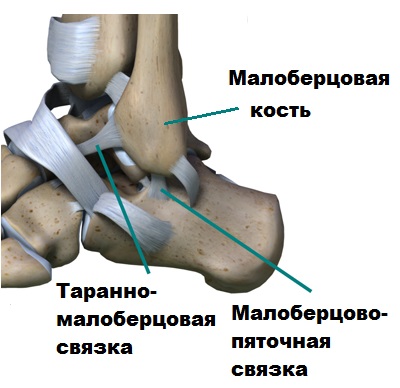
When the foot is rotated inward, the anterior talocrural and calcaneofemoral ligaments are primarily damaged. If patients with the above injuries were inadequately treated or did not see a doctor at all, the ligaments may not heal or heal only with stretching.
Conservative treatment
Most recent ankle ligament tears and sprains can be treated conservatively.
Conservative treatment usually consists of stabilizing the ankle for several weeks with an orthosis, active physiotherapy and physical therapy.

However, statistically we know that a third of all patients develop chronic ankle instability despite treatment.
This instability is often poorly tolerated by patients, affects professional and sporting activities and requires the constant wearing of an orthosis.
Prolonged ankle instability and repeated subluxations associated with ligament insufficiency are indications for surgery.

Sprained or torn ligaments: how to recognize them?
The ligaments of the joint are a bundle of various connective tissue fibers. They serve to connect the bony elements of the joint, strengthen it and limit the range of motion of the joint.
The most common types of ligament injuries are tears and sprains. How do ligaments tear or stretch? How to tell if a ligament is torn or stretched after a joint injury?
A ligament strain is a pathological condition characterized by the tearing of individual fibers of the ligament, but in which the anatomical continuity of the organ is preserved. The causes of this condition can be different. It occurs with sudden and violent movements that are not specific to the joint.
A ligament tear is a traumatic condition resulting from a complete rupture of the integrity of the ligament due to transverse severing of the connective tissue fibers. The causes of a ligament tear are the same as a sprain, but the force exerted on the joint is much greater.
The difference between a torn ligament and a sprain is not obvious at first glance. There is no clear difference between these pathological conditions. In both cases the integrity of the fibers is compromised. However, there is one exception: a sprain is a partial injury and a tear is a complete injury.
What does the clinical picture look like?
Specialists distinguish three main degrees of severity of articular ligament injuries, the variations of which determine the features of the clinical picture of the pathological condition:
- Grade I, ie mild damage, consists of minimal individual fiber tears with the development of a small tissue lesion. The condition is characterized by moderate pain and the ability to move the joint. A mild ligament rupture does not cause a hematoma.
- Grade II (moderately severe) or so-called incomplete ligament rupture. In practice, the injury is manifested by a severe pain syndrome in the injured joint, pronounced swelling of the soft tissues and a sudden restriction of movement.
- Grade III, the severe rupture, is a complete separation of the fibrous elements, characterized by acute, severe pain, severe swelling of the injured joint, bleeding with hematoma formation, and impaired motor function. The joint has a characteristic clicking and pain, as well as abnormal mobility or instability during movement.
The symptoms of these injuries can vary from patient to patient depending on their body type. With a severe sprain or complete tear, some people's mobility is severely limited, while others can move despite pain. This depends on the individual pain threshold, training and fitness.
symptoms of pathology
Classic symptoms of damage to the ligaments that connect the bones in the joint include:
- Pain when moving that does not stop even when at rest
- Swelling of the damaged area
- Extensive hematomas on the second day after injury
- Limitation of range of motion and mobility, with possible joint instability if completely interrupted
- Numbness or tingling
- Crunching or clicking in the joint when moving
What to do after a ligament injury? First, apply ice to the injury site to reduce swelling and bruising and take a pain reliever. Do not hesitate to visit your doctor and undergo a diagnosis.
Stages of development
Depending on which joint ligament is injured, there are three stages of damage:
The first stage, sprain, is characterized by maintaining overall integrity but tearing a portion of the ligament fibers.
Second degree or tear – the mechanical integrity of the band is partially damaged.
A third-degree ligament tear or a complete tear is associated with instability of the joint.
The first diagnosis is made during the examination. In order to fully assess the extent of the injury, diagnostics must be carried out.
symptoms
The patient complains of pain. The injury site is swollen and the joint contour is flattened. In a partial rupture, there is mild to moderate swelling; in a complete rupture, the swelling is significant and often affects adjacent anatomical segments. The extent of edema depends not only on the severity of the injury, but also on the age of the injury. Sprains or lacerations that have not healed (more than a day old) can be associated with greater edema than fresh, complete wounds. Complete wounds almost always have bruising to the skin.
The degree of support and limitation of movement also depends on the severity of the injury, ranging from mild difficulty in sprains to inability to support the leg in complete ruptures. Palpation of the ligament is painful. Crepitations are not present. Abnormal stiffness of the joint (e.g., lack of normal lateral movement or excessive forward and backward movement of the knee) is also seen in larger tears and injuries.
diagnosis
Ligament tears are often clinically very similar to periarticular or intraarticular fractures, so in all of these cases X-rays are taken to rule out bone damage. When ligaments are torn near the base of the ligament, x-rays sometimes show a loose, thin bone plate - a fragment that has come off with the ligament. A CT scan of the joint is recommended to rule out minor damage to the dense structures of the joint, while an MRI scan of the joint is used to assess the extent of ligamentous damage. In some cases, arthroscopy is used for diagnosis and treatment.
The shoulder joint is an extremely active joint with many different movements. A large number of ligaments are attached to this joint. Depending on the location, possible injuries include injuries to the cruciate ligament (ACL), injuries to the sternoclavicular ligament, injuries to the tendons of the short and long heads of the biceps, and injuries to the rotator cuff of the shoulder, which are formed by the tendons of the supraspinatus, subscapularis, scapularis and obturator minor becomes.
The ligaments of the shoulder joint can be torn as a result of an outward rotation of the arm, a fall on the outstretched arm, a blow to the collarbone, or a sudden extension of the arm during a throw. The joint is swollen, deformed and smoothed. Bruising may occur. Mobility is restricted. If the biceps tendon is torn, the biceps brachii shortens when you try to bend your arm. Shoulder ligament injuries can be complete or incomplete, with symptoms being more pronounced with a complete tear.
The diagnosis is made based on the clinical picture and x-rays of the shoulder joint, which show no bony damage. Magnetic resonance imaging of the shoulder joint is indicated if labral injury and complete rupture of other ligaments are suspected. In some cases, arthrography and ultrasound are also used. If the location and extent of the injury cannot be determined using the above-mentioned examinations, the patient is referred for shoulder arthroscopy, which can be used both as a diagnostic and therapeutic procedure (suturing the defect).
Physiotherapeutic treatment
Physiotherapy treatments are always recommended when treating ankle injuries. Their therapeutic effect is no less effective than that of pharmacological treatment. For grade 1 and 2 ligament injuries, physiotherapeutic treatments are also recommended on the 3rd and 4th days of treatment. After surgical procedures, on the other hand, they are carried out during the rehabilitation phase. The choice of physiotherapy is made by the traumatologist individually for each patient. He or she takes into account:
Electrophoresis is used in the initial phase of treatment. A sterile gauze pad soaked in a solution is placed on the injured area and metal plates are placed on top. Under the influence of electrical impulses, the drug molecules penetrate into the deepest tissues. During the procedure, glucocorticosteroids, painkillers and non-steroidal anti-inflammatory drugs are used. Chondroprotective solutions are prescribed to promote healing of ligaments that have separated from the base of the bone.
In addition to electrophoresis, the following physiotherapy treatments can also be carried out during rehabilitation
- Ultrasound therapy. It serves to improve microcirculation in damaged tissue and increase lymphatic drainage. This is followed by more complete absorption of medications – ointments, gels, lotions. The drugs are better absorbed and distributed throughout the ligaments and tendons;
- UHF therapy. Accelerates the repair processes, stops the inflammatory process. And by dilating blood vessels, it improves metabolism;
- Paraffin therapy. Physiotherapy helps to quickly eliminate severe swelling and even stubborn, extensive hematomas. The improved microcirculation increases the supply of oxygen, nutrients and bioactive substances to the damaged tissue.
Magnetic therapy is an essential physiotherapeutic measure for ankle injuries. After it, blood and lymphatic drainage improves and inflammation is reduced. A more complete absorption of drugs from ointments and gels was also observed.
Therapeutic exercises and gymnastics
Therapeutic exercises are recommended to patients to improve the function of the ligament-tendon apparatus. The exercises begin with light warm-up exercises. They gradually become more and more difficult. The general rule for therapeutic exercise is that you should not feel pain of any intensity. The exercises should be done in moderation:
Patients are recommended to walk on their toes and then on their heels several times a day. Rehabilitation therapists recommend flexing and extending the foot and performing circular rotations to achieve rapid recovery.
| treatment methods. | Medication, physiotherapy, exercises |
| Pharmacological drugs | Systemic NSAIDs (Celecoxib, Diclofenac, Ketorolac), topical NSAIDs (Fastum, Voltaren, Ketorol, Arthrozilen), chondroprotectors (Dona, Alflutop, Structum, Tereflex), Venotone (Troxevasin, Lyoton, Heparin ointment), drugs to improve blood circulation (Detralex, Venarus, Flebodia). |
| Physiotherapeutic treatments. | UHF therapy, electrophoresis, paraffin therapy, ultrasound therapy, magnet therapy. |
| Surgical interventions | tendon and bone sutures |
| Therapeutic exercises and gymnastics | Walking on tiptoes, walking on heels, picking up small objects from the floor with your toes, rolling bottles with your feet. |
Damage to the ankle ligaments can cause serious health problems in the early stages if left untreated. Within a few months, complications such as flat feet, habitual sprains, arthritis and arthrosis develop. That's why it's important to see a doctor as soon as possible after an injury. A well-conducted examination and competent treatment of torn ligaments can avoid irreversible consequences.
Diagnosis of the problems
The diagnosis is made based on the external examination of the patient, his complaints and instrumental findings. The most informative x-ray images are the direct and lateral projections. They can be used to distinguish between a torn ligament and a broken joint or long bone.
An experienced diagnostician can determine the nature of the injury after analyzing the results of ultrasound examination, although it is considered an additional examination method. The ultrasound shows the extent and location of inflammatory swelling and bleeding in the joint cavity.
MRI is usually indicated in patients preparing for surgery. The examination makes it possible to image the surgical field, assess the extent of the rupture and rule out damage to the bony and cartilaginous structures of the ankle joint.
How do you give first aid to an injured person?
First aid affects the speed and intensity of ankle recovery, as well as the nature of symptoms. The person is placed on a firm surface, covered with a thin blanket or bandage, and kept calm. The injured joint is completely protected and the leg is fixed in a slightly elevated position with a splint or bandage.
Cold compresses are then used to cool the area to reduce the intensity of the pain. A plastic bag filled with ice cubes is placed on the ankle for 10 minutes every half hour. A piece of frozen meat, mixed vegetables or a towel soaked in cold water are also suitable. Cold compresses not only have a pain-relieving effect, but also prevent inflammatory swelling caused by the narrowing of small blood vessels.
The injured person is given a tablet containing a non-steroidal anti-inflammatory drug (NSAID). These include Diclofenac, Naiz (nimesulide), and Ketorol (ketorolac). If these drugs are not present in the home medicine cabinet, paracetamol is used. These medications provide pain relief until the emergency services arrive.

REAR ANKLE LIGAMENTS: WHO IS AT RISK?
A sprained ankle can occur at any age. Sometimes it literally happens 'surprisingly': a walk, a stumble and it's done: an attack of pain from torn ligaments in the ankle and the inability to step on the foot. However, there are people who are particularly vulnerable to injury:
- competitive athlete.
- Lovers of ski resorts, inline skating, ice skating, etc.
- Gardeners Armed with Shovels: Digging the soil in the spring puts a lot of unusual strain on the ankle.
- Patients with abnormal feet: valgus foot, flat foot, etc.
- Patients with diseases of the musculoskeletal system: scoliosis, posture and gait disorders.
- Patients with obesity.
- People with congenital diseases in which the connective tissue is particularly elastic (Marfan syndrome, Ehlers-Danlos syndrome, etc.).
WHAT A TORN ANKLE LIGAMENT LOOKS LIKE
1ST STAGE
Elongation of a small part of the fibers.
- Discomfort when walking or running quickly. No pain at rest.
- Slight swelling over the lesion and on the forefoot.
2 STAGE.
Partial tear – significant fiber damage.
- Sharp pain with every step and at rest, especially on waking.
- Significant swelling that is noticeable when putting on shoes (the painful foot is larger than the healthy foot).
3 DECISION
Torn ligaments with extensive trauma to the ankle joint.
The symptoms of a torn ligament are particularly severe:
- Inability to put weight on the foot due to pain;
- swelling of the entire joint, the redness may reach the middle of the shin;
- Hematoma over the injured ligament.
If these symptoms appear, consult a doctor immediately!
Massage for chronic injuries
Up to 50 percent of patients who suffer an ankle injury do not seek medical attention or receive appropriate treatment afterwards. This is associated with a high rate of poor treatment outcomes. Thirty percent of patients experience long-term consequences after an ankle injury. This can in particular be a case of chronic instability of the ankle joint.
For long-term injuries, massage alone is probably not sufficient. If instability has developed, it can in some cases be treated with external fixation devices within the first two months. If the injury is more extensive, surgical intervention must be carried out. These are divided into 3 groups:
massage

massage
- Local tissue repair of the torn ligament;
- repair with allografts (preserved donor tissue);
- Replacement of plastics with synthetic prostheses.
If the injury occurred a long time ago but the leg still hurts, swells or tips when exerted, you should see a doctor. There may be a complete ligament tear that has not yet been diagnosed and treated. If the diagnosis shows that healing is possible using conservative methods, massage is used along with other treatments: physiotherapy, physiotherapy, ozone therapy and other methods to relieve pain and improve blood circulation.
AdobeStock_220819137-1.jpg

AdobeStock_220819137-1.jpg
When 'crosses' are torn, in the vast majority of cases they cannot be healed without surgery. The ligaments do not heal by themselves. Walking with a torn ligament is forbidden: it leads to dystrophy of the joint, muscle wasting and can lead to chronic pain.
There are only two situations in which surgery is not possible:
- Partial tear of the cruciate ligament (i.e. If only part of the fiber is damaged, this type of injury is also called a sprain);
- Medical contraindications to surgery.
In the initial period after the injury, the joint is swollen and the pain is severe. For this reason, it is clinically impossible to determine whether the ligaments are completely torn. A proper examination is only possible once the hematoma is removed and the knee is anesthetized. For this purpose, a puncture is performed. The joint cavity is flushed out. After blood and clots are removed, anesthesia is given with a local anesthetic solution. A procaine solution of 0.5 % or 1 % can be used, injected in 25-30 ml.
An instrumental examination is always required. It's likely that more than just the tapes were damaged. The doctor will at least take an x-ray. This allows the exclusion of burst fractures (when a bone fragment breaks off at the point of attachment of the ligament) as well as damage to the femoral and tibial condyles.
After the necessary therapeutic and diagnostic procedures, the extremity is immobilized. A plaster cast is applied for 2 months. Large swelling usually occurs in the first week. This leads to an increase in the volume of the limb. The limb is always swollen when the cast is applied. When the swelling goes down, the bandage is loosened. It should be changed after 5-7 days.
Then the recovery process begins. Painkillers, exercise therapy and physiotherapy are used. Static exercises for the thigh muscles are recommended to the patient. Intra-articular injections of hyaluronic acid and platelet-rich plasma can be used to accelerate regeneration processes and prevent dystrophic changes in the cartilage in the knee joint.
AdobeStock_288966178-1.jpg

AdobeStock_288966178-1.jpg
Conservative treatment is sometimes the mainstay of treatment for patients with knee injuries. This doesn't just apply to sprained ligaments. In some patients, surgery is contraindicated. Others simply refuse to have them done. The reasons for this are different: fear of surgery, the misconception that ligaments can be closed without surgery, underestimation of the impact of the injury, etc. In any case, you cannot force a person who refuses surgery. But you can help in any way you can. There are methods that can speed up the patient's recovery. However, if the ligament structures are completely torn, they cannot eliminate the instability of the knee joint.
Art therapy is one of the most effective treatment methods. This technique involves injecting two medications into the knee:
1. Hyaluronic acid. This is a 'lubricant' for the joint. It softens the friction of the joint surfaces, relieves pain and slows down degenerative processes in the cartilage tissue. Destruction of cartilage is almost inevitable in patients in whom surgical ligament repair was required but not performed. Hyaluronic acid can be used to delay the onset of osteoarthritis and reduce its severity.
2) Platelet-rich plasma. If the patient buys hyaluronate at the pharmacy, he does not need to purchase a second preparation for arthrotomy. It is made from the patient's blood right before it is injected into the knee. To do this, the doctor takes blood from the elbow vein. The blood cells are removed so that only the platelets remain. By removing the fluid, its concentration is many times higher than in the blood. This plasma is injected into the knee.
How does this work?
Platelets are responsible for forming a blood clot. Any injury is accompanied by the formation of a blood clot. Its main function is to close the injured site, stop bleeding and isolate the injury site from pathogenic bacteria and other harmful factors. In addition, the platelets contained in the clot must ensure that the wound heals. They secrete growth factors that stimulate regenerative processes. We use a similar mechanism in the conservative treatment of knee injuries. Injection of platelet-rich plasma into the joint stimulates repair of the intra-articular structures.
Read more:- Injury to the ligaments of the ankle.
- Damaged ligaments of the ankle.
- Partial tear of the ligaments of the ankle.
- Treatment of torn ligaments in the ankle.
- Damaged ligaments of the ankle photo.
- ligaments in the ankle.
- Rupture of the medial collateral ligament.
- dislocation of the ankle.
